Case report: For three to four months, this six-year-old boy developed two skin-colored nodules in the abdominal region, which increased significantly in size during the course.
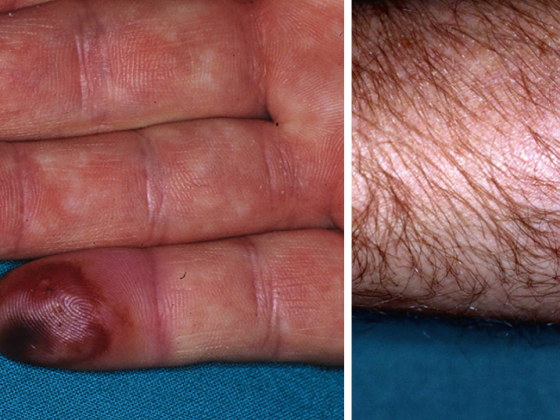
Apart from mild itching, there are no other symptoms. The patient is otherwise healthy, vaccinated according to CH regimen and has never had skin problems before. On examination, two oval, skin-colored, slightly shiny, coarse, bifurcated nodules, each about 20×5 mm in size, with marginal crusts, are seen in the left abdominal region (Fig. 1) . Examination of the remaining integument is unremarkable.

Quiz
Based on this information, what is the most likely diagnosis?
A Verrucae vulgares
B Molluscum contagiosum giganteum
C Juvenile xanthogranuloma
D Nevus Spitz
Diagnosis and discussion: The clinical picture shows typical so-called giant molluscs (Molluscum contagiosum giganteum, response B). Mollusca contagiosa (synonyms: dell warts, flying warts) are characterized by (usually) 1-5 mm skin-colored, bifurcated, dermal papules. Typical of Mollusca contagiosa is a central indentation with a porus from which crumbly whitish material (virus particles) can be expressed. Mollusca contagiosa are a common, contagious, benign, and self-limiting skin disease in children caused by DNA virus from the poxvirus family [1]. Rarely, the lesions can reach a diameter of several centimeters and are then referred to as so-called giant molluscs, as in the present case [2]. In contrast to adulthood, giant mollusks are very rarely associated with immunodeficiency, as is extensive infestation of mollusks. However, further investigations are indicated in case of additional clinical indications.
Virus transmission occurs directly from person to person or by autoinoculation. Mollusca contagiosa can manifest basically on the whole integument, but prefer intertriginous areas such as the axillae and the genital region, furthermore also the flanks and the face. Mucosal infestation is very rare. The spread of dell warts is favored by a disturbed skin barrier, especially in the context of atopic dermatitis, which can lead to disseminated seeding of mollusks, known as eczema molluscatum [3]. Molluscs around the lid margin can cause keratoconjunctivitis and, in rare cases, lead to corneal scarring. Another complication is secondary impetiginization with abscess formation.
Considering the high spontaneous remission (usually within six months in immunocompetent children), not every infestation of common nipples needs active therapy. In principle, regular, intensive, lipid-replenishing skin care (and, in eczema patients, anti-inflammatory local therapy) is recommended to prevent further seeding and promote healing. Therapy is often desired for prolonged, subjectively bothersome molluscs and/or complications. To date, there is no specific antiviral therapy for molluscum contagiosum. The choice of treatment method should be based on the extent of the mollusc infestation as well as the age, acceptance and compliance of the patient and possible adverse effects of the respective form of therapy. Before starting treatment, any existing eczema should be allowed to heal (using topical corticosteroids; topical calcineurin inhibitors should be avoided).
In slightly older, cooperative children with a manageable number of molluscs, mechanical ablation using a curette (sharp spoon) or forceps under anesthetic cream (e.g. Emla®) is a good and simple option – as is cryotherapy with liquid nitrogen (without anesthetic cream).
For numerous molluscs or anxious (younger) children, we use a topical potassium hydroxide solution 5% (e.g., Infectodell®) as first-line therapy. This substance leads to lysis of the virus-infected cells. Careful application of the solution with applicator is performed once or twice daily until a clinically detectable inflammatory response is seen. Occasionally this causes burning and irritation, but overall it is easy to perform, inexpensive, effective, and has few side effects [4]. Potassium hydroxide solution should not be used in mucosal areas, periorbital areas or on eczematized skin.
The giant molluscs in the present case healed completely within seven weeks under consistent therapy with Infectodell® (Fig. 2). Another therapeutic option is the topical application of the immunomodulator Imiquimod (Aldara®), although response rates vary widely and treatment costs are high [5]. In children with extensive mollusc infestation, e.g., in the setting of immunodeficiency, painless topical application of cidofovir solution (a nucleotide analogue) has proven effective, although this is associated with considerable cost [6].

Lisa Weibel, MD
Regula Wälchli, MD
Martin Theiler, MD
Med. pract. Alexandra Smith
Literature:
- Brown J, et al: Childhood molluscum contagiosum. Int J Dermatol 2006; 45: 93-99.
- Kim SK, et al: Giant molluscum contagiosum of immunocompetent children occurring on the anogenital area. Eur J Dermatol 2007; 17(6): 537-538.
- Erdmann SM, et al: Molluscum contagiosa in an infant with atopic eczema: a therapeutic challenge. Dermatologist 2004; 55(10): 991-994.
- Short KA, et al: Double-blind, randomized, placebo-controlled trial of the use of topical 10% potassium hydroxide solution in the treatment of molluscum contagiosum. Pediatr Dermatol 2006; 23(3): 279-281.
- Katz A, et al: Imiquimod is not an effective drug for molluscum contagiosum. The Lancet infectious diseases 2013; 13(10): 877-880.
- Briand S, et al: 1% topical cidofovir used as last alternative to treat viral infections. J Eur Acad Dermatol Venereol 2008; 22(2): 249-250.
DERMATOLOGIE PRAXIS 2014; 24(3): 34-35