Cough is among the most common reasons for consultation in the family practice. When evaluating patients with chronic cough, a careful history and assessment of findings is critical. However, in 10-40% of cases, the cause remains unclear after differential diagnostic evaluation. A multimodal treatment strategy is recommended for this clientele. There are interesting new developments in the field of drug therapy options.
The DEGAM* recommendations for the diagnosis and treatment of cough without explainable causes or of cough refractory to therapy, updated in 2021, are intended to provide decision support for a structured procedure that is transparent for patients [1]. This corresponds to a current need. In a European Internet survey of chronic cough, only one-third of patients felt thoroughly examined, and less than 10% were satisfied with the outcome of drug treatment. More than 90% of patients reported feeling frequently depressed and joyless because of the cough. The majority of respondents wanted more information, especially on causes and therapeutic approaches [2].
* DEGAM=German Society of General Practice and Family Medicine
Have all differential diagnoses and “red flags” been excluded?
According to the current nomenclature, cough that persists for at least 8 weeks is defined as “chronic cough” [1]. The most common causes are asthma, UACS (upper airway cough syndrome), GERD (gastroesophageal reflux) or bronchiectasis [3]. If no cause for the cough is found despite a structured diagnostic approach, it is unexplained chronic cough (UCC) [4]. A cough is said to be refractory when treatment of one or more suspected causes of the cough has failed to bring improvement. Because common assessment algorithms include probationary therapies, it is difficult to make a clear distinction.
Smoking history to exclude chronic (obstructive) bronchitis or bronchial carcinoma should also include e-cigarettes/nebulizers, as these are also suspected of irritating cough receptors and inducing cough [5]. The use of cannabis should also be questioned – in contrast to tobacco, cannabis has a bronchodilating effect, but cannabis smokers cough more frequently and often complain of shortness of breath, wheezing and chest pain [6,7].
Other important anamnestic questions concern the use of medications (especially ACE inhibitors), known allergies or allergen exposures, and travel [4]. After exclusion of “red flags” (Tab. 1) or indications of a preventable dangerous course, a chest X-ray in two planes is recommended for further diagnosis after the physical examination [1,8]. In patients taking ACE inhibitors and with cough at low risk for causative pulmonary disease, discontinuation/adjustment of the ACE inhibitor may be performed prior to radiographic examination. Depending on the suspected diagnosis, further diagnostic investigations should be considered (e.g. CT, spirometry, bronchoscopy).
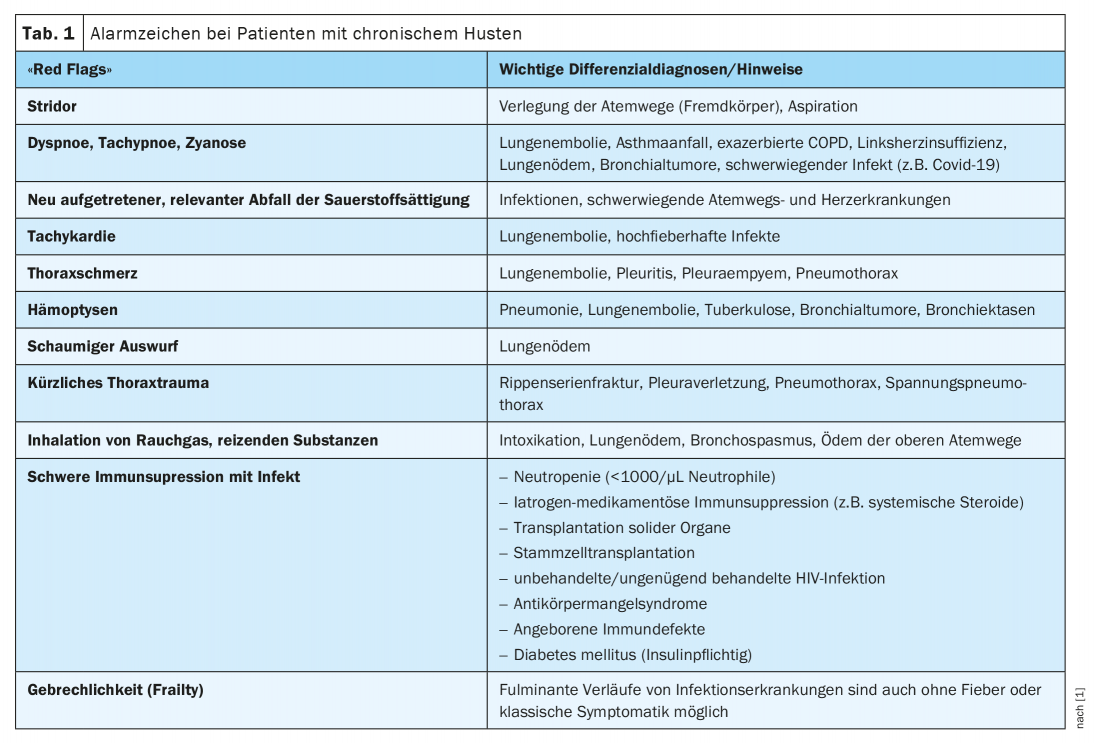
If the cough persists for a long time, there is a particular risk of overlooking diseases that need to be clarified promptly. The following dangerous courses should be recognized or excluded [1].
- Small recurrent pulmonary emboli: sometimes difficult to recognize, more common in patients with diseases of the coagulation system and malignant diseases, dominant symptom is exertional dyspnea and rapid fatigue.
- Left heart failure: known cardiac disease is a risk factor, characteristic is dyspnea on exertion up to orthopnea, affected persons often have leg edema.
- Neoplasms: especially in smokers, often accompanied by unwanted weight loss, night sweats, decreased performance, hemoptysis, chest pain, hoarseness.
- Foreign body aspiration: possible cause of prolonged cough, especially in children and the elderly.
- Lower respiratory tract infections due to chronic aspiration: especially patients after stroke or with chronic neurological diseases are at risk, characterized by chronic microaspiration of saliva and food,
Interdisciplinary, multimodal treatment concept recommended
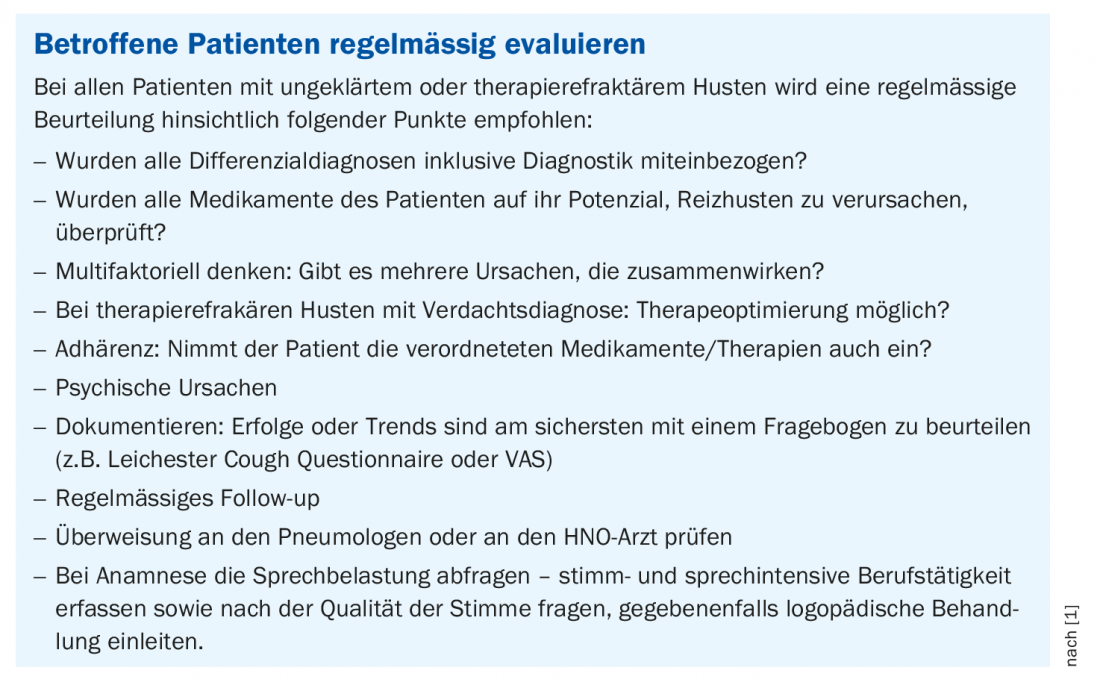
In up to 40% of patients with chronic cough, the cause remains unclear [3]. The patients in question should be educated that an unproductive, chronic cough is physiologically unnecessary and causes further cough irritation, so trigger factors (e.g., dry air, smoke, or other irritants) should be avoided. In order to reduce the increased urge to cough as well as a compulsion to clear one’s throat, accompanying physiotherapeutic and speech therapy treatment may be useful, in which cough suppression techniques and breathing exercises are taught [88]. Inhaling with salt water can also reduce coughing and throat clearing by decreasing dehydration of the airways [9,10]. Because patients with unexplained or refractory cough more often have high psychological distress, increased nervousness, and symptoms of depression, complementary psychotherapeutic treatment may be helpful in individual cases [9,11,12].
Newly approved antitussive: favorable risk-benefit profile
Regarding pharmacotherapy, guidelines recommend a trial of low-dose morphine, gabapentin, pregabalin, or amitriptyline. However, these therapeutic options often do not work satisfactorily. The agents codeine and noscapine have not been studied for refractory cough [1].
Gefapixant (Lyfnua®), a novel antitussive from the P2X3 receptor antagonist group, was recently approved in Switzerland [2,13]. Gefapixant (45 mg, 2×/d) is available in oral dosage form (tablet) and is the first active agent to demonstrate high efficacy and an acceptable safety profile in refractory chronic cough or unexplained chronic cough in Phase III clinical trials [14]. The number of cough attacks was shown to be reduced. The results of the randomized-controlled, double-blind, parallel-group COUGH-1 and COUGH-2 studies were published in the journal Lancet Respiratory Medicine . COUGH-1 was conducted at 156 sites in 17 countries and COUGH-2 at 175 sites in 20 countries. Individuals over 18 years of age who had been diagnosed with refractory chronic cough or unexplained chronic cough of at least one year’s duration were eligible to participate. Both of these studies met the primary endpoint of significantly reduced cough frequency at 24 h.
Literature:
- DEGAM-S3 guideline “acute and chronic cough”, 2021, (DEGAM) www.awmf.org/uploads/tx_szleitlinien/053-013l_S3_akuter-und-chronischer-Husten_2022-01.pdf, (last accessed 22.07.2022).
- Chamberlain SA, et al: The impact of chronic cough: a cross-sectional European survey. Lung 2015; 193(3): 401-408.
- Bürgi U: Cough in the adult, 2021, www.luks.ch, (last accessed 07/22/2022).
- Gibson P, et al: Treatment of Unexplained Chro nic Cough: CHEST Guideline and Expert Panel Report. Chest 2016; 149(1): 27-44.
- Chung S, et al: Electronic Cigarette Vapor with Nicotine Causes Airway Mucociliary Dysfunction Preferentially via TRPA1 Receptors. Am J Respir Crit Care Med 2019; 200(9): 1134-1145.
- Ribeiro LI, Ind PW: Effect of cannabis smoking on lung function and respiratory symptoms: a structured literature review. NPJ Prim Care Respir Med 2016; 26(1): 1-8.
- Davis GP, Gunderson E: Evaluation of chronic cough should consider cannabis use. Am Fam Physician 2012; 85(7): 680.
- Irwin RS, et al; CHEST Expert Cough Panel: Classification of Cough as a Symptom in Adults and Management Algorithms: CHEST Guideline and Expert Panel Report. Chest 2018; 153(1): 196-209.
- Vertigan AE, et al: Efficacy of speech pathology management for chronic cough: a randomised placebo controlled trial of treatment efficacy. Thorax 2006; 61(12): 1065-1069.
- Patel AS, et al: Improvement in health status following cough-suppression physiotherapy for patients with chronic cough. Chron Respir Dis 2011; 8(4): 253-258.
- Birring SS: Controversies in the evaluation and management of chronic cough. Am J Respir Crit Care Med 2011; 183(6): 708-715.
- Hulme K, et al: Psychological profile of individuals presenting with chronic cough. ERJ Open Res 2017; 3(1).
- Authorization of a medicinal product with a new active substance: Lyfnua®, film-coated tablets (Gefapixantum), Swissmedic Journal 5/2022
- McGarvey LP; COUGH-1 and COUGH-2 Investigators. Efficacy and safety of gefapixant, a P2X3 receptor antagonist, in refractory chronic cough and unexplained chronic cough (COUGH-1 and COUGH-2): results from two double-blind, randomised, parallel-group, placebo-controlled, phase 3 trials. Lancet 2022; 399(10328): 909-923.
HAUSARZT PRAXIS 2022; 17(8): 36-37