Heart replacement procedures are increasingly important and highly effective therapeutic procedures for affected patients. Despite the progress made in recent years, they are still mistakenly seen as the “ultima ratio”. In this regard, it would be critical that referral to continuing therapy occur at the right time. After that, a professional and experienced treatment team is a prerequisite for good long-term results. Such a team is ideally composed of a specialized heart failure cardiologist, the cardiac surgeon, the VAD coordinator and perfusionist, the CHF/HTx/VAD nurse, and a psycho-cardiologist.
Heart failure (CHF) is primarily a disease of the advanced age population, where it reaches a prevalence of up to 10%. Across all age groups, the mean prevalence is 1-2% [1]. Despite its epidemic proportions and progressive deterioration in quality of life, as well as its poor prognosis in terms of survival, the importance of heart failure is massively underestimated compared to malignancies [2,3]. Typically, when a malignant neoplasm is present, patients are promptly referred to the medical specialist, the oncologist. The same is apparently not true in heart failure. European and Swiss data demonstrate that patients with evident heart failure are often not treated in an evidence-based manner or with the appropriate target dose of indicated medications [4,5]. The English NICE guidelines on chronic heart failure, compiled in large part by general practitioners, call for the early involvement of a heart failure cardiologist in the patient’s management once heart failure has been diagnosed [6,7]. After specialist assessment and agreement with the referring physician, the patient will then continue to be seen by the primary care physician, but will also be seen at intervals by the cardiologist specializing in heart failure. In addition to optimized medication, this also enables the necessary completion by heart failure counseling as well as a timely evaluation of whether further measures such as a heart replacement procedure should be pursued.
When and in whom is a heart replacement procedure indicated?
Unfortunately, despite the medical-technical developments of the last decade, it is wrongly assumed today that a heart replacement procedure is an “ultima ratio”. “Who needs something as rare as a heart transplant (HTx) or even an artificial heart? Certainly not the elderly population”. This or similar sounds the usual and in a certain sense understandable train of thought of many medical colleagues. Interestingly, there is a significantly greater receptiveness to other therapeutic options such as ICDs, CRTs, MitraClip® and TAVIs, although the associated therapeutic efficiency as well as the present costs do not differ in any relevant way.
A major problem is that quite a few colleagues are incompletely informed about the associated advantages and disadvantages of advanced heart failure therapy. Table 1 summarizes the characteristics of different heart replacement procedures.

Timely referral for advanced therapy is critical. Patients with incipient cardiorenal syndrome (GFR ≤60), incipient pulmonary arterial hypertension resp. Appearance of general weakness should be assigned at this time at the latest. The presence of cardiac cachexia or consecutive right ventricular dysfunction is a clear indication that advanced disease development is already present and may be more treatable at an earlier time.
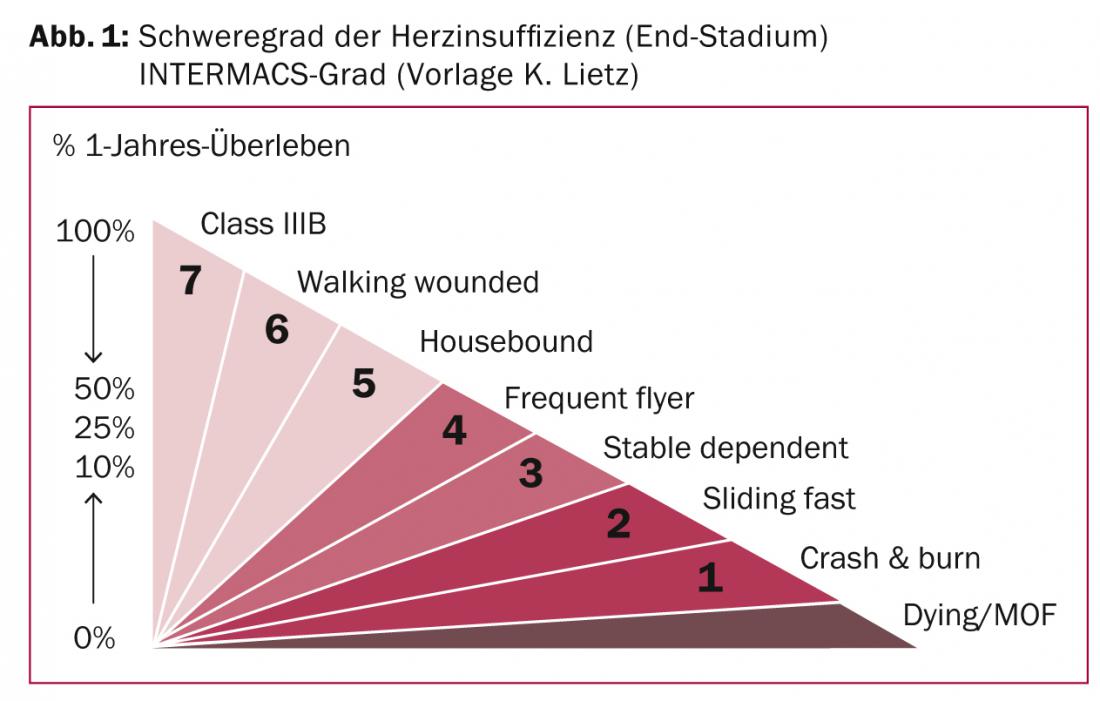
A relatively simple and low-risk implantation of a left-ventricular assist device (LVAD) with proven good outcome data is no longer readily available at this time. To ensure optimal therapy of patients with heart failure, it is worthwhile to use the so-called INTERMACS classification of clinical severity of heart failure (Fig. 1): INTERMACS grade 5 (so-called “housebound”) clearly requires the assessment of a heart failure specialist [8]. INTERMACS grades 3-4 present clinical conditions in which the indication for a heart replacement procedure must be evaluated.
Assessment of the patient at this stage of the disease includes evaluation of morbidity (quality of life) on the one hand and estimation of mortality (risk) on the other.
Parameters of morbidity are the frequency of hospitalization and exercise capacity, measured by the 6-minute walk test or, better, by spiroergometry (VO2maxdetermination) [9]. The VO
2
maximum value then also allows the so-called “Heart Failure Survival Score” (HFSS, according to Aaronson-Mancini) to be determined [10]. The HFSS can be calculated in the simplest way using the “Mediquations” app. Regarding the HFSS, however, it remains to be noted that the calculated risk is estimated without the ICD, which is almost always required. Also, the proven, good prognostic significance of the BNP value is not taken into account.
In patients without a VO2 maximum value, the Seattle Heart Failure Model value can be used for risk assessment(www.seattleheartfailuremodel.org).
Cardiac Support Pumps
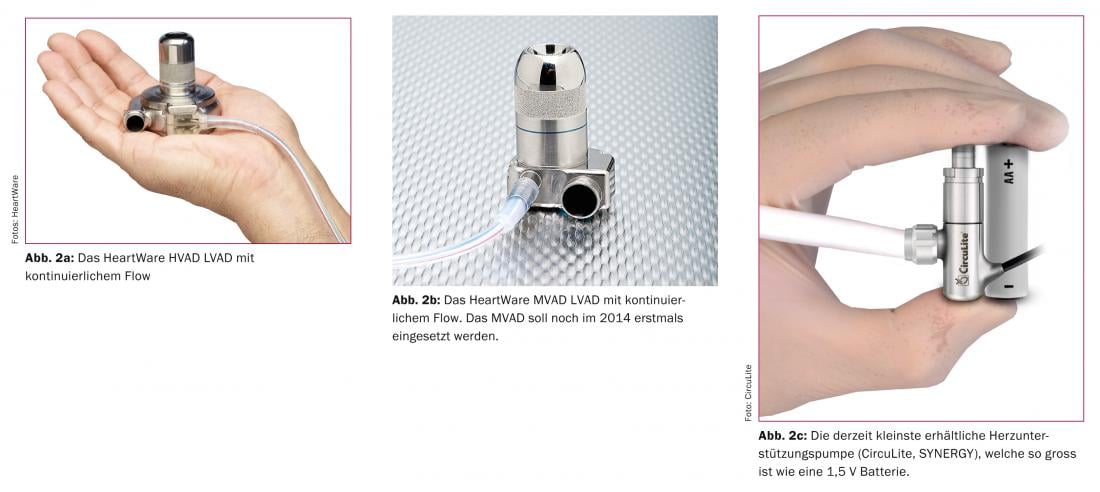
Cardiac assist pumps are now part of everyday clinical practice and by no means just fiction. In this respect, we are in a period similar to the introduction phase of pacemakers or ICDs. Cardiac assist pumps are becoming more reliable and smaller. Their advantages and disadvantages are summarized in Table 1.
Major complications of long-term use of fully implantable cardiac assist pumps are the risk of infection at the exit point of the so-called “drive line”, the cable which transcutaneously ensures the energy demand of the pumps, as well as thromboembolic or hemorrhagic problems. Although not yet optimal in the current setting, it is only a matter of time before the cumbersome cables give way to a transcutaneous power supply for the mechanical support systems. The risk of thromboembolism will also be reducible in the foreseeable future with the introduction of new bio-tissue materials. Cardiac assist pumps are getting progressively smaller, as shown in Figure 2a-c .
Heart transplant
Heart transplants have now been successfully performed for 45 years. Thanks to modern immunosuppressants, the side effects of the highly effective drugs are well tolerated, especially when used in combination and thus at low doses. The performance of patients with a transplanted heart is still better compared to mechanical heart assist pumps. However, in the therapeutic option of heart transplantation, the main problem to be mentioned is the limited availability of donor hearts. This leads to long waiting times for a donor organ and therefore a heart support pump often has to be implanted as a bridge (“bridge to transplant”) until a possible heart transplantation. Occasionally, patients become so accustomed to the heart assist pump during this waiting period and achieve a correspondingly satisfactory to high quality of life that in individual cases they even decide against a subsequent heart transplant.
Literature:
- Mohacsi P, et al: Prevalence, increase, and costs of heart failure Heart and Metabolism 2001; 14: 9-16.
- Stewart S, et al: More malignant than cancer ? Europ J Heart Fail 2001; 3: 315.
- Cowie MR, et al: Heart 2000; 83: 505-510.
- Harjola VP, et al: Characteristics, outcomes, and predictors of mortality at 3 months and 1 year in patients hospitalized for acute heart failure. Eur J Heart Fail 2010; 12: 239-248.
- Luthi JF, et al: Swiss Med Wkly 2006; 136: 268-273.
- www.nice.org.uk/nicemedia/live/13099/50526/50526.pdf.
- www.nice.org.uk/nicemedia/live/13099/50517/50517.pdf.
- Stevenson LW, et al: INTERMACS Profiles of Advanced Heart FAilure: The Current Picture. J Heart Lung Transplant 2009; 28: 535-541.
- Lucas C, et al: The 6-min walk and peak oxygen consumption in advanced heart failure: aerobic capacity and survival. Am Heart J 1999; 138: 618-624.
- Aaronson KD, et al: Development and prospective validation of a clinical index to predict survival in ambulatory patients referred for cardiac transplant evaluation. Circulation 1997; 95: 2660-2667.
CARDIOVASC 2014; 13(3): 8-10











