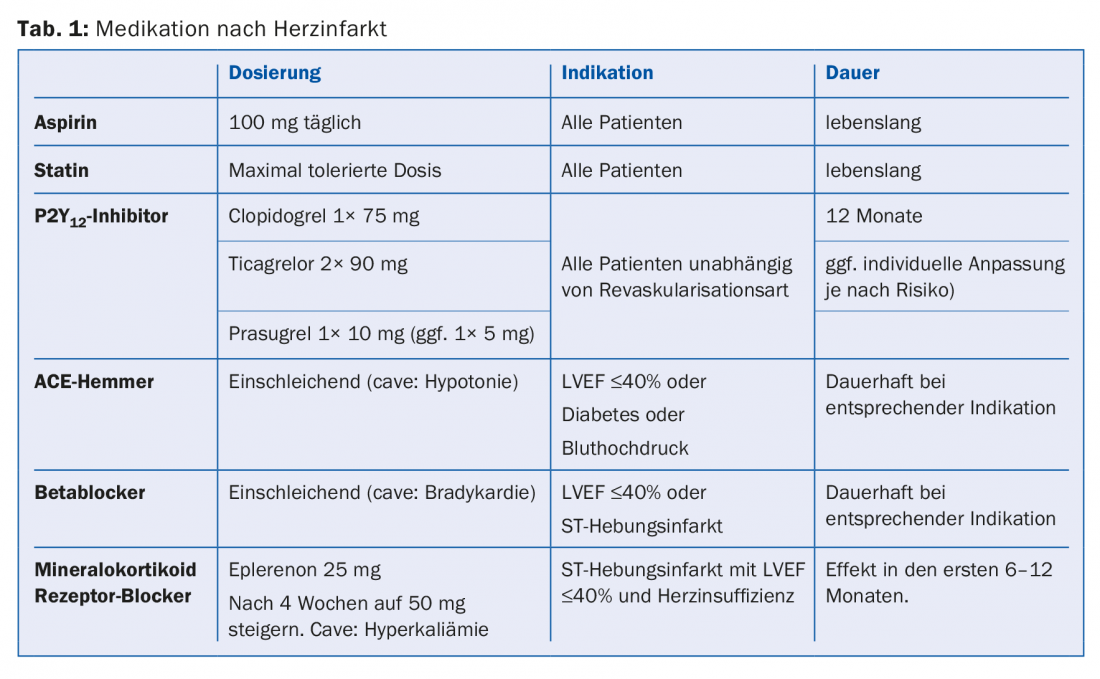
Heart attack patients should receive aspirin 100 mg and the maximum tolerated statin dose for life. Regardless of the type of revascularization, all myocardial infarction patients should take a P2Y12 inhibitor for 12 months (clopidogrel, ticagrelor, or prasugrel). Depending on the risk of bleeding and ischemia, the duration can be adjusted individually. Myocardial infarction patients with impaired systolic left ventricular function (ejection fraction ≤40%), hypertension, or diabetes benefit from ACE inhibitors. Beta-blockers should be used in patients after ST-segment elevation myocardial infarction and in all patients with impaired systolic left ventricular function (ejection fraction ≤40%).
Therapy after a heart attack is based on two pillars: lifestyle modification and medication. Along with a balanced diet and regular physical activity, abstinence from smoking is one of the most important lifestyle factors that can improve prognosis after a heart attack. Basic medication with aspirin and a statin, which is recommended for all patients with manifest atherosclerosis for life, initially includes dual antiplatelet therapy and, depending on the size of the infarct, systolic left ventricular function, and risk factors, the use of a beta-blocker, an angiotensin-converting enzyme (ACE) inhibitor, or even a mineralocorticoid receptor antagonist (Table 1) [1]. The type of revascularization has no relevant influence on drug therapy after myocardial infarction [2]. The treatment recommendations for myocardial infarction patients after aortocoronary bypass surgery (ACBP), percutaneous coronary revascularization (PCI), or conservative management, do not differ fundamentally.
Aspirin
Aspirin leads to reduction of platelet activity through irreversible inhibition of cyclooxgenase-1. This effect is achieved at dosages between 75 mg and 150 mg. Higher dose increases gastrointestinal side effects with no other beneficial effects on platelet inhibition. Therefore, lifelong therapy with aspirin 100 mg daily is generally recommended for all patients after myocardial infarction. This therapy should never be paused prior to elective surgery (exceptions: neurosurgical procedures involving opening of the dura mater and posterior orbital surgery). For patients who take oral anticoagulation (OAC) for life (e.g., because of a mechanical heart valve or atrial fibrillation with increased risk of stroke), OAC is sufficient in the long term as secondary prevention after myocardial infarction. Long-term combination of aspirin with an OAK is not beneficial but increases the risk of bleeding.
Adenosine diphosphate receptor (P2Y12) antagonists
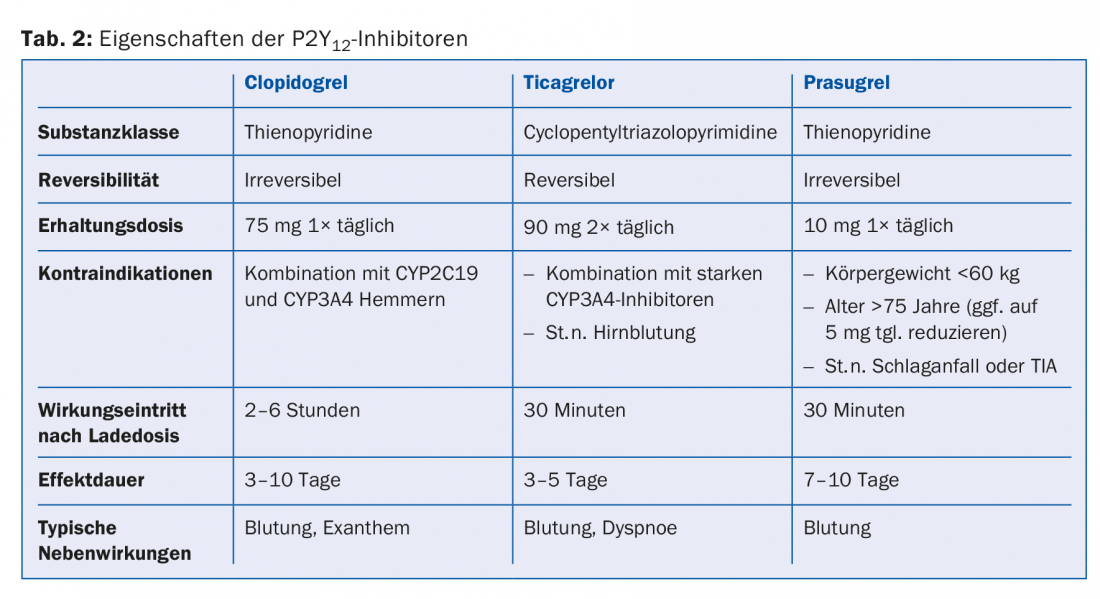
The CURE trial [2] demonstrated that after myocardial infarction and independent of revascularization, additional platelet inhibition with a P2Y12 antagonist reduced ischemic end points. Currently, three oral P2Y12 antagonists are approved for this use: Clopidogrel [2], Prasugrel [3] and Ticagrelor [4] (Table 2). While the first two drugs are prodrugs that must first be metabolized and eventually lead to irreversible blockade of the P2Y12 receptor, ticagrelor is directly active and reversible. In general, after myocardial infarction, a P2Y12 antagonist is recommended in addition to aspirin (dual antiplatelet therapy, DAPT) for 12 months [1,5,6]. This applies to patients treated conservatively as well as after PCI or ACBP. Especially in the first months after stent implantation, uninterrupted DAPT therapy is essential, because without DAPT the risk of stent thrombosis would be massively increased.
In patients at high risk of bleeding or ischemia [7] or with an indication for OAK, the DAPT duration or the duration of the combination of DAPT with OAK must be decided on an individual basis. In principle, concomitant use of DAPT and OAK should be prescribed for as short a time as possible (one to a maximum of six months) because the risk of bleeding is increased sixfold with this combination. On the other hand, there are situations in which, due to an increased risk of ischemia, DAPT therapy is beneficial even over several years. Individual therapy recommendations should be evident in the discharge report after myocardial infarction or, in case of doubt, discussed with the treating cardiologist.
Lipid-lowering therapy
Patients after myocardial infarction are recommended lifelong therapy with a highly potent statin that lowers low-density lipoprotein cholesterol (LDL-C) by at least half or to below 1.8 mmol/l (e.g., atorvastatin 80 mg or rosuvastatin 20 mg). Statins act directly on the vascular walls, leading to plaque stabilization and, in high doses, even plaque regression. Regular measurement of LDL-C serves as compliance control and therapy adjustment. If the LDL-C level is above 1.8 mmol/l under maximum tolerated statin dose, an additional lipid-lowering agent should be prescribed (e.g., ezetimibe 10 mg) [8]. A new class of substances are the monoclonal antibodies against proprotein convertase subtilisin-kexin type 9 (PCSK9), which are applied subcutaneously and lower LDL-C much more strongly than statins. So far, these have been approved for use in familial hypercholesterolemia, but it is expected that in the future these drugs will also be used after a heart attack.
ACE inhibitors
After myocardial infarction, ACE inhibitors improve left ventricular (LV) remodeling. They are the basic therapy for systolic heart failure and arterial hypertension. By vasodilation, blood pressure reduction and preload reduction, ACE inhibitors relieve the left ventricle and influence the remodeling processes in the myocardium after myocardial infarction. Accordingly, patients after a major infarction, patients with impaired LV systolic function (≤40%), arterial hypertension, or diabetes mellitus benefit particularly. After about half a year, the adaptation processes in the myocardium after a heart attack are complete. Accordingly, nondiabetics without arterial hypertension and with normal LV systolic function benefit little from ACE inhibitors. If ACE inhibitor intolerance (irritable cough), can be switched to an angiotensin receptor blocker.
Beta blocker
Beta-blockers lower blood pressure and pulse rate by blocking the action of adrenaline and noradrenaline. The oxygen demand of the myocardium is reduced, thus relieving the heart. Thus, beta-blockers are a basic therapy for systolic heart failure. Beta-blockers should be used after ST-elevation myocardial infarction and in all myocardial infarction patients with impaired LV systolic function (≤40%). To avoid symptomatic bradycardia, beta-blockers should be gradually increased after myocardial infarction.
Mineralocorticoid receptor antagonists
This class of agents, which has an important role in symptomatic heart failure with severely impaired LV systolic function, can favorably influence LV remodeling after a major myocardial infarction [9]. Accordingly, it is used in patients after ST-segment elevation myocardial infarction with an LV EF ≤40% and heart failure. Because this class of drugs can lead to hyperkalemia, it should be used only with adequate renal function (creatinine <221 μmol/L in men and <177 μmol/L in women) and with regular monitoring of serum potassium.
Calcium antagonists
Calcium antagonists can be used for symptomatic therapy of angina pectoris, but they have no particular value in patients after myocardial infarction. If a calcium antagonist is used after a myocardial infarction, the patient should have previously taken the maximum tolerated dose of an ACE inhibitor and a beta blocker. If blood pressure is not adequately controlled with this combination, a calcium antagonist may be used, with long-acting ones being preferred (e.g., amlodipine, lercanidipine).
Summary
Whereas aspirin and statin should be taken for life after myocardial infarction, all other drugs are sometimes useful only temporarily (e.g., P2Y12 antagonists), and sometimes their benefit has been demonstrated only in certain groups of patients (e.g., ST-segment elevation myocardial infarction, impaired LV systolic function, heart failure, or arterial hypertension). Important tasks of the primary care provider include monitoring compliance [10], increasing the dose of initially low-dose medications (especially ACE inhibitors and beta blockers), and managing potential side effects. Patients should be encouraged to take these usually well-tolerated combination therapies regularly, but not without pointing out that optimal therapy consists of a combination of medications and lifestyle modifications.
Conflicts of interest: The author has received speaking fees from AstraZeneca and serves on an advisory board for Abbott.
Literature:
- Windecker S, et al: 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014; 35(37): 2541-2619.
- Yusuf S, et al: Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial I. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001; 345(7): 494-502.
- Wiviott SD, et al: Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007; 357(20): 2001-2015.
- Wallentin L, et al: Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2009; 361(11): 1045-1057.
- Steg PG, et al: ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012; 33(20): 2569-2619.
- Roffi M, et al: 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016; 37(3): 267-315.
- Binder RK, Luscher TF: Duration of dual antiplatelet therapy after coronary artery stenting: where is the sweet spot between ischaemia and bleeding? Eur Heart J 2015; 36(20): 1207-1211.
- Cannon CP, et al: Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N Engl J Med 2015; 372(25): 2387-2397.
- Pitt B, et al: Eplerenone Post-Acute Myocardial Infarction Heart Failure E, Survival Study I. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003; 348(14): 1309-1321.
- Choudhry NK, et al: Post-Myocardial Infarction Free Rx E, Economic Evaluation T. Full coverage for preventive medications after myocardial infarction. N Engl J Med 2011; 365(22): 2088-2097.
HAUSARZT PRAXIS 2016; 11(12): 29-34











