Practical strategies for treatment management of metastatic renal cell carcinoma (mRCC) were presented at the ESMO Congress in Amsterdam. Updates on current clinical trials and the utility of new treatment options were discussed in light of current treatment modalities that still need improvement. Different mechanisms of action were presented.
(ag) Christian Kollmannsberger, MD, from the University of British Columbia, Canada, opened the symposium with an overview of the current treatment of metastatic renal cell carcinoma (mRCC): “While we have made many advances in the therapy of this disease. We understand the underlying biological processes better and we can thus target the relevant pathways [1]. Nevertheless, the current treatment approach is not curative, i.e., we cannot cure the disease [2]. The median progression-free survival is 8-12 months in the first-line setting. After administration of VEGF inhibitors, the median rate is four to five months in the second-line setting. Currently, therefore, we are working to develop new strategies to optimize therapy based on a more detailed understanding of the molecular pathways involved in drug resistance.”

What should the therapy target?
Clear cell renal cell carcinoma (ccRCC) is by far the most common form of all RCCs, accounting for approximately 75% of cases. This condition in turn almost always (90% of ccRCC) has a genetic characteristic, namely a mutation in the Von Hippel-Lindau tumor suppressor gene (VHL) [3]. The VHL/HIF axis appears to be crucial in ccRCC: the inactivated VHL protein (pVHL) can no longer perform its functions correctly. Sometimes this deregulates HIFα expression, which in turn stimulates various growth factors (“GFs”) and thus contributes fundamentally to the pathogenesis of ccRCC. A growth factor that has been known for some time is VEGF [4].
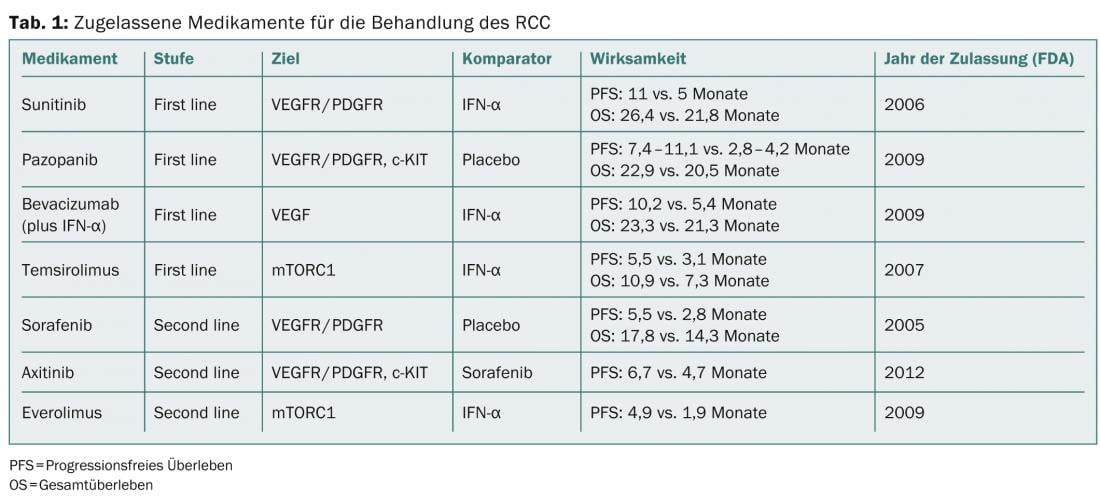
Agents that interfere with one or more mechanisms of HIFα overexpression or its effects, for example by inhibiting a GF, have been investigated in various studies and are also approved in Switzerland. A list of currently available drugs in RCC treatment is shown in Table 1.
Resistance
“With antiangiogenic drugs, however, adaptive or intrinsic resistance occurs sooner or later. The first form develops in the course of treatment, while the second has existed since the beginning,” Kollmannsberger explained. “So either patients experience benefit first and then disease progression. This is true for about 80% of patients. Or they don’t respond to therapy at all and face rapid deterioration and a poor prognosis. This happens in about 20% of patients.”
In everyday clinical practice, adaptive (evasive) resistance can be observed more frequently. The mechanisms of this resistance are becoming increasingly clear. Several processes seem to be involved in the intrinsic form:
- It is possible that the tumor has supernumerary proangiogenic signaling pathways from the beginning. These could further maintain angiogenesis, even after inhibition of VEGF signaling.
- Furthermore, the presence of myeloid cells producing proangiogenic factors could contribute to intrinsic resistance.
If tumors become progressive after initial treatment success (adaptive resistance), upregulation of proangiogenic factors, e.g., by new signaling pathways or the use of alternative VEGF ligands, plays a role. The tumor adapts to inhibition of angiogenesis, which may also mean that it uses the normal vasculature of surrounding tissues to be less dependent on VEGF signaling.
Ways to counteract resistance are as follows [5]:
Dose adjustment: there is debate as to whether stepwise increasing dosing is an optional second-line therapy. However, benefit appears to be seen only in those patients who tolerate the higher doses.
Combination therapy: In the future, a combination of different agents targeting the diverse pathways involved in angiogenesis, including VEGFR, PI3K and mTORC1/2, would be possible [6]. However, toxicity problems could occur.
Switching to another agent: Consideration is given to switching to an agent that has either the same or a different mechanism of action. This is because cross-resistance is not always to be expected.
What’s next?
“Treatment response in mRCC is not durable, so patients eventually relapse with currently available targeted treatment modalities,” Kollmannsberger summarized. “This makes it all the more important to have a suitable sequence logic in the administration of the approved drugs. This can increase the success of therapy.” New agents targeting different pathways involved in this condition and its high resistance are being explored.
“Tumors develop alternative signaling pathways to re-initiate angiogenesis, such as the FGF pathway. Addressing this effectively, for example with a tyrosine kinase inhibitor (TKI), may result in longer survival rates. Studies show a potential benefit of third-line therapy for patients with progression. Further research in this area is ongoing. Immunotherapies are also being investigated in the context of therapy resistance,” Viktor Grünwald, MD, from the Medical School Hannover, Germany, concluded the lecture series.
Source: ESMO Congress, 27 September to 1 October 2013, Amsterdam
Literature:
- Rini BI: New Strategies in Kidney Cancer: Therapeutic Advances through Understanding the Molecular Basis of Response and Resistance. Clin Cancer Res March 1 2010; 16: 1348-1354; Published OnlineFirst February 23, 2010; doi:10.1158/1078-0432.CCR-09-2273.
- Sonpavde G, Choueiri TK: Biomarkers: the next therapeutic hurdle in metastatic renal cell carcinoma. Br J Cancer 2012 Sep 25; 107(7): 1009-1016. doi: 10.1038/bjc.2012.399. Epub 2012 Sep 4.
- Audenet F, et al: Genetic pathways involved in carcinogenesis of clear cell renal cell carcinoma: genomics towards personalized medicine. BJU Int 2012 Jun; 109(12): 1864-1870. doi: 10.1111/j.1464-410X.2011.10661.x. Epub 2011 Oct 28.
- Shen C, Kaelin WG: The VHL/HIF axis in clear cell renal carcinoma. Semin Cancer Biol 2013 Feb; 23(1): 18-25. doi: 10.1016/j.semcancer.2012.06.001. Epub 2012 Jun 13.
- Ravaud A, Gross-Goupil M: Overcoming resistance to tyrosine kinase inhibitors in renal cell carcinoma. Cancer Treat Rev 2012 Dec; 38(8): 996-1003. doi: 10.1016/j.ctrv.2012.01.003. Epub 2012 Feb 12.
- Figlin RA, et al: Targeting PI3K and mTORC2 in metastatic renal cell carcinoma: new strategies for overcoming resistance to VEGFR and mTORC1 inhibitors. Int J Cancer 2013 Aug 15; 133(4): 788-796. doi: 10.1002/ijc.28023. epub 2013 Feb 12.
InFo Oncology & Hematology 2014; 2(1): 42-44.