Often, even “out of treatment” emphysema patients can be offered improvement in dyspnea and exercise capacity through a lung volume reducing procedure. The postinterventional beneficial effects after surgical or bronchoscopic lung volume reduction clearly outweigh the comparatively low periinterventional morbidity and mortality. Bronchoscopic lung volume reduction can often offer a good alternative to “inoperable” patients. The selection of the appropriate procedure should be made within an interdisciplinary consortium consisting of pulmonologists, thoracic surgeons and radiologists, taking into account pulmonary functional, radiological, clinical as well as subjective factors.
Chronic obstructive pulmonary disease (COPD) leads to irreversible narrowing of the airways (obstruction) and/or destruction of the lung parenchyma (emphysema). These two mechanisms result in pulmonary hyperinflation, which causes the diaphragm to deepen and flatten. However, a flattened diaphragm is no longer able to perform its role as the most important respiratory muscle. This, the loss of gas exchange surface, and the reduction in elastic recoil ultimately contribute to increased work of breathing, which affected patients experience as permanent shortness of breath. Initially, dyspnea is reported only on exertion, then as the disease progresses, it is reported as speech and resting dyspnea.
The cornerstones of conservative treatment primarily include consistent smoking cessation. In addition, patients benefit from regular physical activity (outpatient/inpatient pulmonary rehabilitation if necessary) and avoidance of infectious complications through influenza and pneumococcal vaccination. Drug therapy consists primarily of inhaled therapy with one to two long-acting bronchodilators (betamimetics, anticholinergics). Inhaled steroids, macrolide antibiotics, and/or roflumilast may also be indicated to prevent COPD exacerbations. Finally, if there is significant resting hypoxemia, continuous oxygen therapy is used. If these conservative treatment options have been largely exhausted, interventional treatment may be indicated.
Principle of interventional emphysema therapy
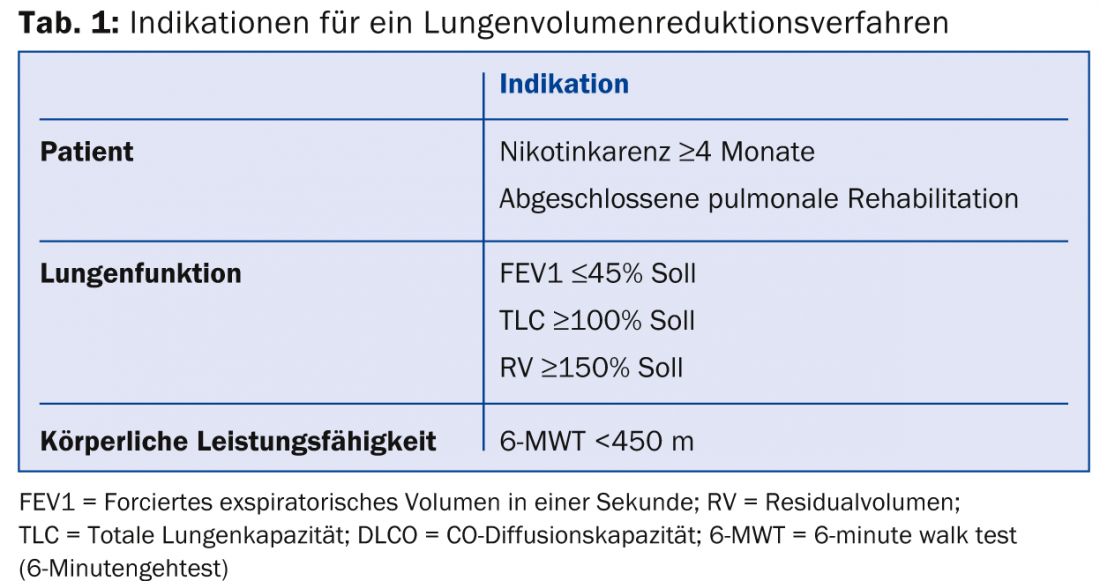
The goal of interventional emphysema therapy is essentially to decrease lung hyperinflation so that the flattened diaphragm can regain its characteristic shape (hump). In fact, the diaphragmatic humps enable a functional respiratory muscle pump in the first place, which leads to a decrease in dyspnea and improvement of lung function. Both surgical (LVRS) and bronchoscopic lung volume reduction (valves, coils, steam application) can achieve this goal, provided some prerequisites are met (tab. 1) . In particular, patients who are severely limited by dyspnea benefit from interventional emphysema therapy. However, prior smoking cessation and completed pulmonary rehabilitation are essential.
Surgical Lung Volume Reduction (LVRS).
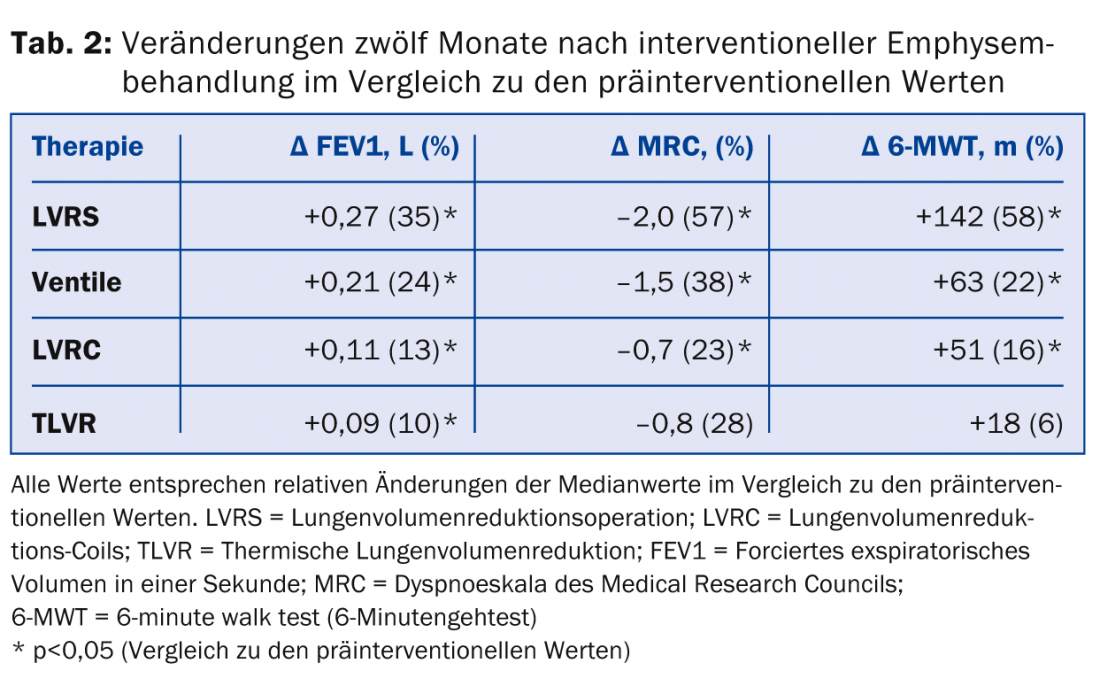
In LVRS, functional lung parenchyma is preserved and only severely damaged emphysematous lung portions are resected under general anesthesia, usually thoracoscopically. To define the so-called target zones of resection, lung perfusion scintigraphy and high-resolution computed tomography are indicated for surgical planning. LVRS can achieve a reduction in mortality in addition to an improvement in quality of life, physical performance, and pulmonary function if patient selection is adequate (Table 2).
In addition, the risk of future COPD exacerbations seems to tend to decrease postoperatively. In most cases, these positive effects last for at least five years postoperatively. However, after pulmonary function values and symptoms have returned to preoperative levels, repeat LVRS can be evaluated, as this may return improvement sustained over at least one year. A round focus suspected of carcinoma within an emphysematous target zone can also be removed with curative intent during LVRS without accepting a deterioration of lung function.
Preoperatively, coronary artery disease and pulmonary arterial hypertension should be ruled out, as these are considered contraindications for LVRS. Pulmonary complications after LVRS occur with a frequency of approximately 30% within 30 days. The most common complications are prolonged air fistula, respiratory failure, and pneumonia. The published 90-day mortality after LVRS is 5%, but this number is much lower according to our own experience and is about 1%. The hospitalization period is approximately twelve days.
Bronchoscopic lung volume reduction
In bronchoscopic procedures for lung volume reduction, there are three methods to choose from: endo- resp. intrabronchial valves (EBV/IBV), lung volume reduction coil (LVRC), or thermal obliteration of the (emphysematous) lung tissue. All methods can be applied via a flexible bronchoscope, which usually requires general anesthesia. Superficial sedation in spontaneous breathing is also possible.
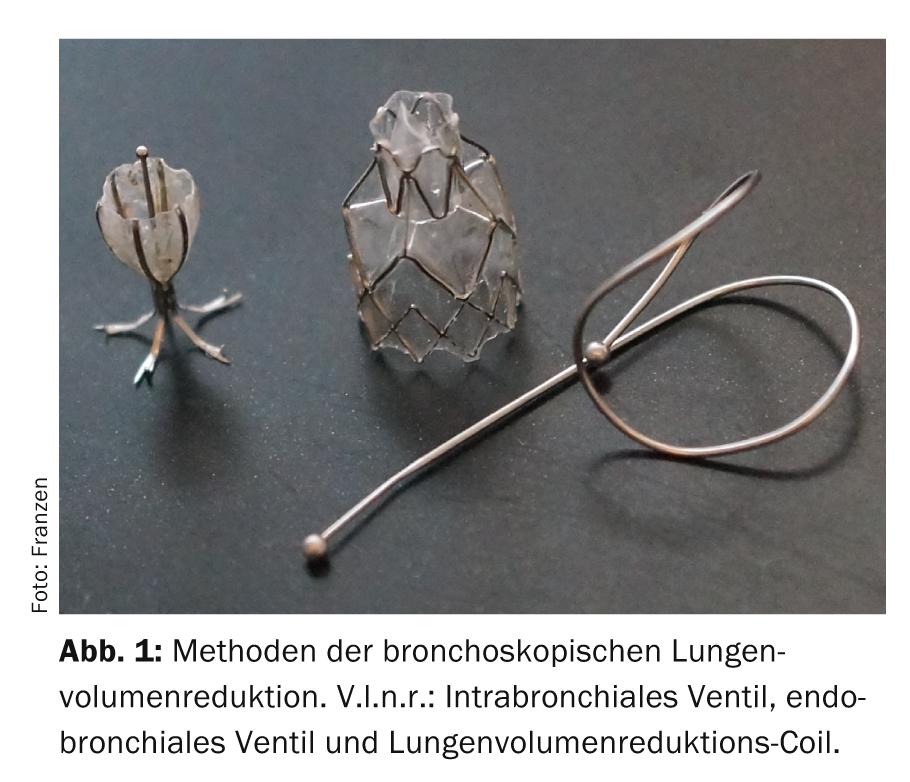
Endo- or intrabronchial valves: Valves are one-way valves that allow airflow from emphysematous lung areas during exhalation but prevent the same during inspiration (Fig. 1) .
In this way, atelectasis of the treated section of the lung occurs, leading to a decrease in pulmonary hyperinflation. However, atelectasis and thus a perceptible therapeutic effect can only develop if there is no ventilation from an adjacent lung area via collateral channels, e.g. Kohn’s pores. Possible collateral ventilation can be measured with a catheter that can be inserted via a bronchoscope or estimated on computed tomography.
Improvements in symptoms and lung function after valve treatment can also last for several years (Tab.2). It should be noted here that endobronchial valve insertion is the only fully reversible procedure for interventional emphysema treatment because all or individual valves can be removed with flexible bronchoscopy under superficial sedation.
Preinterventional cardiological investigations are usually not necessary for valve inserts. In contrast, analogous to LVRS, lung perfusion scintigraphy and high-resolution computed tomography are essential.
The most common complications in the first 90 days after valve insertion are COPD exacerbations (10%) and pneumothoraces (approximately 20%). Interdisciplinary care in a center is strongly advisable, as occasionally the removal of one or more valves is necessary. Pneumothoraces after valve insertion occur because of traction forces on peripheral lung tissue due to rapid atelectasis formation, and indeed the therapeutic effect is particularly pronounced in these patients. The 90-day mortality rate is 1%. The average hospitalization time for valve insertion is five days.
Lung Volume Reduction Coils (LVRC): A completely different approach is taken with the insertion of LVRC wires made of the shape-memory alloy nitinol, which are inserted stretched into a subsegmental bronchus and assume their characteristic curved shape after removal of the insertion sleeve (Fig. 1). In the process, they pull the tissue together by pulling the conducting airways; the elastic restoring forces of the wire spirals are thereby transferred to the lung tissue. This leads on the one hand to a volume reduction effect and on the other hand to an improvement of the elastic recoil forces of the lungs (“elastic recoil”). To achieve a noticeable therapeutic effect, approximately ten LVRC must be placed per lobe of the lung. Currently, long-term efficacy data after more than one year are not yet available (tab. 2) . The advantage of LVRC is that they can be used in patients with collateral ventilation or missing target zones as well as in completely homogeneous emphysema. The procedure is irreversible. The most common complication in the first 30 days after LVRC therapy is hemoptysis in 30% of cases, which is why oral anticoagulation or dual platelet anticoagulation and relevant pulmonary arterial pressure elevation are considered absolute contraindications for this procedure. Deaths have not been reported to date in the few available studies of LVRC.
Thermal lung volume reduction (TLVR): Bronchoscopic application of thermal energy in the form of water vapor leads to fibrosis and atelectasis via an inflammatory response. The most common complication after steam application is COPD exacerbation (20%) or generalized inflammatory syndrome (SIRS). The success of the treatment does not depend on the degree of heterogeneity of the emphysema or the fissure integrity (tab. 2). However, this procedure is also irreversible.
Selection of the appropriate therapy method
LVRS is most effective in terms of improving pulmonary function and symptomatology. In addition, the best long-term results are currently available for LVRS, as well as data on improved survival. Nevertheless, bronchoscopic lung volume reduction procedures have an important role in modern emphysema treatment. First, periinterventional morbidity and mortality appear to be lower compared with LVRS, so multimorbid patients and those marginal in terms of pulmonary function benefit from these procedures. Patients with severely impaired one-second or diffusion capacity can no longer be operated on, but a bronchoscopic procedure can often still be considered. Hospital stay is usually shorter in patients treated by endoscopy. The effect of the various bronchoscopic procedures was recently confirmed in a meta-analysis.
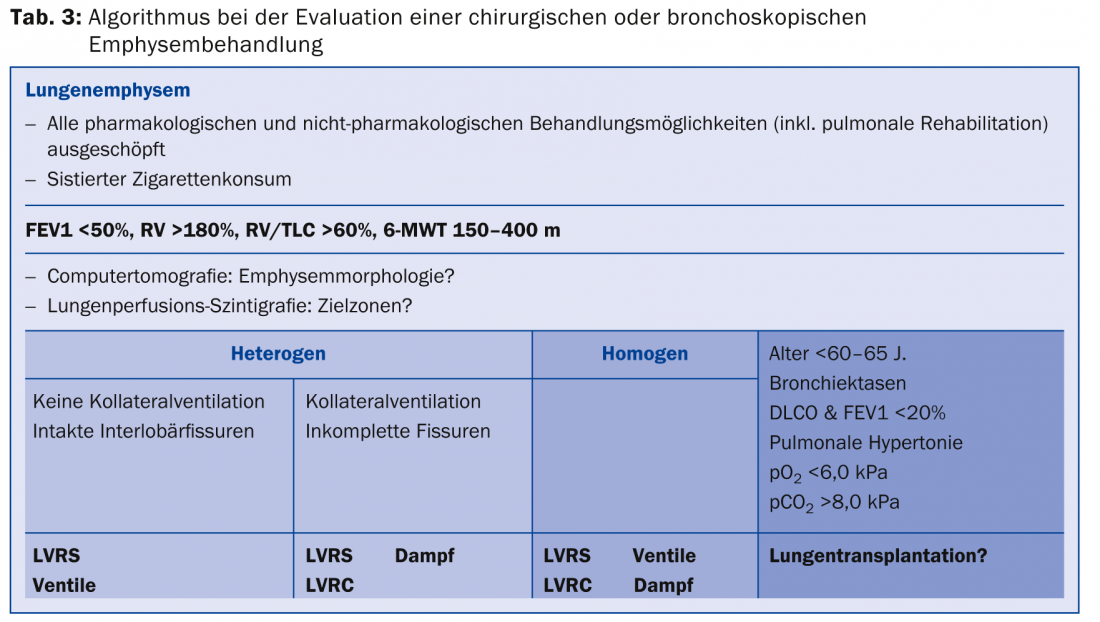
When selecting the appropriate therapeutic procedure for interventional emphysema therapy, it is crucial to consider emphysema morphology, possible collateral ventilation, and also the patient’s wishes, in addition to pulmonary functional and clinical aspects. The options become greater due to the multitude of procedures, but the decisions thus also become more difficult. For this reason, each patient evaluated for interventional emphysema treatment should be discussed by an interdisciplinary panel consisting of pulmonologists, thoracic surgeons, and radiologists to determine the most appropriate procedure for the individual. In this sense, surgical and bronchoscopic lung volume reduction procedures do not represent competing methods, but rather complementary ones that can also be combined to some extent. In this regard, the diagram presented in Table 3 may provide assistance in decision making regarding the appropriate procedure for emphysema treatment.
Further reading:
- Fishman A, et al: A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003; 348: 2059-2073.
- Weder W, et al: Persistent benefit from lung volume reduction surgery in patients with homogeneous emphysema. Ann Thorac Surg 2009; 87: 229-236.
- Shah PL, Herth FJ: Current status of bronchoscopic lung volume reduction with endobronchial valves. Thorax 2014; 69: 280-286.
- Tutic M, et al: Lung-volume reduction surgery as an alternative or bridging procedure to lung transplantation. Ann Thorac Surg 2006; 82: 208-213.
- Hamacher J, et al: Improved quality of life after lung volume reduction surgery. Eur Respir J 2002; 19: 54-60.
- Choong CK, et al: Concomitant lung cancer resection and lung volume reduction surgery. Thorac Surg Clin 2009; 19: 209-216.
- Venuta F, et al: Long-term follow-up after bronchoscopic lung volume reduction in patients with emphysema.
- Eur Respir J 2012; 39: 1084-1089.
- Deslee G, et al: Lung volume reduction coil treatment for patients with severe emphysema: a European multicentre trial. Thorax 2014 Nov; 69(11): 980-986.
- Herth FJ, et al: Characterization of outcomes 1 year after endoscopic thermal vapor ablation for patients with heterogeneous emphysema. Int J Chron Obstruct Pulmon Dis 2012; 7: 397-405.
- Iftikhar IH, McGuire FR, Musani AI: Efficacy of bronchoscopic lung volume reduction: a meta-analysis. Int J Chron Obstruct Pulmon Dis 2014; 9: 481-491.
- Rathinam S, et al: The role of the emphysema multidisciplinary team in a successful lung volume reduction surgery program. Eur J Cardiothorac Surg 2014 Dec; 46(6): 1021-1026; discussion 1026.
HAUSARZT PRAXIS 2015; 10(3): 20-24











