If headaches occur regularly, they can lead to a significant reduction in quality of life. Majority are primary headaches, with migraine and tension-type headaches being the most common. In addition to a wide range of options for pharmacotherapeutic treatment and prophylaxis, adjustment of lifestyle factors can also contribute to prophylaxis and coping.
Headache is the sixth leading cause of years of life lost to disability, according to data from the Global Burden of Disease Study published in the Lancet [1]. “Patients are significantly restricted in their everyday life and family life,” explains PD Hakan Sarikaya, MD, Inselspital Bern. To date, no curative treatment exists, and the currently available therapies are all symptomatic [2]. The fact that recurrent relapses usually occur can sometimes lead to frustration among patients, the speaker explained. In health economic terms, the direct and indirect costs associated with headache disorders are considerable.
Primary or secondary headache?
According to the International Headache Society, there are 200 different types of headache, with a distinction between primary and secondary forms (overview 1) and a division into a total of 14 subgroups [3]. In clinical practice, most cases are tension-type headaches, with migraine headaches being the second most common [2]. Secondary headaches and cluster headaches are less common [2]. Routine checks in the evaluation of headache patients include: Meningismus, mobility of the cervical spine, pressure dolence of the temporomandibular joint and muscles, myogelosis of the neck and shoulder muscles, Horner’s syndrome. In addition, a measurement of blood pressure should be performed. If the etiology is unclear, the speaker recommends magnetic resonance imaging (MRI) testing.
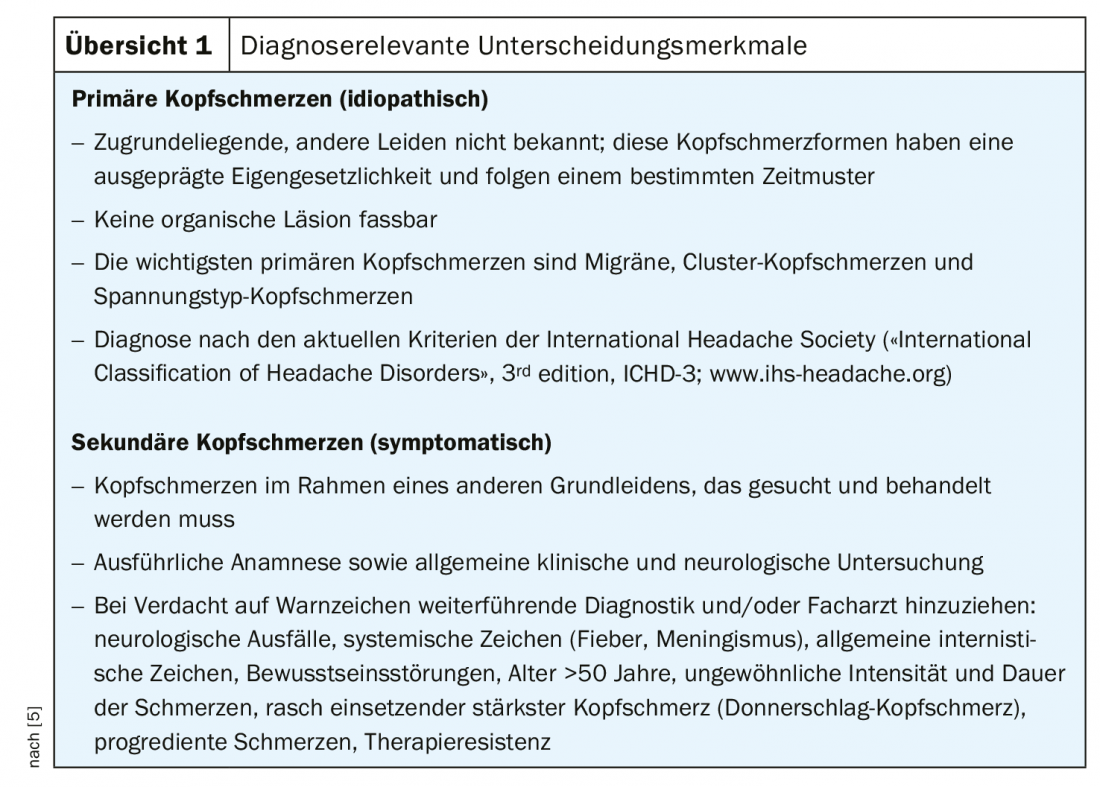
To rule out secondary causes of headache, the following possible etiologies should be reviewed in particular: Subarachnoid hemorrhage, meningitis, hypertensive BP levels, sinusitis, temporal arteritis, dissection, post-traumatic causes/cranlotomy, reversible cerebral vasoconstriction syndrome (RCVS), cerebral venous/sinus thrombosis, medication-overuse headache, idiopathic intracranial hypertension, temporal arteritis (only after age 60), brain tumor, epileptic seizures.
If the headache is primary, a careful history is particularly important with regard to the following factors: duration, intensity, pain character, localization, accompanying symptoms, trigger, behavior during the pain attack, time of day, positional dependence, medication use. Which subtype of headache is involved can be ascertained by specific clinical features [2]:
- Migraine: pulsatile, unilateral, nausea/vomiting, photophobia/phonophobia, movement increased, 4-72 hours, trigger factors.
- Tension headache: dull, diffuse bilaterally, mild-medium, no accompanying symptoms.
- Cluster headache: unilateral (around the eye), most severe pain, tearing, redness of the eye, blocked nose, waking up at night and symptoms around the same time
- Chronic migraine and medication overuse headache: almost daily, rather dull-pressing, attacks strong, migraine-like, pain medication >10 days.
Migraine symptoms are usually not characterized exclusively by headaches, but are accompanied by other accompanying symptoms. According to a US study (n=510), the most common were light sensitivity (90%), difficulty concentrating (82%), nausea (69%), and irritability (60%) [4]. Migraine is also frequently associated with depression and anxiety disorders, sometimes sufferers have irritable bowel syndrome and fibromuscular dysplasia, and if cardiovascular risk factors are present, the risk of stroke is increased. The speaker mentioned that a possible migration background could also play a role in the clarification of headache patients, as there are certain culture-specific differences, e.g. with regard to pain assessment and communication.
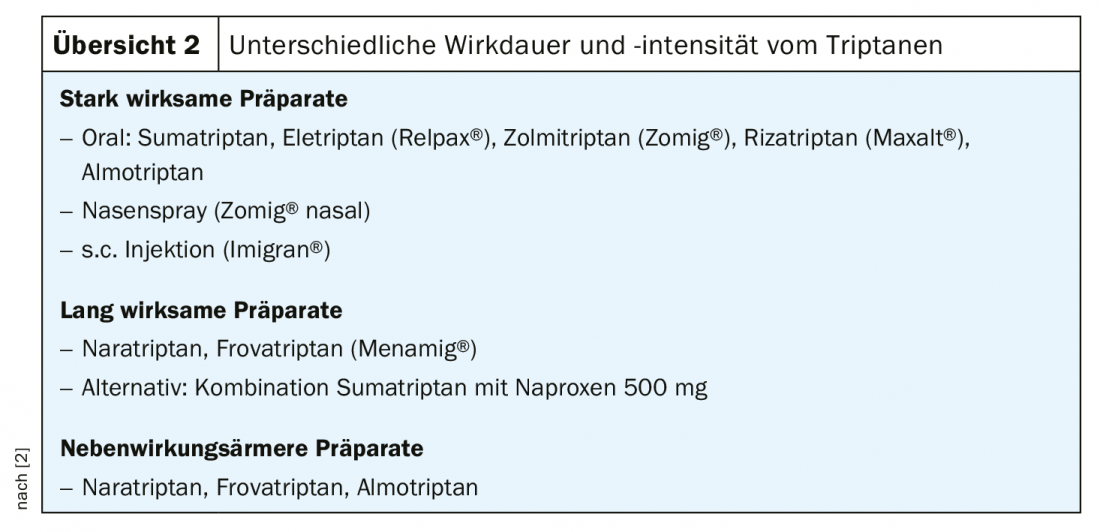
Triptans: high value for the acute treatment of migraine
The treatment of migraine attacks with moderate and high pain intensity and disability in everyday life is mainly done with triptans. These are characterized by specific and strong efficacy in migraine. Early use is important, but not in the aura phase. There are preparations in various forms of administration: Per os, sublingual, subcutaneous, nasal spray. The individual substances are basically interchangeable, although there are certain differences in terms of duration and intensity of action (overview 2) . In general, the following three points should be considered for the pharmacotherapeutic treatment of mild to moderate intensity attacks: sufficiently high dosage, early intake, no excessive frequency. As a non-drug measure, the speaker recommends rest, sleep and relaxation.
What are the criteria for long-term prophylaxis?
According to treatment recommendations published in 2019 by the Swiss Headache Society [5], long-term prophylaxis may be considered for primary headaches in the following cases: more than three attacks per month (>5 days), very severe or prolonged seizures, protracted or clustered auras, intolerance of acute therapeutic agents, in cases of medication overuse headache, when quality of life is markedly impaired, and when patient wishes. For long-term pharmacotherapeutic prophylaxis to be as effective and safe as possible, consideration of the following aspects has proven helpful:
- If the benefit is good (which should be evident after 8 weeks at the latest), long-term prophylaxis can be continued for 6-12 months.
- Acute medications should not be used for long-term treatment (caveat: medication overuse headache)!
- Comorbidity influences drug choice (weight gain with flunarizine and amitriptyline, for example; contraindications to beta-blockers in patients with severe asthma, hypotension; beta-blockers, flunarizine, and topiramate may promote depression).
- Desirable side effects can be targeted (e.g., weight reduction by topiramate, sedative effect by amitriptyline, laxative effect of magnesium, blood pressure and pulse lowering effect by beta blockers).
- If lamotrigine and topiramate are used, watch for interactions with hormonal contraceptives. Topiramate and valproate are teratogenic, so these should only be used under safe anticonception.
The following non-drug measures have also been shown to be effective for long-term prophylaxis: aerobic endurance training (3× 30 min/week), stress management, progressive muscle relaxation, behavioral measures (regular meals, regular sleep schedules, cognitive behavioral therapy, avoidance of trigger factors), acupuncture/manual therapy.
Source: FOMF Zurich
Literature:
- GBD 2015 DALYs and HALE Collaborators: Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388 (10053): 1603-1658.
- Sarikaya H: Slide presentation, PD Hakan Sarikaya, MD. Symposium: Neurology: Headache, Internal Medicine – Update Refresher. 03.12.2019, Zurich.
- International Headache Society: The International Classification of Headache Disorders 3rd edition, Cephalalgia 2018; 38(1): 2011-2211, https://ichd-3.org
- Gonzalez JM, et al: Headache 2013; 53(10): 1635-1650.
- Swiss Headache Society: Therapy recommendations for primary headache incl. Headache Algorithm for the Family Physician, 10th Completely Revised Edition 2019, www.headache.ch
GP PRACTICE 2020; 15(4): 24-25.