Most patients with CML are dependent on therapy with a tyrosine kinase inhibitor for the rest of their lives. However, there is increasing research into when and in which patients it would be possible to stop therapy. The latest results of the EURO-SKI study were presented at this year’s EHA Congress.
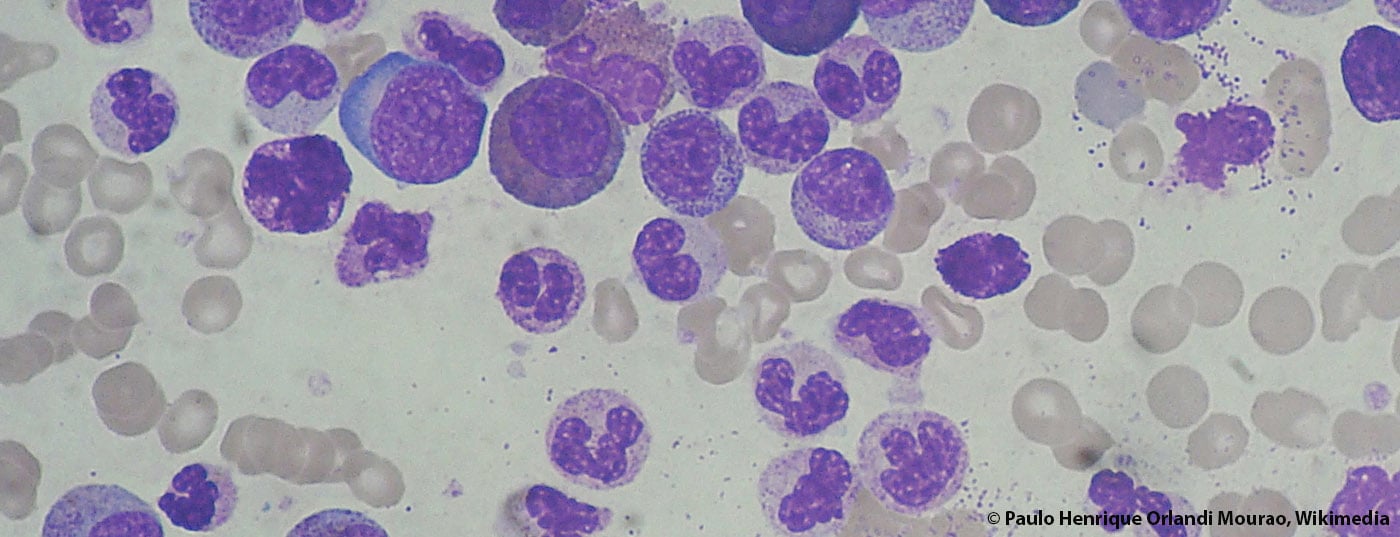
Tyrosine kinase inhibitors (TKIs) have fundamentally changed the treatment and care of patients with chronic myeloid leukemia (CML). Patients who respond to therapy now have almost the same life expectancy as people without CML. However, patients still need to take TKIs for the rest of their lives.
Several trials have attempted to stop treatment in patients with a “deep molecular response” (MR4), and approximately 50% of patients remained in remission without a TKI. Current trials are evaluating the criteria a patient must meet to discontinue TKI treatment without risking relapse.
Discontinuation attempt only after three years of TKI therapy
At the EHA Congress, the corresponding results of the EURO-SKI (Europe Stop Tyrosine Kinase Inhibitors) study were presented [1]. A total of 760 patients were enrolled in the study between May 2012 and December 2014 (46.6% of whom were women, mean age 60.3 years). 10% were high-risk patients according to EUTOS score, 18% were high-risk patients according to Sokal score. First-line therapy consisted of imatinib in 94% of patients, 2% received dasatinib, and 4% received nilotinib. 115 patients have since been treated with second-line therapy due to resistance to the first-line agent (58 dasatinib, 7 imatinib, 49 nilotinib). The median duration of treatment with a TKI was 91 months (range: 36.3-170 months). Requirements for inclusion in the study were that patients had received a TKI for at least three years and had achieved a deep molecular response for at least one year.
After two years, 50% of patients still in remission
In 717 patients, the corresponding molecular data were collected after discontinuation of the TKI. Molecular response (MMR) was lost in 331 subjects during follow-up (1-36 months) after TKI discontinuation, 4 died in remission during the follow-up phase, and 381 patients were still in remission at the last follow-up. 62% of patients were in remission 6 months after stopping therapy, 56% at 12 months, and 51% at 24 months. These results confirm the experience that most CML relapses occur relatively early after therapy cessation. Duration of TKI therapy and MR4 correlated significantly with MMR status at six months. No significant association with MMR status at six months could be observed with respect to sex or variables of EUTOS resp. Sokal scores can be determined. Approximately 30% of patients experienced mostly transient musculoskeletal symptoms after discontinuation of the TKI.
No side effects, lower costs
Stopping TKI therapy not only saves CML patients from any side effects of TKI treatment, such as arterial hypertension, but also considerable costs. It is estimated that treatment with a TKI costs around 30,000-40,000 euros per patient per year in Europe. However, these costs do not simply drop to zero when therapy is stopped, as the patients in question must be followed up very closely. EURO-SKI first author Johan Richter (Lund, Sweden) emphasized in his presentation that stopping therapy in CML is still experimental and should only be done in the context of clinical trials.
Literature:
- Richter J, et al: Stopping tyrosine kinase inhibitors in a very large cohort of European chronic myeloid leukemia patients: results of the EURO-SKI trial. EHA21, 2016, Copenhagen, Abstract: S145.
InFo ONCOLOGY & HEMATOLOGY 2016; 4(5): 3.