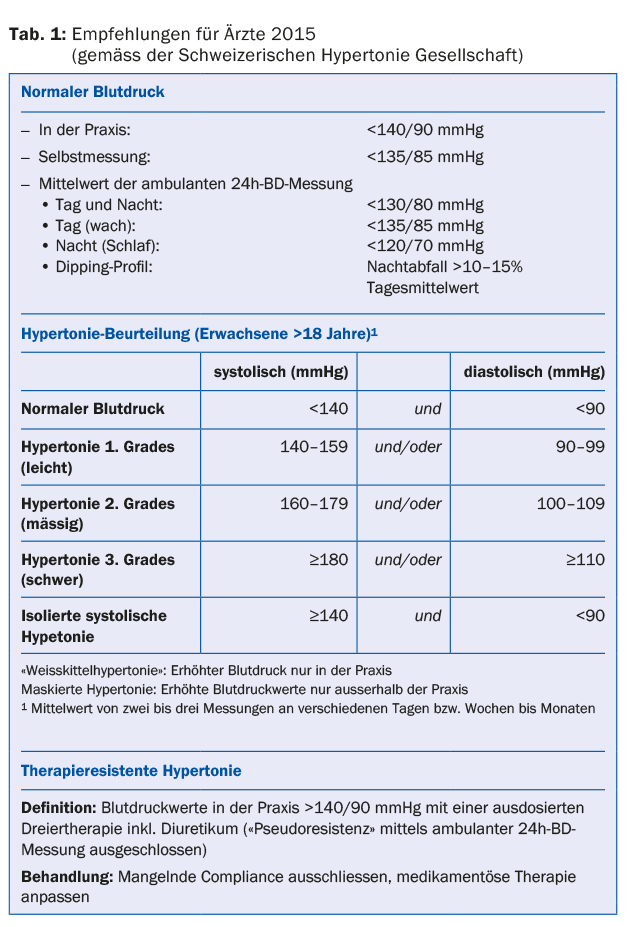
The definition of refractory hypertension is very precise (tab. 1): Blood pressure in the physician’s office is >140/90 mmHg despite triple combination therapy in appropriate dosage (including a diuretic). In the case of a patient diagnosed with hypertension who has elevated blood pressure values on subsequent checks despite prescription of antihypertensives, it is better to speak of “difficult-to-control hypertension” or “pseudoresistant hypertension”. Some controls are needed to exclude “pseudoresistance”: “white drug effect”, lack of compliance, inadequate dosage, other factors such as concomitant medication, excessive alcohol consumption, sleep apnea. So-called secondary hypertension must also be ruled out. Only after all the above-mentioned influencing factors have been excluded can the patient’s condition be described as “therapy-resistant arterial hypertension” and special therapeutic strategies considered, which belong exclusively in the hands of the specialist.
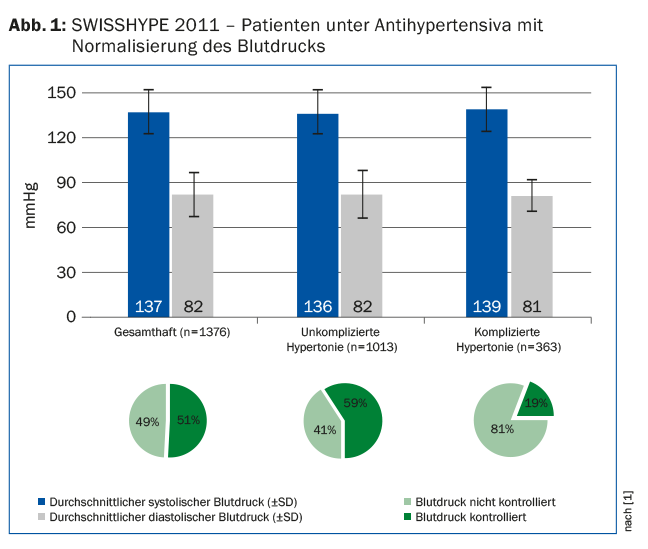
Considering that hypertension is one of the major risk factors for cardiovascular morbidity and mortality, the therapeutic goal is logically to reduce elevated blood pressure to normal levels. The SWISSHYPE study (Fig. 1) [1] shows that blood pressure values measured in the physician’s office were <140/90 mmHg in only 49% of hypertensive patients treated. Consequently, about half of adults treated for hypertension with medication do not reach the blood pressure levels recommended in national and European guidelines.
Carlo C., male, 48 years old
Carlo, smoker, is a cashier in a supermarket, BMI 29. He measured his blood pressure in a pharmacy: 150/96 mmHg. In the family practice, blood pressure values were 165/105, 160/102, 155/100 mmHg when measured three times. The physician suggests starting drug therapy (monotherapy). Control after four weeks: RR 168/104, 160/102, 158/100. Why haven’t Carlo’s blood pressure readings normalized?
Hypertension: methodological approach
Blood pressure measurement is the most common routine medical procedure in every family practice. The measurement technique requires a note: If one wants to confirm or exclude elevated values and thus hypertension, it is imperative to follow the guidelines for correct blood pressure measurement listed in the guidelines (Tab.2). These apply both in the doctor’s office and in any other location (home, other non-medical environment).
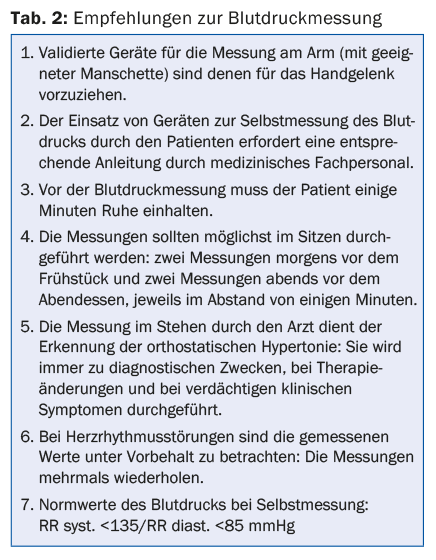
Measurement by auscultation using a stethoscope is now preferred to oscillometric measurement by validated automated devices. Among other things, these have the advantage that they can be given to the patient to take home.
Conclusion: Elevated blood pressure values measured during a medical examination must be controlled. Only after a correct blood pressure measurement and a sufficient number of measurements can one confirm or exclude that the patient’s values are elevated. Approximately 15-30% of patients with an elevated value during a medical examination actually have absolutely normal blood pressure values during subsequent checks under suitable conditions (“white coat effect”).
Self-measurement and ambulatory (24h) BP measurement
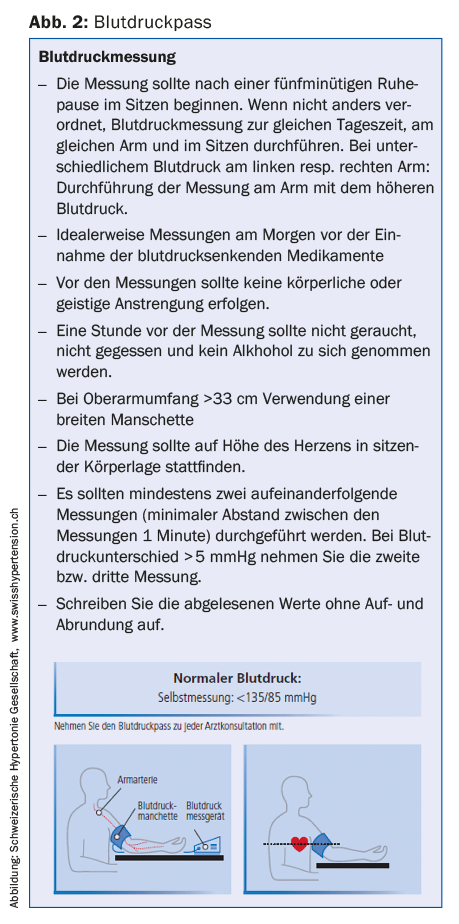
Thanks to modern automated oscillometric devices for blood pressure measurement, anyone who wants to can easily measure blood pressure themselves. However, it is essential to follow the instructions for correct self-measurement (Fig. 2) . To check whether one’s own blood pressure values are normal or elevated, it is recommended to take a measurement in the morning and in the evening for one week and then visit the family doctor.
Ambulatory BP measurement is an important and indispensable complement to self-measurement by the patient. It enables the recording of blood pressure fluctuations during the day and, in particular, blood pressure behavior during the night’s rest (Fig. 3) . It is a very important diagnostic tool, indicated both for the diagnosis of hypertension and for checking the effectiveness of antihypertensive therapy.
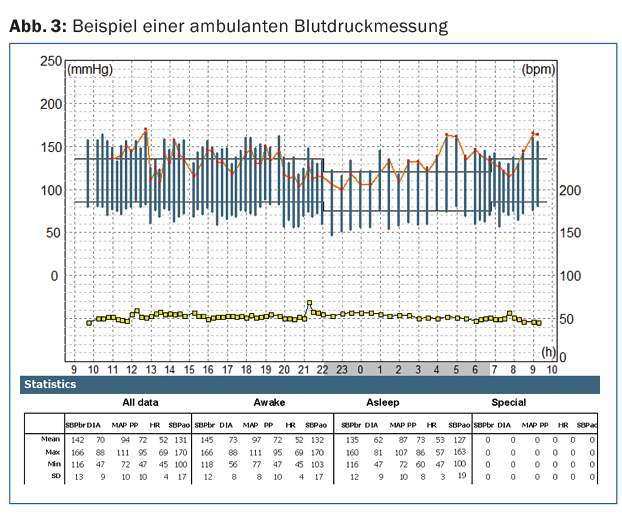
CONCLUSION: To confirm the diagnosis of hypertension, a sufficient number of correctly and guideline-conforming blood pressure measurements over several weeks as well as an ambulatory 24-h BP measurement must be available, as this allows the recording of blood pressure fluctuations during the day and during the night’s rest as well as a review of the effectiveness of antihypertensive therapy.
The case of Carlo C.
Assuming that the necessary checks were carried out on Carlo C. to confirm the diagnosis of hypertension, the following question must be asked: Does Carlo really have elevated blood pressure values despite therapy? It is well known that patients who are being treated for hypertension with medication can also exhibit the so-called “white coat reaction”. This phenomenon occurs in 15-30% of the non-hypertensive general population. A small study conducted using 24-h ambulatory BP measurement showed that one in three antihypertensive patients whose BP was elevated in the physician’s office actually had normal values over a 24-h period [2].
Conclusion: Patients who still have elevated blood pressure values when measured in the general practitioner’s office while on antihypertensive drug treatment must perform another week of self-measurement at home according to the guidelines. In addition, it is recommended to perform 24-h ambulatory BP measurement to check the variability of BP and, in particular, the normal nocturnal BP drop (prognostic value for nocturnal “dipping”).
Is Carlo’s drug therapy sufficient to normalize blood pressure levels? It is correct to speak of “difficult-to-control hypertension” when blood pressure values do not normalize under combination therapy with three different antihypertensive substance classes. “Therapy-resistant hypertension” is defined as blood pressure that remains >140/90 mmHg in the physician’s office despite triple combination therapy at appropriate doses (including a diuretic and after exclusion of pseudotherapy resistance by 24h ambulatory BP measurement).
Conclusion: A single drug rarely achieves normalization of blood pressure values. Thanks to well-tolerated and combinable substances, we now have combination drugs that simplify daily dosing (one tablet – two or three active ingredients). The guidelines specify when and how to apply this strategy. If normalization of blood pressure values is not possible with an adequate triple drug combination, the advice of a blood pressure specialist should be sought.
Is Carlo actually taking the prescribed medication? This is certainly the most important aspect: no drug, no effect. An infallible (but expensive!) method to prove whether the patient has really taken the drug is to detect the substance in the urine. In a hypertension clinic on the other side of the Atlantic, this trick has succeeded in demonstrating that half of the patients referred for consultation for refractory hypertension had not taken all or part of the prescribed medication [3]. It is important to convince patients of the benefits that are undoubtedly obtained by normalizing blood pressure: Only regular use of the medication ensures a good cardiovascular prognosis. The clinical trial conducted over approximately six years with approximately 250,000 patients in Lombardy [4] showed that hypertensive patients with good adherence to therapy reduced the risk of cardiovascular complications by 37%.
CONCLUSION: In practice, the efficacy of an antihypertensive drug can be easily determined by administering it directly to the patient and checking the effect in the following hours by means of ambulatory short-term BP measurement (four to six hours). Adherence to therapy can also be checked with the help of the pharmacist: How many packs of the prescribed medication were picked up in the course of three to six months after the doctor prescribed it?
Is Carlo perhaps taking other substances that interfere with the antihypertensives? Many commonly used substances (drug and non-drug), often dispensed over-the-counter, can affect antihypertensives and reduce their effectiveness. Particularly insidious are harmless-acting substances such as cold remedies (nose drops, drinks against flu) or “natural” slimming pills. NSAIDs are a classic example of drugs with a significant “hypertensive” effect. Antidepressants can also produce a similar effect.
Conclusion: It is important to regularly ask patients how many and which substances with pharmacological properties they spontaneously ingest. Magazines and the Internet are inexhaustible sources of (supposed) health tips and tricks. If possible, they should have the original packaging they purchased brought to them. The patient’s therapeutic regimen and interactions should be reviewed regularly.
…and if Carlo has secondary hypertension? In adequately treated patients whose blood pressure is difficult to adjust on repeated checks, one should think of clarifying secondary hypertension. Occasionally, these are conditions in addition to primary hypertension. One should think of three possible causes.
- Chronic kidney disease: It is easily clarified by appropriate laboratory tests.
- Sleep apnea: It is increasingly diagnosed in non-adipose patients. In this context, the anamnesis is most important in order to initiate an appropriate specialist examination.
- Excess aldosterone (primary hyperaldosteronism). This cause is more common than was thought in the past.
CONCLUSION: When there is a reasonable suspicion of secondary hypertension, the patient should be referred directly to a hypertension specialist in order to use the time and resources to best treat the patient.
Literature:
- Brenner R, Waeber B, Allemann Y: Medical treatment of hypertension in Switzerland. The 2009 Swiss Hypertension Survey (SWISSHYPE). Swiss Med Wkly 2011 Mar 4; 141: w13169.
- Tschudi P, Martina B: False non-response in hypertension treatment in family practice. PRAXIS 2008; 97: 543-547.
- Weber M: MY APPROACH to the Patient With Hard-To-Control Hypertension. Expert Opinion/My Approach 2015 January 06.
- Mancia G, et al: Better compliance to antihypertensive medications reduces cardiovascular risk. Journal of Hypertension 2011; 29: 610-618.
HAUSARZT PRAXIS 2016, 11(3): 20-23











