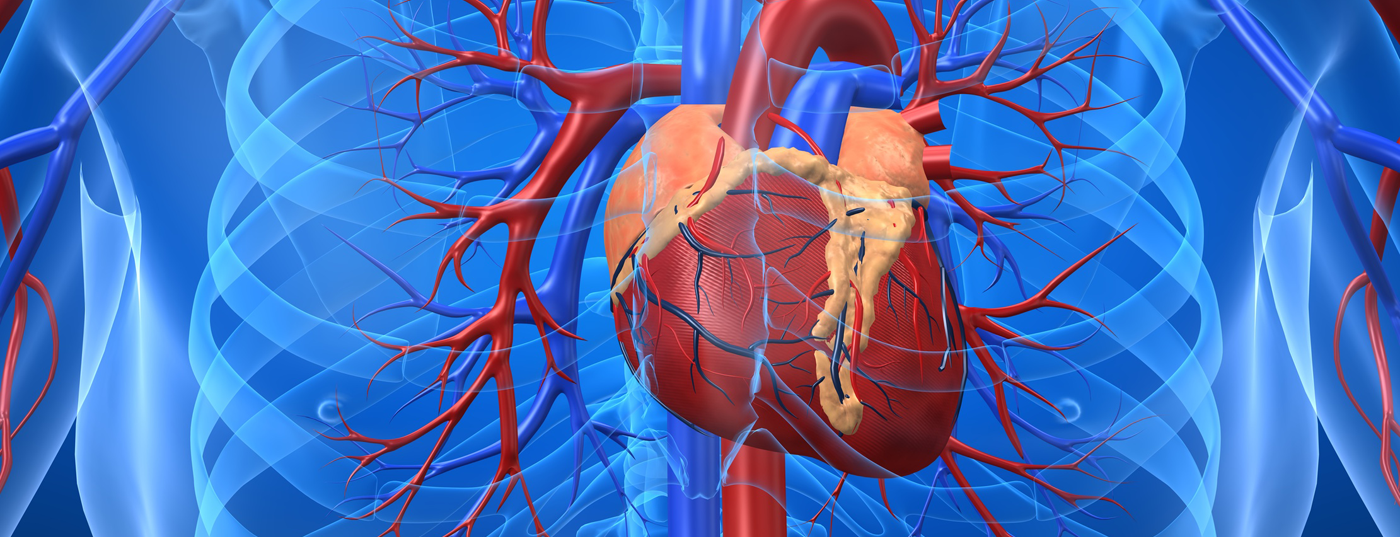
Various heart specialists from the University Hospital Zurich discussed the diagnosis and treatment of aortic valve stenosis at the Zurich Heart House, Foundation for Cardiovascular Research. The disease, treated purely with medication, leads to death within a few years. Since 2007, TAVI (transcatheter aortic valve implantation) has been used in addition to surgical heart valve replacement, with very good results. In a high-risk patient population, it results in faster recovery time and regain of mobility.
Aortic valve stenosis is a serious heart valve disease defined as narrowing or calcification of the aortic valve. In half of the cases, the disease leads to death within one year if treated with medication alone. In this context, the general practitioner should be aware of the following symptoms, which occur more frequently with increasing constriction: Possible signs include shortness of breath, chest pain, loss of performance and dizziness. “The risk of aortic valve stenosis increases with age. Approximately 3% of the population is affected. Many of the patients are around 80 years of age and older. This form of the disease is called degenerative,” says Prof. Thomas Lüscher, M.D., Director of the Department of Cardiology at the University Hospital Zurich.
The TAVI – Less invasive, faster recovery time
To improve symptoms and quality of life, the aortic valve must be replaced. For decades, the gold standard has been surgical valve replacement. However, since 2007, an innovative and now proven therapy has also been available: TAVI (transcatheter aortic valve implantation). This is a minimally invasive method that allows the aortic valve to be replaced without opening the chest or using a heart-lung machine. In this procedure, the new biological heart valve is implanted via a catheter, either through the inguinal artery or a small incision on the left chest wall. 462 TAVI procedures have already been performed at the University Hospital Zurich since the introduction of the technique. The results are very good. The narrowed valve is not surgically removed (as in traditional surgical aortic valve replacement). The new valve is left in the heart via a special technique and “pushed” to the side against the wall. According to PD Fabian Nietlispach, MD, team leader of TAVI in the Department of Cardiology at the University Hospital Zurich, the most commonly used valves are the balloon-expandable SAPIEN valves from Edwards. The latest generation is the Edwards SAPIEN 3 aortic valve (Fig. 1) . It has also been available on the Swiss market since January of this year. It can be implanted via different access routes: transfemoral (via inguinal artery) and transapical (via left chest wall). Due to a so-called “skirt” (outer sealing seam), it has the advantage of reducing paravalvular leakage (leaks) [1,2].

Effectiveness of TAVI confirmed by studies
The world’s first randomized pivotal trial of transcatheter aortic valve replacement in elderly, inoperable, and high-risk patients with severe aortic stenosis is the PARTNER trial. Results from Cohort B show a significant reduction in mortality for TAVI patients compared with conservative medical therapy [3]. In addition, TAVI was associated with significant health-related improvement in quality of life as assessed by the Kansas City Cardiomyopathy Questionnaire (KCCQ) and SF-12 questionnaire, which was maintained over one year [4]. TAVI is also noninferior to surgical aortic valve replacement in high-risk patients (cohort A) [5]. “TAVI valve replacement could be used in the future in younger patients with intermediate risk. Studies are currently underway that are researching in this direction. So it remains exciting,” Dr. Nietlispach concluded.
Improving the quality of life
Because of its relatively low invasiveness, TAVI offers significant advantages compared to surgery: faster recovery times for the patient and a resulting regained mobility. All potential risks associated with the use of a heart-lung machine can be eliminated. In addition, side effects are reduced because the prostheses are biological heart valves and therefore no anticoagulant medication with oral vitamin K antagonists is necessary. The risk of surgical trauma from the use of the heart-lung machine, transection of the sternum, and cardiac arrest is reduced, significantly lowering the burden on the patient. The design of the SAPIEN 3 aortic valve is unique in this form and is intended to further simplify the procedure, keep postoperative complications even lower, and thus accelerate patient recovery.
“TAVI is primarily used to treat elderly patients with comorbidities such as kidney weakness, diabetes or arterial occlusive disease. Another advantage of this method is that general anesthesia is not required in most cases. This is because the recovery phase is also shortened and the patient’s quality of life is improved in a shorter time. Overall, the patient spends less time in the hospital and returns to everyday life sooner. Both result in a faster improvement in quality of life,” explained Dr. Nietlispach.
Family doctor assumes decisive role
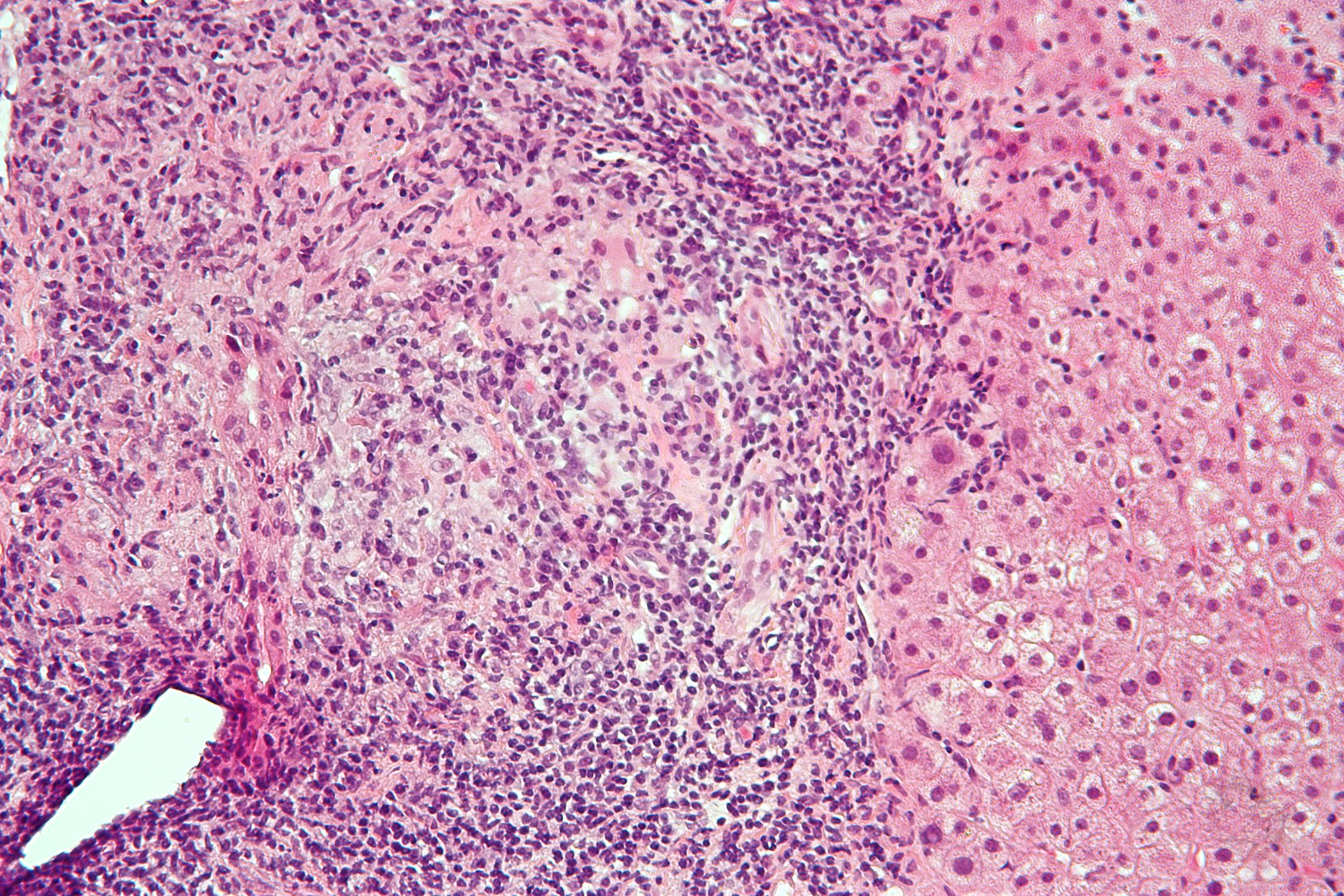
Diagnosis begins in the primary care physician’s office. Complaints and findings such as exertional dyspnea, angina, systolic or syncope must be interpreted correctly. Because of its frequency in patients between 75 and 90 years of age, it is important to keep aortic valve stenosis in mind as a diagnosis, especially in this patient population. Exhaustion, weakness and dyspnea are often blamed on old age. However, if heart murmurs are present, patients should always be referred to a cardiologist for echocardiography or to the hospital for further evaluation. There, the further procedure is determined on the basis of the echocardiographically determined severity of the aortic valve stenosis. In severe symptomatic aortic valve stenosis, valve replacement is the only effective therapy. The decision for one of the possible treatment methods is made depending on the findings, but also the comorbidities and the presence of frailty. In this context and with regard to individual preferences, the information from the referring GP or cardiologist is important, as they have known the patient for some time [6].
Thus, the primary care physician has an important role in the overall diagnostic approach in several respects. He should be well informed about the procedure in order to be able to provide information to patients and relatives in case of queries [6].
Source: Lecture at Zurich Heart House, February 5, 2014, Zurich.
Literature:
- Binder RK, et al: Transcatheter Aortic Valve Replacement With the SAPIEN 3: A New Balloon-Expandable Transcatheter Heart Valve. J Am Coll Cardiol Intv 2013; 6(3): 293-300. doi:10.1016/j.jcin.2012.09.019.
- Dvir D, et al: TCT-787 Preliminary Clinical Experience using the SAPIEN 3 device. J Am Coll Cardiol 2013; 62(18_S1): B239. doi:10.1016/j.jacc.2013.08.1539.
- Leon MB, et al; PARTNER Trial Investigators: Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 2010; 363: 1597-1607.
- Reynolds MR, et al; Placement of Aortic Transcatheter Valves (PARTNER) Investigators: Health-related quality of life after transcatheter aortic valve replacement in inoperable patients with severe aortic stenosis. Circulation 2011; 124: 1964-1972.
- Smith CR, et al; PARTNER Trial Invetsigators: transcatheter versus surgical aortic-valve replacement in high-risk patients. N ENgl J Med 2011; 364: 2187-2198.
- Mücke C: Severe aortic stenosis – from suspicion to therapeutic decision. Ars Medici 2013; 21: 1064-1065.
HAUSARZT PRAXIS 2014; 9(5): 11-12