Dust mite allergy is characterized by year-round symptoms of the nose, lungs and/or eyes. Inadequate diagnosis and treatment may favor the development of allergic asthma (“floor change”). If symptomatic therapy does not produce the desired effect, hyposensitization can lead to sustained relief. In advance, a molecular diagnostic clarification is performed to identify the allergens.
In contrast to seasonal allergic rhinitis, perennial rhinitis occurs year-round and is primarily due to allergens in the home (e.g., feces of dust mites, cockroaches, animal dander, mold), possibly also due to strong reactivity to pollen in the different seasons. Worldwide, an estimated half a million people are affected by dust mite allergy (box) [1,2]. Altogether there are numerous different mite species, in our latitudes mainly Dermatophagoides pteronyssinus and D. farinae are allergy-relevant. Most patients are sensitized to allergens of both types, but monosensitization is less common. A mite produces up to 40 fecal balls per day, and a teaspoonful of bedroom dust contains an average of nearly 1000 mites and 250,000 tiny fecal balls [4].
Treat symptomatically if prick test is positive
Dust mite allergens spread through the air like grass and tree pollen. The prick test shows good significance in allergies induced by aeroallergens. First, however, a thorough history should be taken of the symptoms and the time course of onset. The diagnosis of allergy cannot be made solely on the basis of a positive skin test reaction, but only in conjunction with the corresponding clinical picture and a suitable medical history. Ralph Litschel, MD, ENT practice at Roter Platz, St.Gallen, demonstrated the procedure by means of a case study [5]. Prick test showed a strong reaction to mites with sensitization to tree and grass pollen in one patient. Symptomatic therapy was performed with Dymista®, a nasal spray containing azelastine hydrochloride (antihistamine) and fluticasone (cortisone) [6]. In addition, eye drops containing olopatadine (Opatanol®) and a systemic H1 antihistamine (Bilastin) were prescribed [6]. That provided symptomatic improvement, but the patient wanted longer-term effective therapy, Dr. Litschel said. To this end, further clarifications were launched.
Specific immunotherapy based on component-based diagnostics
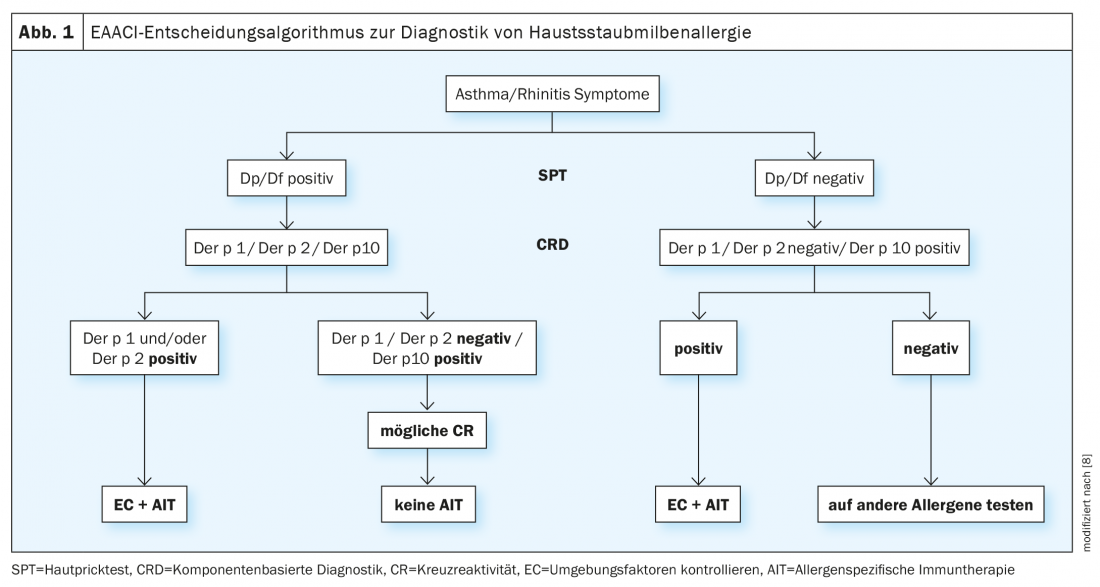
For further laboratory diagnostic clarification, specific allergen sources can be identified by serological IgE tests. A further development is the so-called molecular allergy diagnostics, which is also called component-based diagnostics: IgE antibodies are determined against individual allergen molecules (“allergen components”). These proteins are grouped into protein families based on structural similarities. This method is much more sensitive and, especially in the case of special questions, more informative than conventional test methods. Allergen sources may contain both specific and cross-reactive allergen components. The number of known and commercially available allergen molecules for the determination of specific IgE antibodies has increased significantly in recent years. In house dust mite allergy, Der p 1 and Der p 2 are among the majorallaergens. Determination of Der p 1 and Der p 2 can diagnose over 97% of patients with allergy to D. pteronyssinus [1,7]. Cross-reactivity between D. pteronyssinus and D. farinae is high, so it is not necessary to test both species [8]. If the test results show evidence of sensitization, this is decisive for the indication of a specific immunotherapy [1].
Systematic hyposensitization brings lasting relief
The aim of specific immunotherapy/hyposensitization is to reduce allergy symptoms in the medium and long term. The duration is about three years. Hyposensitization can be applied in childhood as well as in adulthood. The basic principle is to gradually accustom the immune system to the allergy triggers. For this purpose, allergen extracts are administered to the body in the form of injections or as tablets or drops. The amount of extract supplied is initially very small, and the dose is gradually increased until a maximum personal dose is reached, which is then administered at regular intervals. In subcutaneous immunotherapy (SCIT), the allergens are administered with the help of injections. In sublingual immunotherapy (SLIT), the allergens are taken sublingually as drops or tablets. SCIT is more complex, regular visits to the doctor are required. SLIT, on the other hand, can be performed by the patient at home.
SLIT: randomized trials demonstrate efficacy and safety
Acarizax® [6] is an SLIT preparation available in Switzerland for the indication of moderate to severe rhinitis with proven sensitization to house dust mites. Efficacy and safety of SLIT in house dust mite allergic patients have been demonstrated in several studies. The following are the findings of two selected RCTs:
Bergmann et al. 2014 [10]: This randomized-controlled double-blinded study evaluated the efficacy and safety of 2 doses of SLIT with house dust mite allergens over 1 year of treatment and the following immunotherapy-free year. At the end of the study period, evaluable data were available from 427 subjects. Both 500IR and 300IR house dust mite SLIT resulted in significantly reduced mean symptom scores compared to placebo (-20.2%, p=0.0066 and -17.9%, p=0.0150, respectively). The efficacy of both doses was maintained during the treatment-free follow-up phase. The effect started after 4 months. Adverse reactions were mainly local reactions; no anaphylaxis was reported.
Demoly et al. 2016 [9]: This randomized-controlled double-blind phase III study, conducted in 12 European countries, enrolled 992 adults with moderate to severe house dust mite-induced respiratory allergic symptoms that were inadequately controlled with medication. Subjects were randomized 1:1:1 to 1 year of daily treatment with 6 SQ-HDM tablet, or 12 SQ-HDM tablet, or placebo. The primary endpoint was the total combined rhinitis score during the efficacy evaluation phase (i.e., approximately the last 8 weeks of the treatment period). Data analyses showed absolute reductions in total combined rhinitis score of 1.18 (p=0.002) for 6 SQ-HDM and 1.22 (p=0.001) for 12 SQ-HDM compared to placebo. A statistically significant treatment effect was seen from week 14 after treatment initiation.
Congress: FomF Family Doctor Training Days St. Gallen
Literature:
- Ballmer-Weber B, Helbling A: A popular disease of the 20th century. Allergic rhinitis. Swiss Med Forum 2017; 17(08): 179-186.
- Batard T, et al: Patterns of IgE sensitization in house dust mite-allergic patients: implications for allergen immunotherapy. Allergy 2016; 71: 220-229.
- Portnoy J, et al: Environmental assessment and exposure control of dust mites: a practice parameter. Ann Allergy Asthma Immunol 2013; 111: 465-450.
- Allergiezentrum Schweiz: Hausstaubmilbenallergie, www.aha.ch/allergiezentrum-schweiz (last accessed 06.05.2021)
- Litschel R: Allgeriebekämpfung – Was gibt es Neues? Ralph Litschel, MD, FomF, Family Physician Continuing Education Days, 03/12/2021
- Drug Information, www.swissmedicinfo.ch (last accessed 05/06/2021).
- Veghofer M, et al: Variability of IgE reactivity profiles among European mite allergic patients. Eur J Clin Invest 2008; 38(12): 959-965.
- Matricardi PM, et al: EAACI Molecular Allergology User’s Guide.Pediatr Allergy Immunol 2016; 27 Suppl 23: 1-250.
- Demoly P, et al: Effective treatment of house dust mite-induced allergic rhinitis with 2 doses of the SQ HDM SLIT-tablet: Results from a randomized, double-blind, placebo-controlled phase III trial. J Allergy Clin Immunol 2016; 137(2): 444.
- Bergmann KC, et al: Efficacy and safety of sublingual tablets of house dust mite allergen extracts in adults with allergic rhinitis. J Allergy Clin Immunol 2014; 133(6): 1608-1614.e6. Epub 2013 Dec 31.
HAUSARZT PRAXIS 2021; 16(6): 38-39 (published 6/6/21, ahead of print).