In a seminar at this year’s KHM Congress, PD Dr. med. Silvia Ulrich Somaini, University Hospital Zurich, provided information on the most important aspects of pulmonary hypertension and how patients are best clarified and treated. Dr. med. Adelheid Hettich, practice Kappel, Ebnat-Kappel, asked questions relevant to practice.
(ee) “The small circulation is the big one,” said Silvia Ulrich, “because the lungs contain the entire cardiac output at all times!” The lungs are like a sponge that offers no resistance, so a lot of blood can flow through the pulmonary circulation. Mean pulmonary pressure should be less than 25 mmHg and wedge pressure (equivalent to left atrial pressure) should be less than 15 mmHg, otherwise pulmonary hypertension (PH) is present as part of a left heart problem.
From left heart failure to thromboembolism
The pathophysiologic mechanisms leading to PH vary widely:
- Left heart failure secondary to systolic or diastolic dysfunction or valvular disease. In diastolic dysfunction, the heart does not fill properly and there is blood back up into the lungs, especially during exercise.
- Hypoxic lung diseases, especially COPD: When there is not much oxygen in certain parts of the lungs, the vessels are contracted to prevent a shunt of deoxygenated blood into the systemic circulation in these parts of the lungs. As a consequence, the pressure in the pulmonary vessels increases. These patients are not served by vasodilator medications.
- Pulmonary hypertension due to chronic thromboembolism (CTEPH): This form of pulmonary hypertension occurs after pulmonary emboli scar the lungs. Only 60% of affected patients recall having pulmonary emboli. The treatment of choice here is surgical endarterectomy.
- Pulmonary arterial hypertension (PAH): The problem lies in the pulmonary vessels themselves.
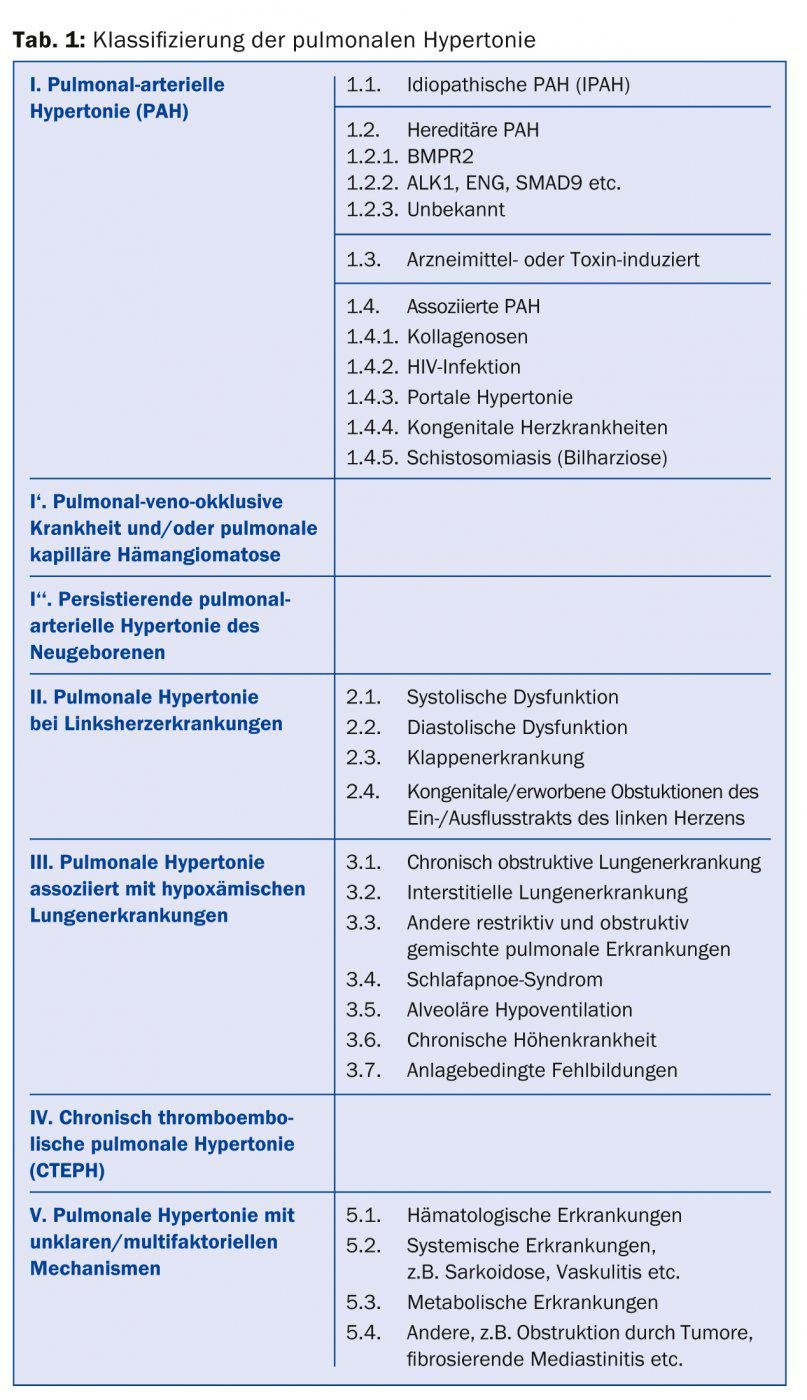
Accordingly, the various forms of PH are classified into five categories (Table 1). PH as a consequence of liver disease occurs more often than one might think. In the French registry, liver disease is now the most common cause of PH.
Diagnostic gold standard: the right heart catheter examination
The most common symptom in PH is exertion-dependent dyspnea. In addition, there are symptoms of forward failure such as fatigue, decreased performance, and syncope, and signs of reverse failure such as edema or weight gain. The latter symptoms usually appear only in advanced stages, as do ECG changes. “Especially in young women, it often takes years before a diagnosis is made because the symptoms are discrete and the affected individuals look healthy,” Silvia Ulrich said. “Often, patients adapt their lifestyle to their symptoms and simply don’t go jogging anymore, for example.”
If PH is suspected, primary investigations are performed for differential diagnosis of respiratory distress, for example, pulmonary function tests (spirometry, lung volume, etc.). Decreased diffusion capacity may be the first indication of PH. Echocardiography is important for differential diagnosis (valvular disease, vites), initial estimation of pressures, and evaluation of right ventricular function.
The gold standard for diagnosing PH is pressure measurement by right heart catheterization; access is usually through the jugular vein. The measurement is performed on an outpatient basis and takes about two hours. The examiner should have great experience, otherwise the results will not be reliable. In all patients with detected precapillary PH, vasoreactivity testing is also performed. In this procedure, a short-acting vasodilator is inhaled (nitric oxide, iloprost) or swallowed (sildenafil). Patients in whom this causes the mean pulmonary arterial pressure to fall by ≥10 mmHg to ≤ 40 mmHg may be treated primarily with a calcium antagonist. If CTEPH is suspected, a ventilation perfusion scintigram must be done because CT does not show old pulmonary emboli well.
Drug therapy of PAH
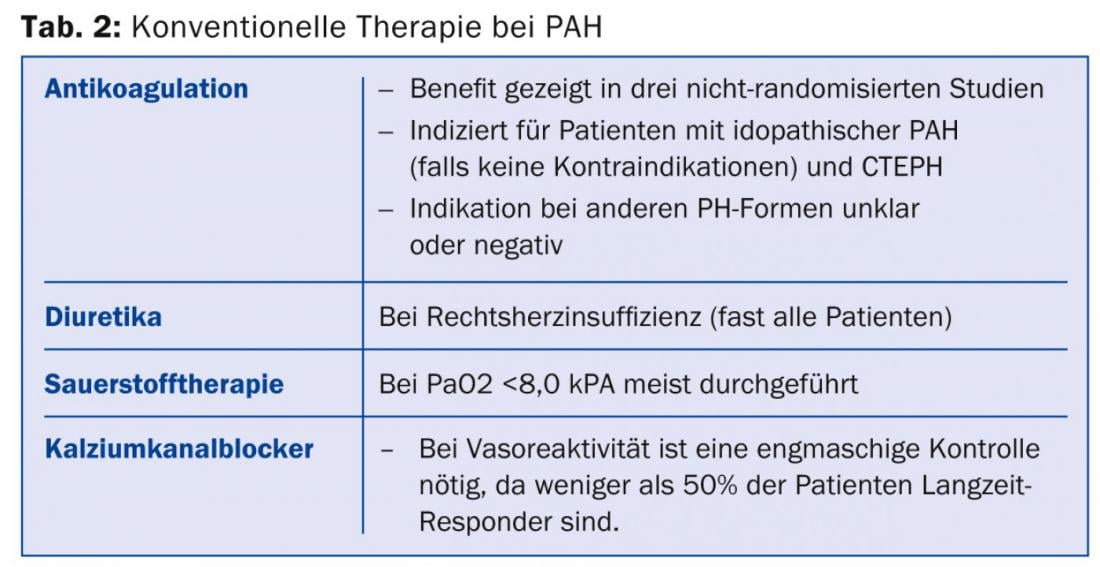
There are specific drugs for the treatment of patients with PAH or CTEPH; in all other patients with PH, only the underlying disease can be treated. Basically, a distinction is made between conventional (Tab. 2) and specific therapy, which includes the following agents:
- Prostanoid
- Endothelin receptor antagonists (ERA): Bosentan, ambrisentan, macitentan
- Phosphodiesterase-5 inhibitors (PDE5I): sildenafil, tadalafil
- Guanylate cyclase stimulator (sGCS): riociguat (approved in Switzerland for CTEPH only).
Treatment with the specific therapies is very expensive and complex, therefore these drugs are only suitable for patients who are cared for in a center and, if possible, are included in a registry (such as the Swiss PH Registry).
So far, prostanoids can only be given parenterally: via an intravenous catheter or subcutaneously implanted pumps tunnelled to the vascular system, by inhalation (laborious, as inhalation is required 6 – 8× per day for 5 minutes each) or subcutaneously with an insulin pump, which, however, can be painful. The subcutaneously implanted pumps are filled once a month. The pump costs around 20,000 Swiss francs and is estimated to last well over ten years. Thus, prostanoid prescribing is complex and needs experience. Possible side effects include pain at the subcutaneous injection site, hypotension, diarrhea, nausea, and flushing.
The vasodilator and antiproliferative endothelin receptor antagonists are taken orally. The new agent riociguat is currently approved for the treatment of inoperable CTEPH. Recent data from the Swiss Registry of Pulmonary Hypertension show that currently about 50% of the nearly 1000 registered patients receive combination therapies. The specific medications should be prescribed in a center, at the family doctor the regular checks of INR, electrolytes, liver values and much more.
Physical training
New studies show that highly specialized, targeted physical training is useful in patients with PAH – views here have changed from the past, when patients were advised to take it easy. However, it is important that the training is done carefully and under expert guidance (specialized physiotherapy) and started in a specialized center. Training is done with low watts and only one loaded muscle group at a time. Patients should stay fit but not overexert themselves.
Surgery for CTEPH
In the majority of patients with CTEPH, surgery is possible to peel out the scarred thromboemboli (endarterectomy, not embolectomy). The procedure is risky and complicated: Patients are cooled down to 18-20°C body temperature so that surgery can be performed in case of total circulatory arrest. Mortality is 2-10% depending on the risk constellation. This operation has been performed in Switzerland in close internal interdisciplinary collaboration and cooperation with international centers since September 2013 in Zurich; the demand is estimated at around ten operations per year throughout Switzerland.
Source: Seminar “Pulmonary Hypertension”, 16th Continuing Education Conference of the College of Family Medicine (KHM), June 26, 2014, Lucerne.
HAUSARZT PRAXIS 2014; 9(8): 38-41











