Headaches are one of the main issues in family practice today, which is why patients seek medical advice. Migraine, in particular, is widespread. Several epidemiological studies demonstrate its high prevalence and immense socioeconomic and personal impact. This presents a daily challenge for any primary care physician. This is because it is important, on the one hand, to quickly alleviate the symptoms and, on the other hand, to quickly identify the cause.
Basically, migraine can be divided into two main types, migraine without and with aura. Migraine without aura is a clinical syndrome characterized by a typical headache pattern and its accompanying symptoms. This so-called simple migraine is characterized by a recurring headache that, if left untreated, manifests itself through attacks lasting from four to 72 hours. Typical characteristics are unilateral localizations of moderate to severe intensity, which are aggravated by routine physical activities and involve the concomitant occurrence of nausea and sensitivity to light or noise.
Migraine with aura is characterized by transient focal neurologic symptoms that usually precede or accompany the headache. Some patients report a precursory phase that may precede the headache by hours or days and a recovery phase after the headache disappears. Symptoms of the precursor phase include hyperactivity, hypoactivity, depression, ravenous hunger for certain foods, repeated yawning, fatigue, and neck stiffness or pain. In rare cases, an aura without headache may also occur, a so-called “migraine sans migraine”. In migraine without headache, the patient perceives an aura, but often does not recognize it as such. The aura usually lasts from 15 minutes to a maximum of one hour and is accompanied by very mild or no headache. So that the visual problems are perceived but not associated with a migraine.
In the beginning is the diagnosis
The diagnosis of migraine is usually made by taking a medical history. If a patient meets the criteria for more than one type of migraine, they should all be diagnosed and coded. Because differentiating a single or isolated migraine attack from symptomatic migraine-like attacks can be difficult, the diagnosis requires at least five attacks that have two or more of the following four characteristics: unilateral localization, pulsatile nature, moderate or severe pain intensity, intensification by or leads to avoidance of routine physical activities (e.g., walking or climbing stairs). Typically, the symptoms appear with the onset of puberty. In addition, migraine has a strong genetic component and its prevalence is higher in patients with directly affected first-degree relatives than in the general population. Family history is therefore an important part of the medical history and is often positive in migraine patients. For example, migraine without aura has a threefold increased risk of first-degree relatives also having migraine without aura. The risk is twice as high for both migraine with aura and migraine without aura. Physical examination is confirmatory in most cases, and further investigations are needed only to confirm or refute suspicions of secondary causes of headache.
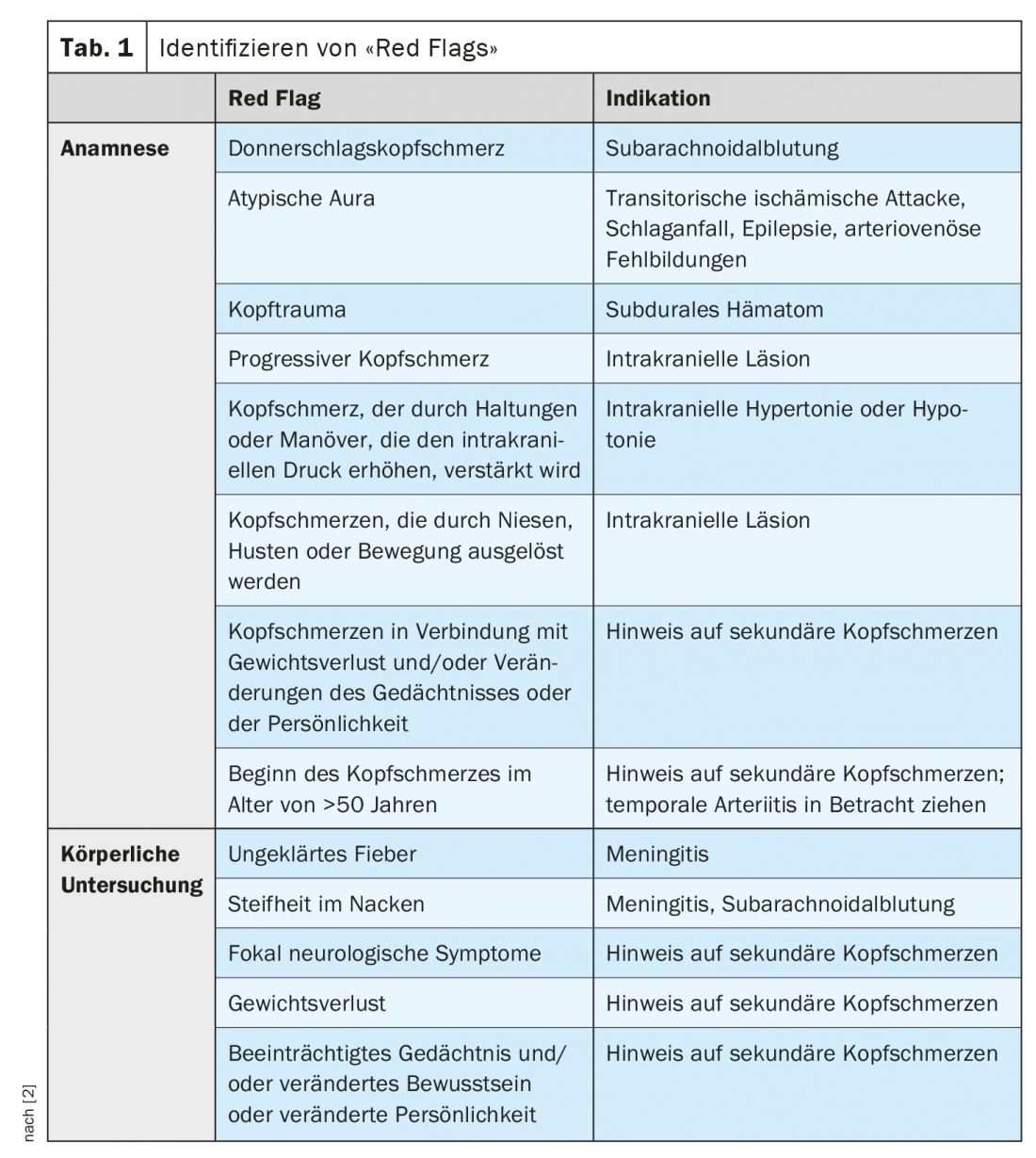
Identifying “Red Flags
In order to guide the need for and type of additional diagnostics, the identification of warning symptoms (“red flags”) is crucial (Table 1) [2]. Further clarification is needed, for example, in acute/peracute headaches that may indicate subarachnoid hemorrhage (SAB) or atypical auras that occur suddenly without a known migraine. In addition, positional headaches suggestive of intracranial hypertension or hypotension should be further investigated, as should headaches that occur with age, as these are often preceded by a secondary cause. Head trauma or abnormal symptoms on clinical examination, such as fever, weight loss, etc., also require further neurologic evaluation. Dr. med. et phil. David Winkler, Head of Neurology at the Baselland Cantonal Hospital, refers at this point to a patient with a flu-like infection and a severe cough, followed by daily headaches. Finally, an MRI shows meningeal thickening, which was caused by negative pressure in the CSF system due to a spontaneous CSF leak [2].
Attack therapy and prophylaxis
Symptomatic measures can reduce the frequency of migraine attacks and their severity. The main thing is to avoid provoking factors, such as caffeine, alcoholic beverages, chocolate, milk, nuts or citrus fruits. Regular aerobic endurance exercise as well as pain management, stress management and relaxation techniques may also be helpful. In addition, a guided headache calendar can provide information on when the migraine attacks occur and contributed to treatment.
First-line medications for attack therapy include over-the-counter analgesics, such as nonsteroidal anti-inflammatory drugs (NSAIDs). However, these should only be used <10 days a month, otherwise medication overuse headache may occur. Metoclopramide or domperidone may also be prescribed for nausea. For more severe headache attacks, triptans such as almotriptan, eletriptan, frovatriptan, naratriptan, rizatriptan, sumatriptan, or zolmitriptan may be used. These should also be used <10 days a month and treatment should be started early in the migraine attack but after the aura has subsided. Depending on the migraine attack / course, it is possible to apply the triptans nasally or subcutaneously, which leads to a rapid onset of action, which, however, is not long-lasting. If, on the other hand, the triptans are administered orally, this leads to a delayed onset of action with a long-lasting effect.
Newer drugs already approved in the U.S. include Gepante and Ditane. Gepante are CGRP receptor blockers with the same mechanism of action. Ditans are serotonin receptors that have the same mechanism of action as triptans but have fewer vasoactive side effects and therefore can be used in cardiac risk patients. It is worth mentioning, however, that the ability to drive is restricted for eight hours.
CGRP antibody therapy – new form of migraine prophylaxis
The prerequisite for the indication of migraine prophylaxis is three or more migraine attacks per month, which limit the quality of life. These so-called complicated migraine attacks, with debilitating and/or long-lasting auras, regularly last longer than 72 hours. In this case, basic therapies can be administered. Various classes of substances are available here, such as beta blockers, antiepileptic drugs, calsium antagonists and psychotropic drugs, which reduce the attack frequency by 50%. Which substance should be administered depends on the patient’s side effect profile.
A new form of migraine prophylaxis is CGRP antibodies, which must be prescribed by a neurology specialist. Here, too, there are different substances. On the one hand antibodies against the CGRP receptor, on the other hand against the Calcitonin Gene-Related Peptide (CGRP) itself. This peptide is released from the trigeminal nerve towards the dura and leads to water dilatation at the dura. In addition, there are cells from the trigeminal nerve that use this peptide to influence the pain afferent from the dura toward the thalamus. It can be assumed that the action of the antibodies takes place primarily in the trigeminal nerve. Thus, the main effect is a regulation of water dilatation of blood vessels, which leads to a significant reduction in migraine frequency. Therapy with erenumab leads to a reduction of up to four migraine days per month [3]. For CGRP antibody therapy, at least two other baseline therapies must have been used previously, which documented with a headache calendar either did not respond or were not tolerated, or for which there is a contraindication.
Not all headaches are the same
Besides migraine, there are other types of headaches. For example, tension headache is a mild to moderate holocephalic headache with a dull-pressing character. Vegetative signs are usually completely absent. If there is chronic tension-type headache and medication overuse, the temporal relationship is often difficult to establish. Therefore, in such cases both diagnoses, chronic tension-type headache and headache attributed to medication overuse, are assigned. Accut therapy consists of taking NSAIDs. For basic therapy, amitriptyline, mirtazapine, or venlafaxine may be administered, and additional physical therapy may be prescribed.
A rather rare form is cluster headache. In this type of headache, the pain can be invalidating with long pauses and predominantly nocturnal attacks. The diagnosis is a unilateral headache with retroorbital punctum maximum and Horner’s syndrome on the side of the pain; rhinorrhea is also not a factor. Attacks can occur up to eight times daily and last from 15 to 180 minutes. Accut therapy consists of 100% oxygen via face mask, sumatriptan/zolmitriptan nasal spray, or intranasal application of lidocaine 4-10%. Verapamil/topiramate (off-label) can be administered as prophylaxis.
Literature:
- PD Dr. med. et phil. David Winkler: “Headache and Mirgrine,” Forum for Continuing Medical Education, Sept. 08, 2021.
- Eigenbrodt, et al: Diagnosis and management of migraine in ten steps. Nature Reviews Neurology 2021, doi: 10.1038/s41582-021-00509-5.
- Goadsby, et al: A Controlled Trial of Erenumab for Episodic Migraine. N Engl J Med 2017, doi: 10.1056/NEJMoa1705848.
HAUSARZT PRAXIS 2021; 16(11): 45-46











