The skin microbiome is the term used to describe the totality of all microorganisms on our skin. The microbiome of healthy skin is characterized by a great diversity of different species of bacteria, fungi and viruses. The composition of the skin microbiome differs significantly between different regions of a person’s skin. The skin microbiome likely plays an important role in the development and progression of inflammatory skin diseases, such as atopic dermatitis.
The healthy human body is an ecosystem populated by various microorganisms. Current estimates suggest that we are made up of about the same number of bacterial cells as human cells. The totality of these microorganisms in our body is called the microbiome. Depending on the organ system observed, a distinction is made, for example, between the gut microbiome and the vaginal microbiome, the respiratory microbiome or the skin microbiome. In the following article, we would like to look at the skin microbiome and its importance in the development of skin diseases. After all, the skin is our largest organ and forms an important interface with our environment.
New analytical methods have enabled research into the skin microbiome
Research on the skin microbiome has become increasingly important in recent years. Research into the complex skin microbiome has been made possible by the widespread availability of new molecular biological analysis methods. First and foremost is next-generation sequencing (NGS). It is only since the introduction of NGS that the entire DNA in a skin sample can be analyzed and taxonomically assigned to different genera and species. This allowed the actual and complex picture of the skin microbiome to be presented for the first time. This is a decisive advantage over conventional methods such as cultivation, with which only selected and, above all, easily cultivatable microorganisms, such as the bacterium Staphylococcus aureus and investigate them. A working group at the U.S. National Institute of Health in Bethesda, MD, led the way in introducing NGS into skin microbiome research. This research group succeeded for the first time in displaying the entire spectrum of bacteria and fungi as if on a map of the skin. For the bacterial skin microbiome, it was shown that seborrheic body regions are dominated by propionibacteria, while corynebacteria predominate in intertriginous regions and proteobacteria on dry skin areas [1]. Among fungi, the yeast Malassezia spp. dominates on most of the examined body sites, although the composition of individual Malassezia species varies considerably between body sites [2].
The skin microbiome is diverse and region specific
According to the research results to date, the microbiome of healthy skin can be defined according to two principles. First, the microbiome of healthy skin is characterized by a particular diversity of different microbial species. Conversely, limited diversity of the skin microbiome is measurable in skin diseases such as atopic eczema. Thus, during relapses of atopic eczema, S. aureus proliferates at the affected skin sites and displaces other bacterial species. However, it still remains unclear whether this proliferation of S. aureus is the cause or rather consequence of the eczema flare [3]. When eczema heals, the diversity of the skin microbiome returns to that of healthy skin. As a second principle of healthy skin, the composition of the skin microbiome has been shown to be typical of each skin region within an individual. Thus, the skin microbiome at the crook of the elbow is dominated by different microorganisms than at the cheek. Interestingly, these differences between individual skin regions are much more pronounced than the differences of a particular skin region between two individuals. In short, the skin microbiome of your elbow is much more similar to the skin microbiome of my elbow than to the skin microbiome of your own cheek. There is only speculation about what factors influence the composition of the microbiome on specific skin sites. The skin pH, the lipid content of the skin or the surface temperature could play a role. We do not know exactly.
The skin microbiome is important for the development of skin diseases
From what we know so far, the skin microbiome is essential for the homeostasis of our skin. Colonization of our skin with commensals, beneficial microorganisms, seems to protect against colonization of the skin with pathogenic microorganisms. This can be explained, at least in part, by the production of antimicrobial peptides by commensal bacteria such as Streptococcus epidermidis. These antimicrobial peptides are effective against pathogenic bacteria such as S. aureus and prevent their growth. The role of the skin microbiome in the development and progression of inflammatory skin diseases is under intense investigation. As an example, the yeast Malassezia spp. deserves detailed discussion because it is not only the most common fungus on healthy skin, but also associated with various skin diseases. He thus challenges the classical microbiome paradigm of commensal versus pathogenic microorganisms.
The yeast Malassezia spp. plays a role in atopic dermatitis
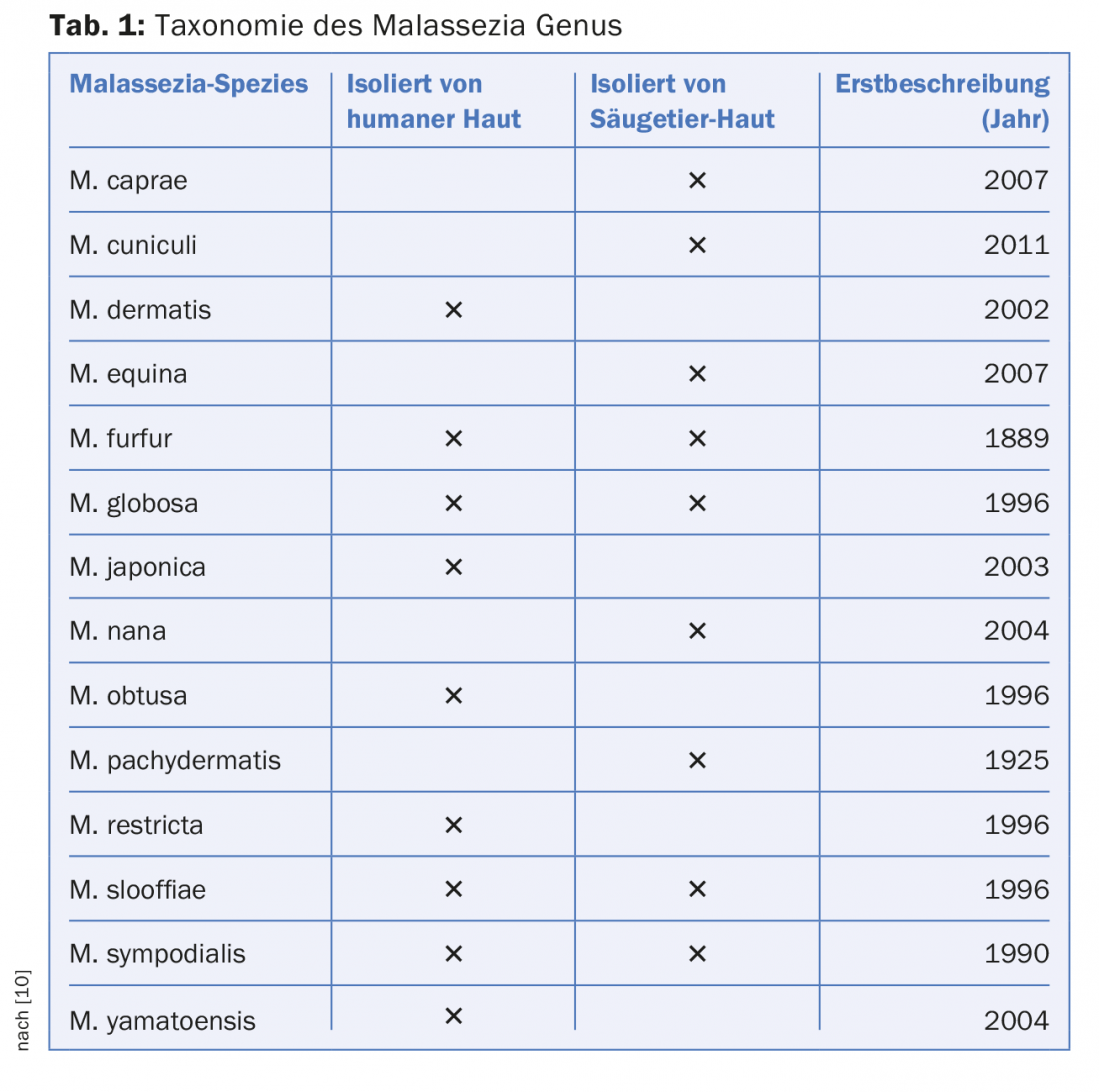
The yeast Malassezia spp. is part of the healthy skin microbiome of humans and mammals [4]. The genus currently comprises 14 species, nine of which are frequently detected on human skin (Tab. 1). These Malassezia species lack their own enzymes for the synthesis of important lipids, which is why Malassezia spp. are found in particular density on seborrheic skin areas such as the head, neck and upper trunk. Thus, although Malassezia spp. is a classic commensal, it appears to be associated with common skin diseases; e.g., pityriasis versicolor, seborrheic eczema, and atopic dermatitis. In the following, we will take a closer look at the role of Malassezia spp. in atopic dermatitis (AD).
AD is a chronic inflammatory skin disease characterized by recurrent, highly pruritic eczema [5]. The prevalence of AD in developed countries has tripled in the last 30 years. Here, 15-30% of children and up to 10% of adults are affected. Despite its epidemiological and health economic importance, the pathogenesis of AD is not yet fully understood. In any case, the skin of patients with AD is characterized by impaired barrier function and altered immune system compared to skin healthy individuals [5]. These two factors appear to influence the skin microbiome. Indeed, previous studies have supported the pathogenetic role of the otherwise commensal Malassezia spp. in AD. Thus, it is striking that more than 50% of all adult patients with AD are sensitized to Malassezia spp. Thus, they either show a positive skin prick test or have Malassezia spp.-specific IgE antibodies in the serum. In comparison, skin healthy individuals are usually not sensitized to Malassezia spp. although they are also regularly colonized with this commensal [6]. Furthermore, the serum titer of Malassezia spp.-specific IgE antibodies correlates with the severity of atopic eczema in adults [7]. The pathogenetic mechanisms behind this sensitization have been at least partially elucidated.
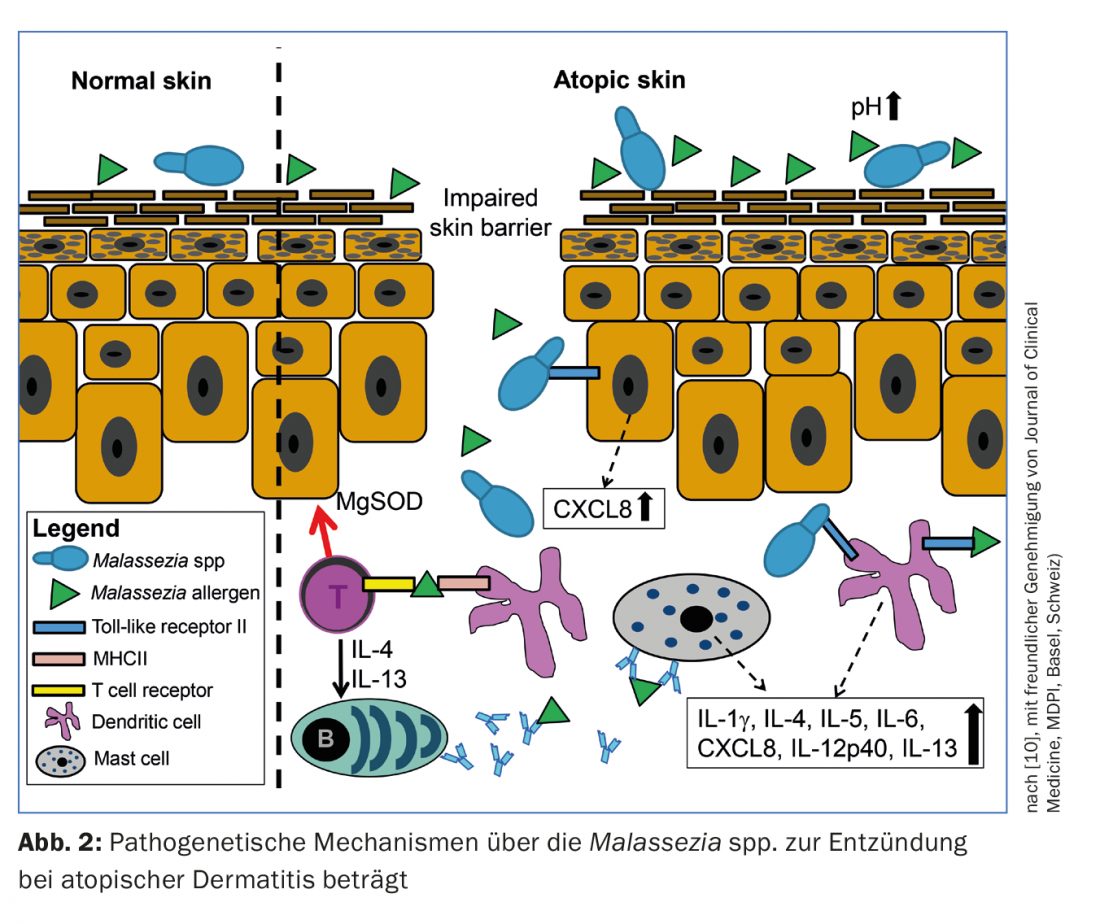
Sensitization occurs via yeast immunogenic proteins (or allergens), which penetrate through the skin barrier typically disrupted in AD into deeper skin layers, such as the lower epidermis and dermis, where they are recognized by dendritic cells. This recognition leads to the activation of T and B lymphocytes and eventually to the production of Malassezia spp.-specific IgE antibodies.
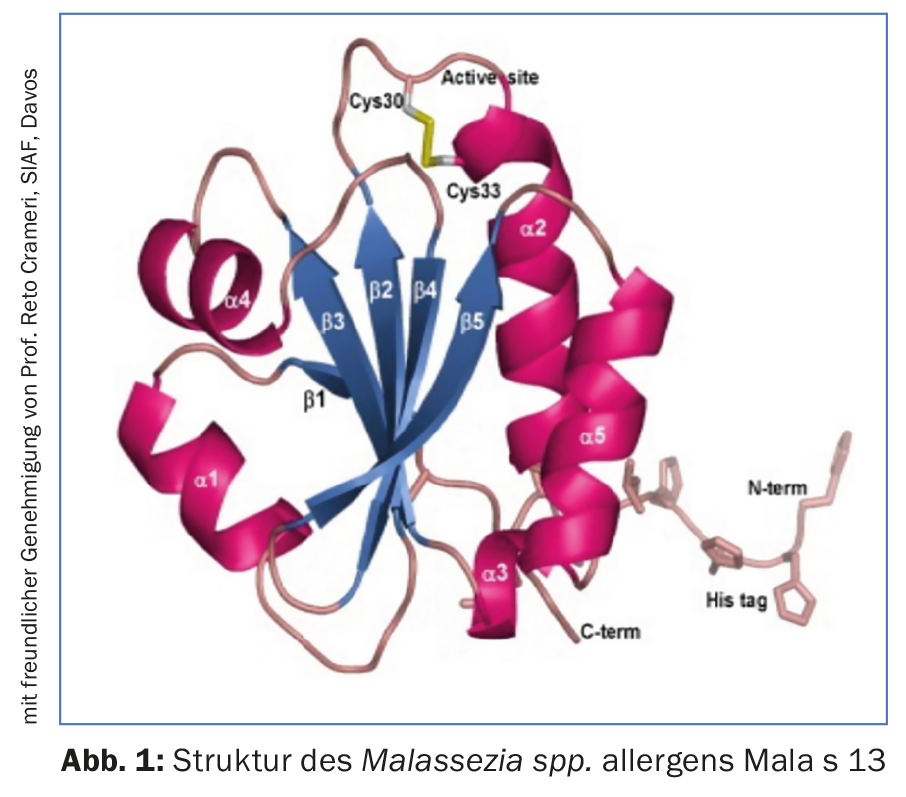
So far, 14 allergens have been identified by Malassezia spp. identified that initiate such IgE antibody production. (Fig. 1, Tab. 2). Already some time ago it could be proved that Malassezia spp. produce and secrete more allergens in an almost pH-neutral environment, which is characteristic of the skin of patients with AD, than in an acidic pH corresponding to healthy skin [8]. However, some allergens not only lead to the production of IgE, but can directly cause eczema on the skin. For example, the allergen Mala s 11, a manganese superoxide dismutase from the species Malassezia sympodialis, has a 50% homologous amino acid sequence with human manganese superoxide dismutase in keratinocytes of the skin [9]. Sensitization to Mala s 11 can therefore induce autoreactive T lymphocytes directed against both the fungal and the very similar human enzyme in keratinocytes. Clinical trials have shown that application of Mala s 11 to the skin of patients with AD probably does indeed lead to eczema via this T-cell-mediated mechanism.
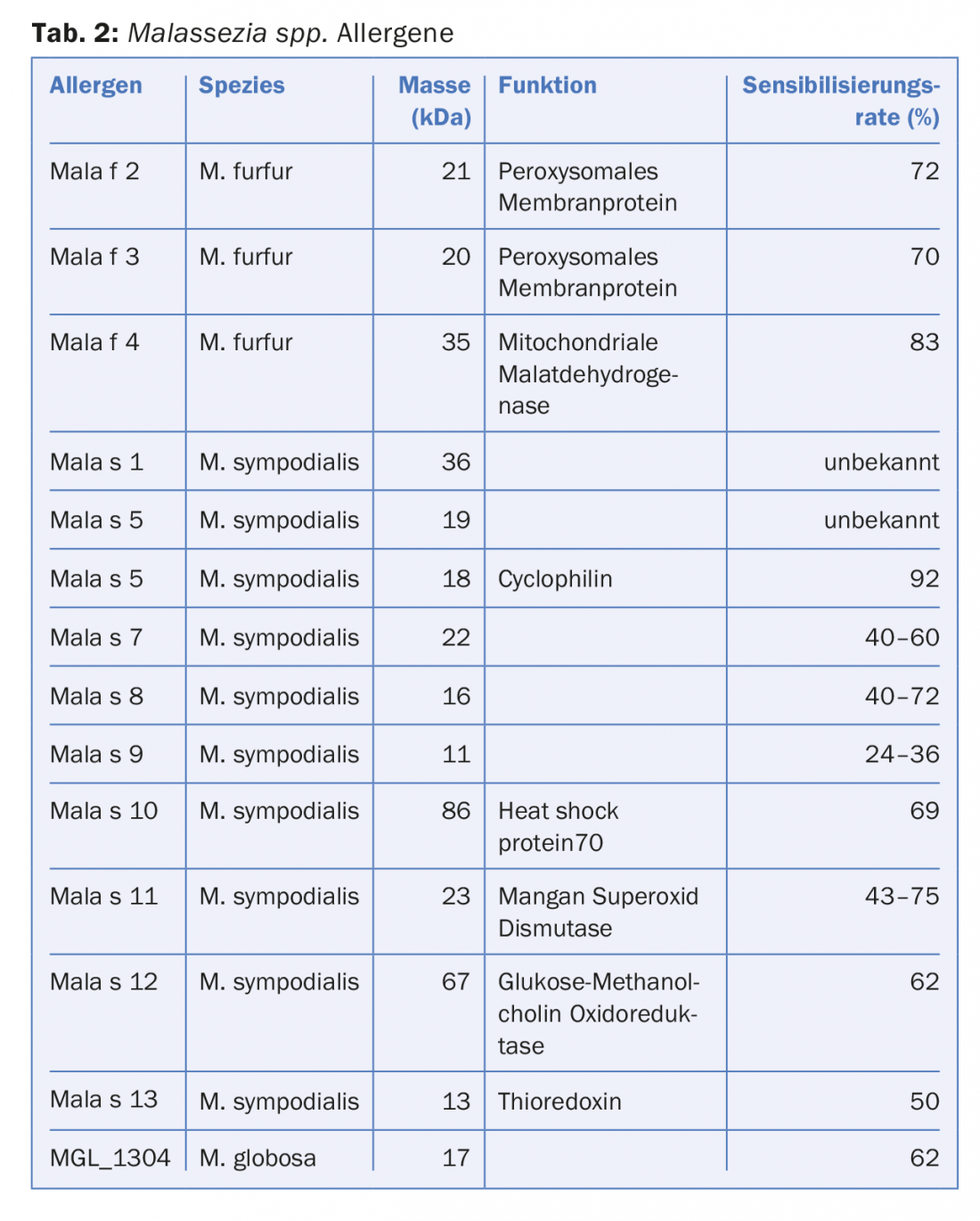
Other mechanisms by which Malassezia spp. contributes to eczema formation have been described, such as activation of Toll-like receptors and subsequent release of pro-inflammatory mediators by dendritic cells or keratinocytes [10]. Other possible mechanisms by which Malassezia spp. contribute to inflammation in AD are summarized in Figure 2.
Significance for practice
Detection of sensitization to Malassezia spp. may be useful when antifungal therapy for AD is being considered. At least two commercial and standardized test kits are available for the measurement of Malassezia spp.-specific IgE antibodies: ImmunoCAP® m70 or ImmunoCAP® m227, Thermo Scientific, www.phadia.com). The m227 test, in contrast to m70, is based on different Malassezia species and therefore appears to have a higher sensitivity. It may well be reasonable to try systemic antifungal therapy with azole antifungals in those patients with AD who are sensitized to Malassezia spp. Systemic therapy options for AD in particular are very limited, as cyclosporine is the only drug approved for systemic therapy of AD in many countries. In addition to the actual antifungal effect, azole antifungals inhibit the release of the pro-inflammatory interleukins IL-4 and IL-5 by Lzmphocytes. IL-4 and IL-5 in particular play a significant pathogenetic role in AD.
Literature:
- Grice EA, et al: Topographical and temporal diversity of the human skin microbiome. Science 2009; 324(5931): 1190-1192.
- Findley K, et al: Topographic diversity of fungal and bacterial communities in human skin. Nature 2013; 498(7454): 367-370.
- Kong HH, et al: Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Res 2012; 22(5): 850-859.
- Gaitanis G, Magiatis P, Hantschke M, Bassukas ID, Velegraki A: The Malassezia genus in skin and systemic diseases. Clin Microbiol Rev 2012; 25(1): 106-141.
- Bieber T: Atopic dermatitis. N Engl J Med 2008; 358(14): 1483-1494.
- Casagrande BF, et al: Sensitization to the yeast Malassezia sympodialis is specific for extrinsic and intrinsic atopic eczema. J Invest Dermatol 2006; 126(11): 2414-2421.
- Glatz M, et al: Malassezia spp.-specific Immunoglobulin E Level is a Marker for Severity of Atopic Dermatitis in Adults. Acta Derm Venereol 2015b; 95(2): 191-196.
- Selander C, Zargari A, Mollby R, Rasool O, Scheynius A: Higher pH level, corresponding to that on the skin of patients with atopic eczema, stimulates the release of Malassezia sympodialis allergens. Allergy 2006; 61(8): 1002-1008.
- Vilhelmsson M, et al: Mutational analysis of amino acid residues involved in IgE-binding to the Malassezia sympodialis allergen Mala s 11. Mol Immunol 2008; 46(2): 294-303.
- Glatz M, Bosshard PP, Hoetzenecker W, Schmid-Grendelmeier P: The Role of Malassezia spp. in Atopic Dermatitis. J Clin Med 2015a; 4(6): 1217-1228.
DERMATOLOGIE PRAXIS 2016; 26(4): 5-8











