During sports, many body functions work at a higher level. The blood flow to the working muscles and the composition of the blood also change. In this context, iron plays a central role in the body.
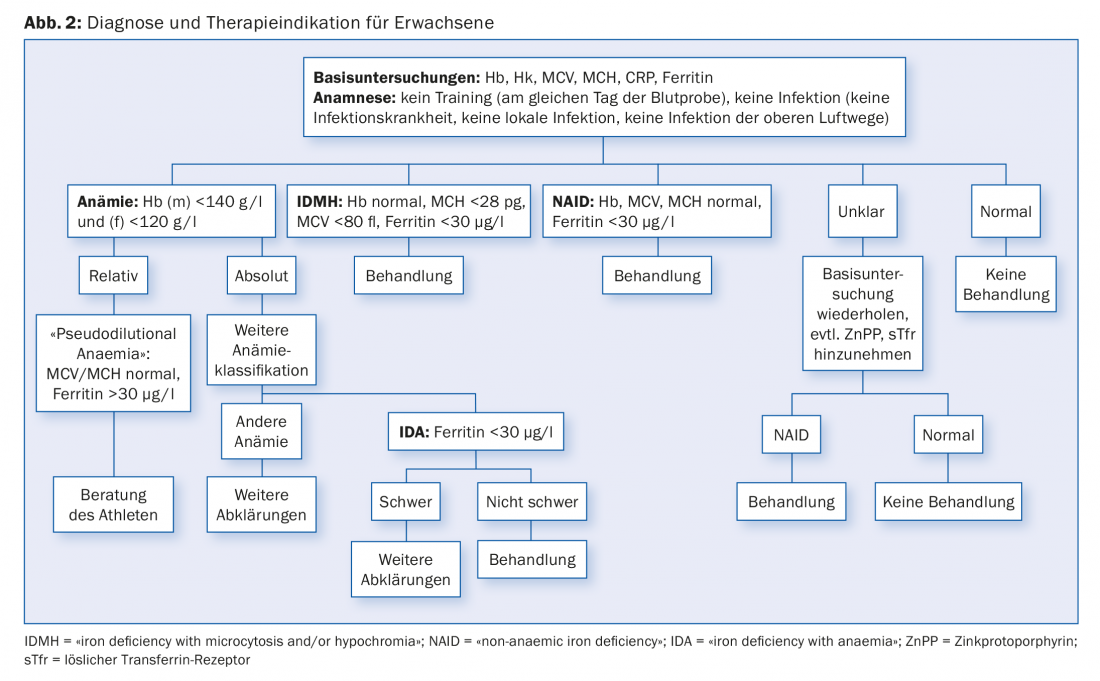
The impressive increase in blood flow to the working muscles by a factor of almost 20 occurs via various adaptation mechanisms: of crucial importance is an increase in cardiac output (Fig. 1). On the one hand, there is an increase in stroke volume (amount of blood carried in one heartbeat), and on the other hand, there is an increase in heart rate. Stroke volume is increased from about 60 ml to just over 100, while heart rate is increased from about 60 to up to 200 beats per minute.
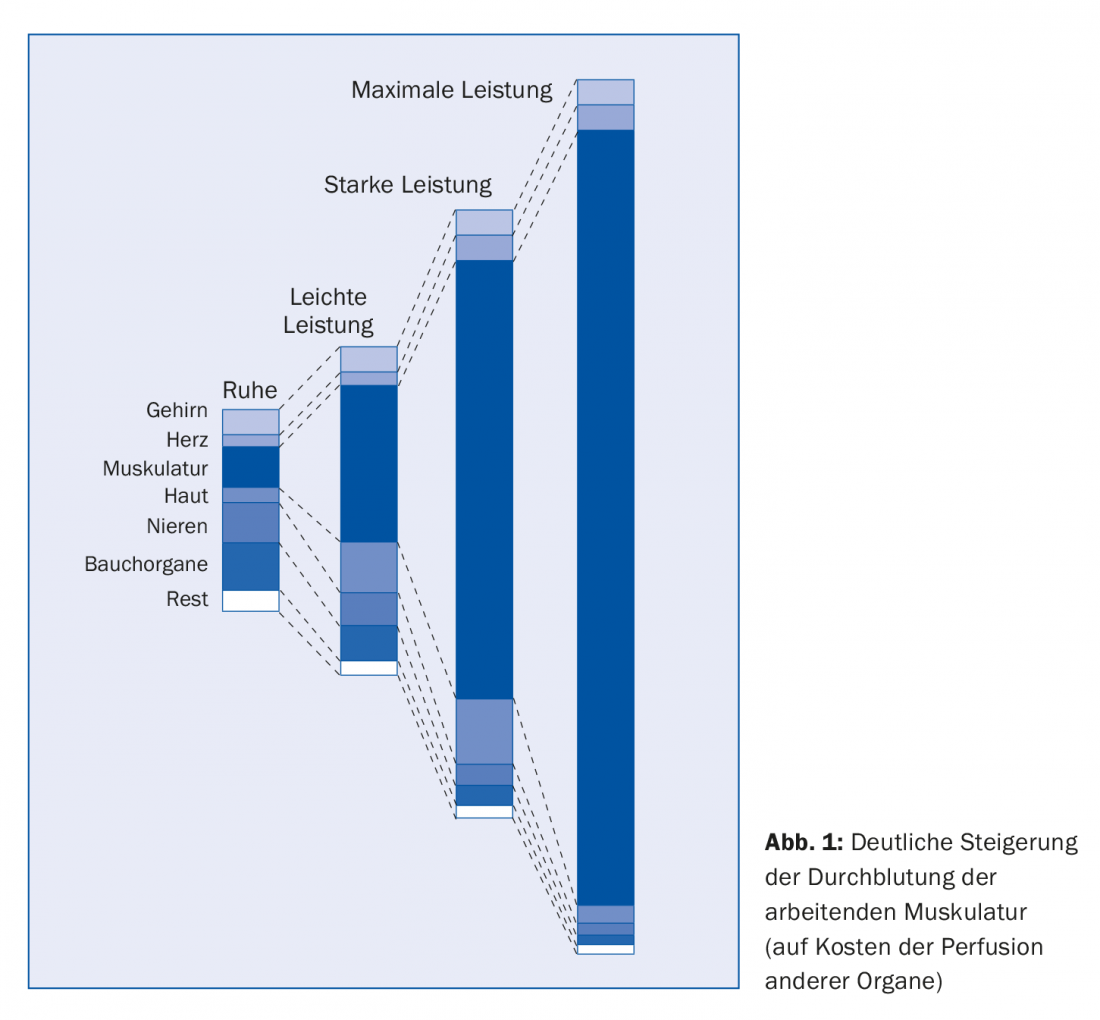
Figure 1 shows that this matched organ perfusion (in ml/min) occurs at the expense of perfusion of other organs during high exercise. It also increases the blood pressure and thus achieves an optimal adaptation of blood circulation to the required performance. This is further facilitated by an increase in the active circulating blood volume. As a result, the working tissue can be supplied with more energy-providing substrates and metabolic waste products can be removed.
The increase in the heart’s pumping capacity is also associated with accelerated and deepened breathing, so that the conditions for oxygen transport and thus the supply of oxygen to the organism are significantly improved. The increase in oxygen uptake is accompanied by the facilitation of oxygen delivery to muscle tissue. The increased body temperature facilitates the delivery of oxygen from red blood cells to muscle tissue by shifting the oxygen dissociation curve to the right. For this, the blood must be “in the best condition”.
Blood adjustments
The blood itself therefore also adapts to physical stresses, in the short term and in the long term. The first changes touch the blood plasma. With the beginning of physical work, there is an increase in body temperature, the regulation of which occurs with a shift of water from the intravascular to the extravascular space of up to 10%. Plasma volume decreases, there is a temporary “blood thickening” (relative increase in blood cells). As a result of this hemoconcentration, hormonally mediated (aldosterone, ADH) fluid retention occurs and after sufficient exercise time, especially in the endurance range, plasma volume increases up to 20%. At the same time, an increase in erythropoiesis leads to an increase in erythrocyte mass. However, since this is relatively smaller than the increase in plasma volume, a tendency for a relative decrease in hemoglobin and hematocrit levels is observed.
As a further consequence, the overall viscosity of the blood is reduced as well as the aggregation tendency of the erythrocytes, which first of all show an improved deformability. These improvements in flow properties also contribute to improved tissue perfusion in the exercised person.
Pseudoanemia
It is important to know these adaptation phenomena of the blood in connection with the training, because, for example, the pseudoanemia caused by the sport does not require treatment in any way. This is despite the fact that in the sports medicine literature, physiological adaptations are misleadingly found under the term “athletic anemia” (“athletic pseudo anemia”).
Blood tests in sport
It should be noted at this point that routine measurements of hemoglobin and hematocrit do not give any indication of the amount of oxygen transport actually present in the organism. In fact, they tend to be unreliable in endurance sports. Today, there is a determination method, the “optimized CO rebreathing method”, which allows a reliable determination of the total hemoglobin mass, the total blood volume, the total erythrocyte volume, the total plasma volume as well as the relative values of these parameters (in relation to the body weight) in a not very complex way. These values reflect training effects much more accurately (they can also be used to detect blood manipulation).
In sports medicine, e.g. on the occasion of the sports medical examination (SPU), blood samples are taken. Among other things, this includes the measurement of hemoglobin, hematocrit and the characterization of erythrocytes in terms of size (MCV) and hemoglobin content (MCH), as well as the determination of the storage iron ferritin and C-reactive protein. With these inexpensive first values, one already approaches the diagnosis “anemia”, provided that the blood analysis was not performed just after a hard workout (wait at least 24 hours). And as we have seen, anemia is simply not in the cards for those seeking peak performance.
Various studies show that this pathological condition is not more common in athletes than in the normal population. Put the other way around, it is just as common in athletes as in inactive people, with the deleterious effects on performance. In a collective of 813 athletes, anemic values were found in 13% of subjects based on blood tests performed at SPU. In the same collective, serum ferritin levels <50 mcg/L were obtained in 37% of cases and <30 mcg/L in 15%. Thus, iron deficiency anemia represents the most common form of anemia in athletes.
Iron Deficiency Anemia
The cause of this deficiency is to be found in sport-specific losses as well as insufficient intake. In athletes, increased iron losses may occur via the gastrointestinal tract, skin (sweat), urine and, in female athletes, menstruation. For example, it has been described that intense running training can lead to intestinal microbleeds, which are exacerbated by frequent use of nonsteroidal anti-inflammatory drugs. The explanation is to be found in a combination of mechanical irritation due to concussion and load-induced reduced blood flow to the gastrointestinal tract. In addition, stress-related conditions may promote hemorrhagic gastritis.
Furthermore, microhematuria has been described in long-distance runners, also a consequence of mechanical irritation of the bladder. For a long time, damage to the erythrocytes in the sole of the runners’ feet was also suspected – this hypothesis is no longer pursued today. It is possible that erythrocyte damage caused by oxygen radicals, which are formed more frequently under stress, plays a role. In addition, up to 1 g of iron is lost through sweat.
On the side of insufficient intake, it is necessary to mention special dietary habits, such as vegetarian diet. They are not so rare in the athletic milieu and must definitely be clarified, because it is actually relatively easy to cover the daily iron losses in sports of about 1.8 mg in men and 2.3 mg in women. With a “normal” food intake of 2500 kcal, there are about 10-15 mg of iron is available, which is sufficient for a normal absorption rate of 10% (which can be increased up to 30% in the case of iron deficiency) – all the more so because the calorie requirement per training hour increases by approx. 600 kcal, and thus more iron is taken in via this additional food.
Importance of iron in the body
At this point, we would like to briefly point out the central importance of iron for life. Iron is found in the body in over 150 vital biochemical reactions, including those for energy production, DNA synthesis, cell proliferation, and mitochondrial activity. The role of iron in the production of neurotransmitters and in several neurological processes is particularly important. The 2.5 g of iron in women and 4 g in men are carefully “managed” – for different areas such as oxygen transport (75%) or enzymatic function (5%). The rest remains inactive, as reserve (ferritin and hemosiderin) and in the cells of the reticuloendothelial system (RES).
The human body has various mechanisms to use this important element sparingly (e.g. recycling of iron after decay of old red blood cells and iron retention). Since excessive iron levels would be toxic, absorption from the digestive tract is finely controlled and limited to 1-2 mg daily. In this context, hepcidin, produced in liver cells, plays an important regulatory role as an inhibitor of duodenal iron absorption and release of iron-storing cells. Recent findings show that, analogous to inflammation and iron administration, intense physical stress can provoke an outbreak of hepcidin with corresponding iron uptake blockage.
“Non-anemic iron deficiency”
This summarized information is intended to show that disorders of iron balance can occur in various forms and iron deficiency anemia is not the only expression of these disorders. It is quite conceivable that iron reserves are used up first, before hemoglobin drops below normal. The ferritin value is below 30 mcg/L, but the hemoglobin value is still normal. The term “iron deficiency without anemia” or “non-anemic iron deficiency” (NAID) is used in this not uncommon situation. Interestingly, this particular situation was underestimated for many years in medicine, especially in hematology, leading to exuberant reactions, and then to restrictive attitudes of health insurers towards intravenous iron applications. In NAID, the cardinal symptom is fatigue, a symptom also found in other disorders and also in athletes. A careful clinical workup and ferritin determination are indicated to initiate targeted therapy.
Figure 2 summarizes the diagnoses and treatment indications for adults again.
HAUSARZT PRAXIS 2018; 13(4): 3-5