The causes of medullary changes of the vertebrae are manifold. Inflammatory, tumorous and traumatic noxae as triggers usually lead to spongiosaedema. In the context of degenerative vertebral conditions, spongiosaedema, fatification or sclerosis can be documented in terms of image morphology. MR tomography in particular is the method of choice here.
The degenerative lesions of the vertebral medulla are almost always accompanied by degenerative disc changes and are the result of fissures of the interfaces with resulting spongiosa edema or sprouting of fibrovascular tissue [1]. Here, the cortical interfaces appear intact on imaging studies in contrast to spondylodiscitis, which is associated with bony changes, specifically destruction of the vertebral endplates. Chronic and acute medullary changes can also be detectable simultaneously and multisegmentally [2,3]. The changes can occur in the cervical, thoracic and lumbar spine, primarily lumbar. The extent of degeneration and the load determine the symptomatology, which can be lumbalgiform or lumboischialgiform of varying intensity.
Cancellous edema due to trauma can also occur after spinal contusions, after whiplash as a result of segmental compression, or in connection with fractures (e.g., osteoporotic sintering). These bone marrow responses, also named “bone bruise” [4], visualize trauma-induced bone marrow edema, blood components, microtrabecular fractures, and also already initial reparative processes with fibrovascular tissue formation. An accurate history indicates the type of traumatic changes to expect.

Computed tomography is a good way to assess degenerative changes in the intervertebral discs, spondyloses and spondyloarthroses. However, compared with MRI, CT has significant deficits in detecting stress-related medullary changes, such as cancellous bone edema. However, pure fracture diagnosis remains the domain of radiography and CT in particular, but radiologically occult (microtrabecular fractures) are only detected by MRI [4] or as nonspecific findings by skeletal scintigraphy.
Magnetic resonance imaging examinations in skeletal diagnostics as well as other organ regions of the human body were appreciated soon after their introduction into clinical routine. The noninvasive differentiation of inflammation of the skeletal system was a major advantage of the method, in addition to the multiplanar visualization of pathologic processes and the lack of radiation exposure [5].
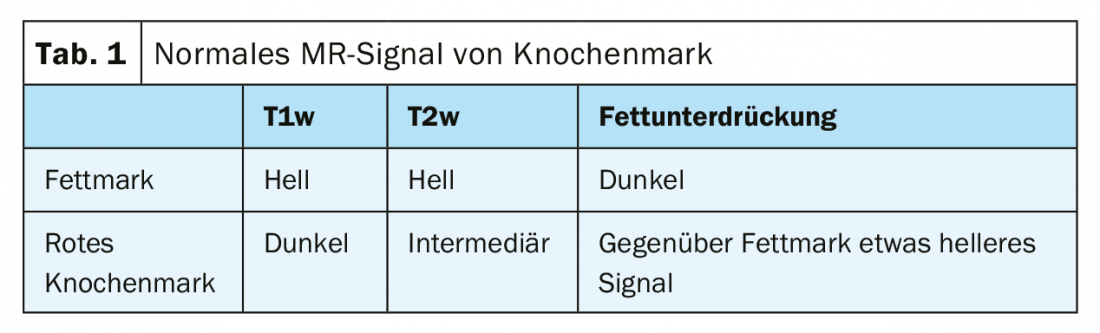
Normal bone marrow shows a fat-equivalent signal in adults (Table 1), and red bone marrow is differentiable [6]. Intravenous contrast agent application does not reveal any relevant signal change in the healthy medullary cavity [7], and the edematous altered cancellous bone areas show an increase in signal regardless of causa.
The spreading pattern of pathologic medullary changes may well be pathognomonic, especially also in the case of diffuse seeding of lesions in the context of tumorous including hematologic underlying diseases. Inflammatory diseases must be differentiated. If trauma has occurred and there are clear clinical symptoms, MRI is indicated for radiographic visualization of occult fractures with “bone bruise.” This applies to the trunk skeleton as well as to the skeletal periphery [8].
The degenerative changes of the spinal segments sum intervertebral disc changes and bony reactions, which in the acute stage are accompanied by subchondral spongiosa edema, and in the chronic stage by subchondral spongiosa fatty degeneration [6,9]. These then exhibit signal amplification in T1w and T2w sequences, verified by signal depression in fat-suppressed measurements. Bone appositions at the vertebral endplates in the context of spondylosis deformans and also facet joint arthroses are often detectable.
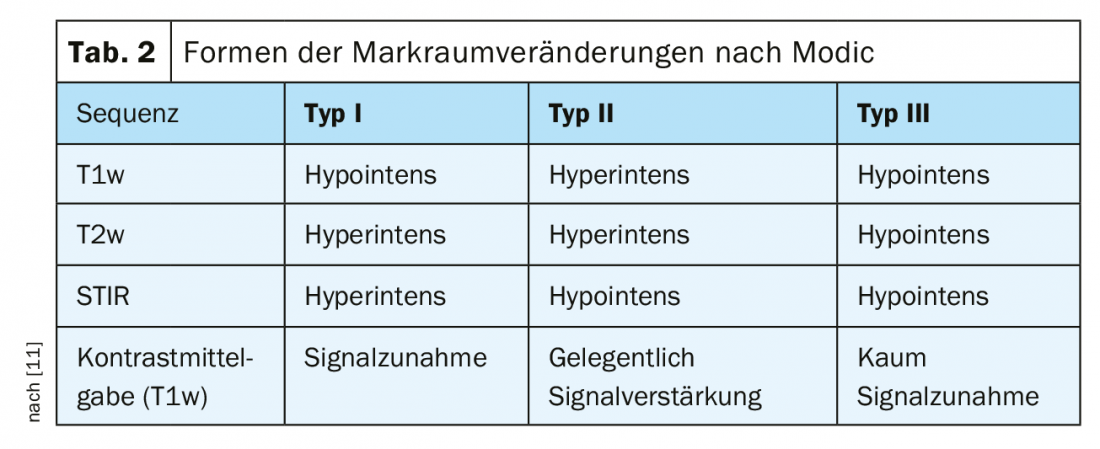
3 types of medullary changes, classified by Modic [10], can be distinguished (Table 2), which have characteristic features in T1w and T2w sequences [1].
Literature:
- Burgener FA, Meyers SP, Tan RK, Zaunbauer W: Differential diagnosis in MRI. Stuttgart, New York: Georg Thieme Verlag 2002; 314.
- Erlemann R, Hoogeveen A: Spondylitis and its differential diagnoses. Radiology up2date 2; 2012; 12: 163-184.
- Marshman LA, Metcalfe AV, Krishna M, Friesem T: Are high-intensity zones and modic changes mutually exclusive in symptomatic lumbar degenerative discs? J Neurosurg Spine 2010; 12(4): 351-356.
- Breitenseher M: The MR-Trainer Lower Extremity. Stuttgart, New York: Georg Thieme Verlag 2003; 28.
- Paushter DM, et al: Magnetic resonance. Principles and applications. Mes Clin North Am 1984; 68(6): 1393-1421.
- Sartor K: Neuroradiology, Stuttgart, New York: Georg Thieme Verlag, 2nd completely revised and expanded edition 2001; 330.
- Brambs, H.-J. (Ed.): Radiology Update ’04. mpm Pohlheim 2004; 11.
- Rummeny EJ, Reimer P, Heindel W (eds.): Whole-body MR tomography. Stuttgart, New York: Georg Thieme Verlag 2002; 579.
- Thiel HJ: Cross-sectional diagnosis of the spine (1.10). Medullary changes of the spine. MTA Dialog 2010; 11: 966-968.
- Boisson M, et al: Active discopathy: a clinical reality. RMD Open 2018; 17: 4(1):e000660
- Stoller DW: Magnetic resonnce imaging in orthopaedics and sports medicine. Volume two – upper extremity. Baltimore: Lippincott Williams&Wilkins, 3rd edition, 2007: 1980-1982.
GP PRACTICE 2020; 15(2): 30-32











