A 43-year-old patient discontinues the PPI as discussed with the physician after 14 days of therapy. The complaints return so violently that he continues the therapy on his own authority. What to do?
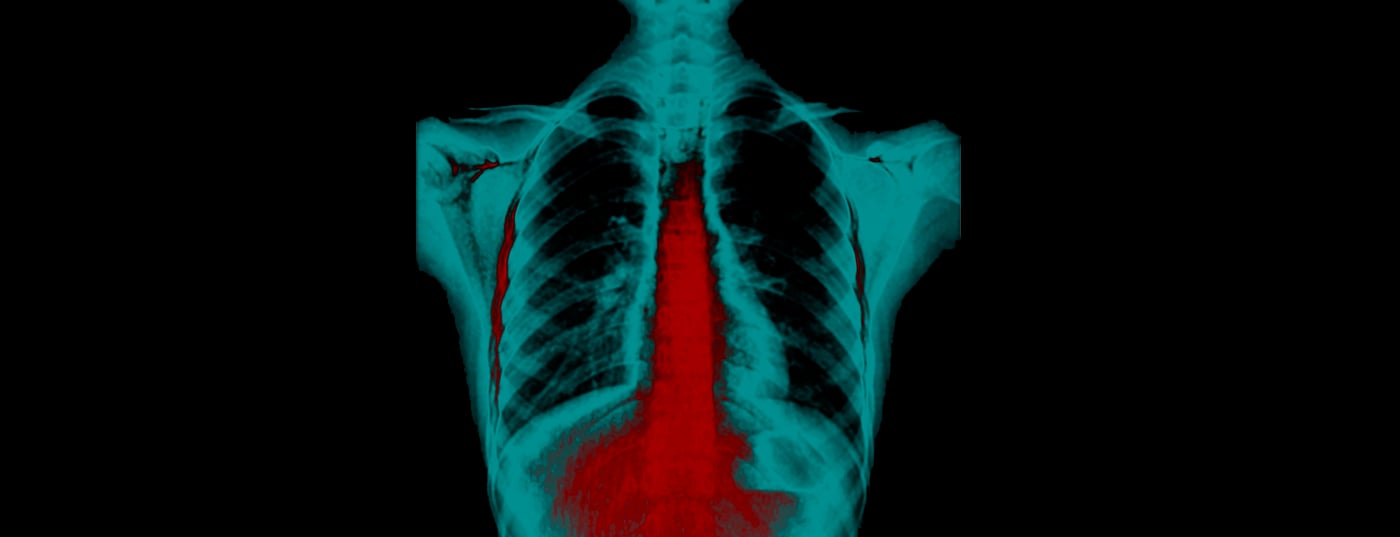
Background: The 43-year-old patient was affected by marked retrosternal pain, heartburn, and regurgitation shortly before the Christmas holidays. Gastroscopy revealed first-degree esophagitis, so medication was initiated with a PPI at a dosage of 40mg once daily. It was agreed that this therapy would be administered over 14 days while adhering to GERD-specific dietary recommendations and lifestyle changes. Raising the head of the bed was also discussed with the patient. 6 weeks after initiation of PPI medication, the patient came to the consultation and reported that he had experienced excellent symptom improvement after 2 weeks of therapy with the PPI, and had stopped taking the PPI as discussed. Already on the following day, the complaints, especially the heartburn, reappeared to such an extent that he had to resume therapy with the PPI. After another 14 days, another attempt to stop the drug followed. This was also immediately accompanied by heartburn, so the patient continued the therapy and now asks for advice in the consultation.
Therapy and course: The renewed anamnesis shows that there is no GERD risk nutrition and with normal body weight no recommendation for weight reduction has to be given. Rather, in this patient, it is clinically difficult to assess whether the recurrent complaints are rebound complaints induced by PPI discontinuation or are actually now chronic GERD complaints. The clinical assessment suggests that chronic GERD symptoms are unlikely, especially since the patient had never suffered from heartburn, regurgitation, or other GERD symptoms throughout his life. In this situation, one can therefore assume classic rebound complaints. Accordingly, the patient is informed that in some patients the discontinuation of PPI may be accompanied by such rebound symptoms and how to deal with them. The following procedure was defined with the patient: Initiation of alginate therapy, three times daily, 30 minutes after eating and from the second day reduction of PPI dosage to one tablet, every other day for one week, followed by cessation of PPI therapy with continuation of alginate therapy for another ten days. 4 months later, the patient visits the practice for a different reason, a flu-like infection, and when asked, reports that the discussed elimination regimen worked well and that he has not experienced any reflux symptoms since.
 Comment by Prof. Martin Storr, MD: Medication with PPI-type acid blockers is often started in primary care practice to relieve upper gastrointestinal tract symptoms. Often this is a pragmatic, symptomatic attempt at therapy; in other cases, medication is justified by findings in imaging procedures such as gastroscopy. In most patients, continuous PPI therapy is not necessary, so that rapid discontinuation is desired and also appears medically given. In many cases, short-term PPI medication in particular can be discontinued without difficulty, but some patients report a recurrence of symptoms shortly after discontinuation. Here, good advice is expensive, because the differentiation between a possibly necessary permanent PPI medication or a rebound phenomenon is often clinically difficult. Rebound phenomenon is reflux symptoms that may occur in patients after PPI treatment for more than 7 days. This rebound phenomenon is observed not only in patients but also in healthy subjects receiving PPI medication in the context of scientific studies. The question of which procedure is now adequate in the event of a rebound has not been adequately investigated in clinical studies. An elegant therapeutic approach is a phase-out regimen in which an overlapping drug is used that does not lead to a rebound phenomenon. Here, alginates are clinically successful with their dual mechanism of action, which has a reflux-preventing mechanism at the acid pocket on the cardia on the one hand and a mucosa-protective effect in the esophageal region on the other. The dosage and type of tapering regimen recommended to patients is up to each prescriber, as there are no clinical studies on this. The tapering regimen described in the present case envisages slow tapering, with overlapping tapering medication not continuing for too long.
Comment by Prof. Martin Storr, MD: Medication with PPI-type acid blockers is often started in primary care practice to relieve upper gastrointestinal tract symptoms. Often this is a pragmatic, symptomatic attempt at therapy; in other cases, medication is justified by findings in imaging procedures such as gastroscopy. In most patients, continuous PPI therapy is not necessary, so that rapid discontinuation is desired and also appears medically given. In many cases, short-term PPI medication in particular can be discontinued without difficulty, but some patients report a recurrence of symptoms shortly after discontinuation. Here, good advice is expensive, because the differentiation between a possibly necessary permanent PPI medication or a rebound phenomenon is often clinically difficult. Rebound phenomenon is reflux symptoms that may occur in patients after PPI treatment for more than 7 days. This rebound phenomenon is observed not only in patients but also in healthy subjects receiving PPI medication in the context of scientific studies. The question of which procedure is now adequate in the event of a rebound has not been adequately investigated in clinical studies. An elegant therapeutic approach is a phase-out regimen in which an overlapping drug is used that does not lead to a rebound phenomenon. Here, alginates are clinically successful with their dual mechanism of action, which has a reflux-preventing mechanism at the acid pocket on the cardia on the one hand and a mucosa-protective effect in the esophageal region on the other. The dosage and type of tapering regimen recommended to patients is up to each prescriber, as there are no clinical studies on this. The tapering regimen described in the present case envisages slow tapering, with overlapping tapering medication not continuing for too long.
Further reading:
- Wilkinson J, Wade A, Thomas SJ, et al: Randomized clinical trial: a double-blind, placebo-controlled study to assess the clinical efficacy and safety of alginate-antacid (Gaviscon Double Action) chewable tablets in patients with gastro-oesophageal reflux disease. Eur J Gastroenterol Hepatol. 2019 Jan;31(1): 86-93.
- Sauter M, Fox MR: The acid pocket – a novel target for the treatment of gastro-esophageal reflux disease. Z Gastroenterol. 2018 Oct;56(10): 1276-1282.
- Coyle C, Crawford G, Wilkinson J, et al: Randomised clinical trial: addition of alginate-antacid (Gaviscon Double Action) to proton pump inhibitor therapy in patients with breakthrough symptoms. Aliment Pharmacol Ther. 2017 Jun;45(12):1524-1533.
- Rohof WO, Bennink RJ, Smout AJ, et al: An alginate-antacid formulation localizes to the acid pocket to reduce acid reflux in patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2013 Dec;11(12): 1585-1591.