Approximately one-fifth of all cancers are caused by diet, overweight and obesity. Crucial in terms of cancer development are mainly too much red and processed meat, alcohol and salt; little fruit, vegetables and fiber.
The aging population in Switzerland is leading to an increasing number of people suffering from chronic diseases such as cardiovascular diseases, diabetes mellitus and cancer. In Switzerland, 18,443 women and 21,395 men developed cancer in 2013; 7475 women and 9200 men died from it. This makes cancer the second leading cause of death in Switzerland after cardiovascular disease [1].
There are many causes of cancer and risk factors vary greatly depending on the type of cancer. Despite similar formation mechanisms, individual factors have partly different effects. This also applies to lifestyle factors, some of which have a very strong influence on the emergence and development of cancer. The most important lifestyle risk factor is smoking, which, based on figures from a British study, is responsible for 20% of all cancers [2]. About 9% are caused by too little fruit, vegetables and fiber, too much red meat, too much salt and another 4% by alcohol consumption. Overweight and obesity, both caused at least in part by diet, account for another 5.5%. Depending on the database, these estimates vary slightly: for example, in an estimate by the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR), 26% of all cancer cases were explained by diet, obesity, alcohol consumption, and lack of physical activity, compared with 18% in the British study.
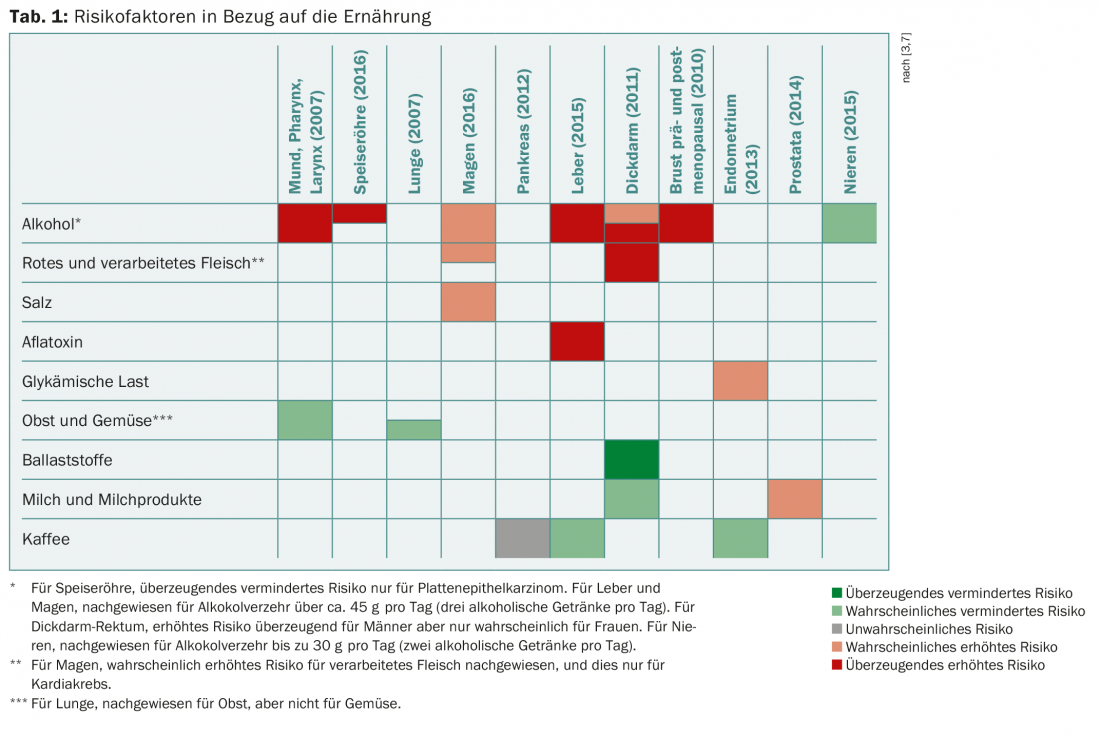
The diversity of the individual tumor types and the variety of risk factors produces a wealth of scientific publications that is currently almost unmanageable. The WCRF/AICR has set itself the task of continuously evaluating risk factors concerning nutrition and obesity and producing evidence-based summaries [3]. The most important risk factors related to nutrition are briefly presented below (Table 1).
Alcohol
Alcohol was classified as a carcinogen by the International Agency for Research on Cancer (IARC) in 2007 [4]. It has the best evidence regarding cancer risk, and based on the WCRF/AICR evaluation, the association with risk of tumors of the mouth, pharynx, esophagus, stomach, liver, colon and rectum, and breast is convincing or at least likely (in contrast, alcohol consumption may be associated with reduced risk of kidney cancer). The excess consumption of 50 g of alcohol per day (about three alcoholic drinks) is associated with an increase in relative risk of 50% for breast cancer and 40% for colon cancer [4]. For tumors in the upper respiratory and digestive tracts, alcohol consumption is associated with a doubling to tripling of relative risk, and smoking appears to amplify the effects of alcohol consumption. Based on the European Prospective Investigation into Cancer and Nutrition (EPIC), it has been estimated that approximately 9% of all cancer cases in men and 3% in women are attributable to excessive alcohol consumption [5]. The German Nutrition Society recommends a maximum of two alcoholic drinks per day for men and only one for women.
Red and processed meat
The effect of red and processed meat on cancer risk has also been studied by IARC [6] and WCRF/AICR [3]. Consumption of processed meat has been classified by IARC as carcinogenic to humans, and consumption of red meat as probable carcinogen [6]. This correlation is particularly visible for colon cancer, but also for stomach cancer. The risk increase associated with high consumption is moderate at 18% per 50 g daily increase in processed meat consumption. For example, the Robert Koch Institute has calculated that the absolute risk of a 65-year-old man developing colon cancer in the next ten years is 2.4%. With a daily increase in consumption of 100 g of processed meat per day, it rises to 3.3%.
Salt, nuts, cereals and glycemic load
In addition, salt is considered a risk factor for gastric cancer, and quite clearly, consumption of moldy nuts and grain products is associated with an increase in liver cancer risk due to the associated aflatoxin intake [3]. Currently, glycemic load is also discussed as an influencing factor; so far, a positive association with the risk of endometrial cancer is considered possible [3,7].
Fruits and vegetables, fiber
Evaluation of the WCRF/AICR shows only a probable beneficial association between fruit consumption and the risk of tumors of the mouth, pharynx, and lung and between vegetable consumption and tumors of the mouth and pharynx. Fruits and vegetables have long been the favored foods when it comes to a protective effect in relation to carcinogenesis, as they are rich in vitamins and phytochemicals that influence many corresponding mechanisms, at least in vitro. However, large prospective studies showed that this effect is nowhere near as strong as has long been assumed. An evaluation of the European Prospective Investigation into Cancer and Nutrition showed that a 200 g higher consumption of fruits and vegetables per day, reduces the overall risk of cancer by only 3% (95% CI 1-4%) [8].
Part of the effect on the colon is likely mediated via dietary fiber, and the WCRF/AICR rated the association between dietary fiber intake and colon cancer as compelling [3]. An additional intake of 10 g per day reduces the risk of disease by 10% [9], and fiber intake from cereals and whole-grain products seems to be particularly important. High consumption of legumes (pulses) is discussed as a protective factor for gastric cancer [3].
Milk and dairy products
Milk and dairy products are commonly considered important in the context of bone health. With regard to cancer risk, contradictory results are seen depending on the cancer site: while a protective effect of high consumption on the risk of colon tumors is seen – per 400 g of milk and dairy products, the risk decreases by 17% (95% CI 12-22% [10]) – a high calcium intake of more than 1200 mg per day seems to be associated with an increased risk of prostate cancer on the other hand. As a possible explanation, it is discussed that high calcium concentrations in the colon tend to promote the differentiation of epithelial cells; in contrast, in the prostate, they tend to lead to the proliferation of cells [11].
Coffee
Coffee is increasingly becoming the focus of research, and coffee consumption is now being discussed as a protective factor for some cancer sites. The WCRF/AICR considers a risk-reducing effect on the risk of endometrial and liver cancer likely [3].
Conclusion
Consumption of processed meat and alcohol increases cancer risk, according to IARC estimates. Other influencing factors discussed include consumption of fruits and vegetables (protective), dairy products (varies by organ), coffee, and salt. However, the mechanisms are still unclear in many cases – on the one hand, substances contained in the food, such as vitamins, may play a role, but on the other hand, substances produced during food processing may also play a role. The question of the influence of genetic differences on the relationship between diet and cancer risk is largely unresolved.
Take-Home Messages
- An estimated 15-20% of all cancers are caused by diet and by overweight and obesity.
- Decisive dietary factors in relation to cancer development are too much red and processed meat, alcohol and salt; too little fruit,
- Vegetables and fiber.
- Nutritional factors have the strongest influence on tumors of the digestive tract.
Literature:
- Foundation National Institute for Cancer Epidemiology and Registration (NICER): Annual mortality rates. Annual incidence rates. 2013. www.nicer.org/en/statistics-atlas/
- Parkin DM, Boyd L, Walker LC: 16. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer 2011; 105(Suppl 2): S77-81.
- World Cancer Research Fund International: Continuous Update Project findings & reports. Continuous Update Project 2017. www.wcrf.org/int/research-we-fund/continuous-update-project-findings-reports
- Baan R, et al: Carcinogenicity of alcoholic beverages. Lancet Oncol 2007; 8: 292-293.
- Schutze M, et al: Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study. BMJ 2011; 342: d1584.
- Bouvard V, et al: Carcinogenicity of consumption of red and processed meat. Lancet Oncology 2015; 16(16): 1599-1600.
- American Institute for Cancer Research/World Cancer Research Fund: Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Washington, DC: AICR 2007.
- Boffetta P, et al: Fruit and vegetable intake and overall cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC). J Natl Cancer Inst 2010; 102: 529-537.
- Aune D, et al: Dietary fibre, whole grains, and risk of colorectal cancer: systematic review and dose-response meta-analysis of prospective studies. BMJ 2011; 343: d6617.
- Aune D, et al: Dairy products and colorectal cancer risk: a systematic review and meta-analysis of cohort studies. Ann Oncol 2012; 23: 37-45.
- Lamp JW: Dairy products and cancer. J Am Coll Nutr 2011; 30: 464S-470S.
InFo ONCOLOGY & HEMATOLOGY 2017; 5(3): 29-31.
HAUSARZT PRAXIS 2017; 12(9): 26-28











