Pneumonia remains a common and deadly infectious disease. Nearly 40,000 patients are hospitalized in Switzerland each year for pneumonia, and a good 1,000 people die each year as a result of this disease. Most of the time, the diagnosis can be made easily with the help of clinic, X-ray and laboratory and the pneumonia heals with antibiotics administration. In some cases, however, the clinic and course are atypical, and response with antibiotic therapy is delayed or absent.
The diagnosis of pneumonia is challenging. Different aspects such as clinical, laboratory and radiology can be highlighted. Community-acquired pneumonia is best diagnosed when several factors come together, explained Dr. Irène Laube, Head of the Department of Pneumology at the Stadtspital Triemli in Zurich [1]: It is an acute illness with cough and ≥1 finding:
- new focal lung lesions
- Fever >4 days
- Dyspnea and tachypnea (WITHOUT other cause)
- new filtrate in X-ray
In a usual course of pneumonia, with adequate antibiotic choice, there should be a marked improvement in the laboratory (especially CRP) in the first 48 hours, and after 4-5 days there is an immune response with clinical improvement after about a week. However, radiological improvement with decrease of infiltrates may take 4-6 weeks (Table 1) . However, a longer course may still be normal: If pneumonia does not resolve on radiography until about 5-8 weeks, this is not nonhealing pneumonia. Instead, inadequate antibiotic therapy, multilobular localization, high CURB-65 score, comorbidities, or older age of the patient, for example, may explain slower healing.
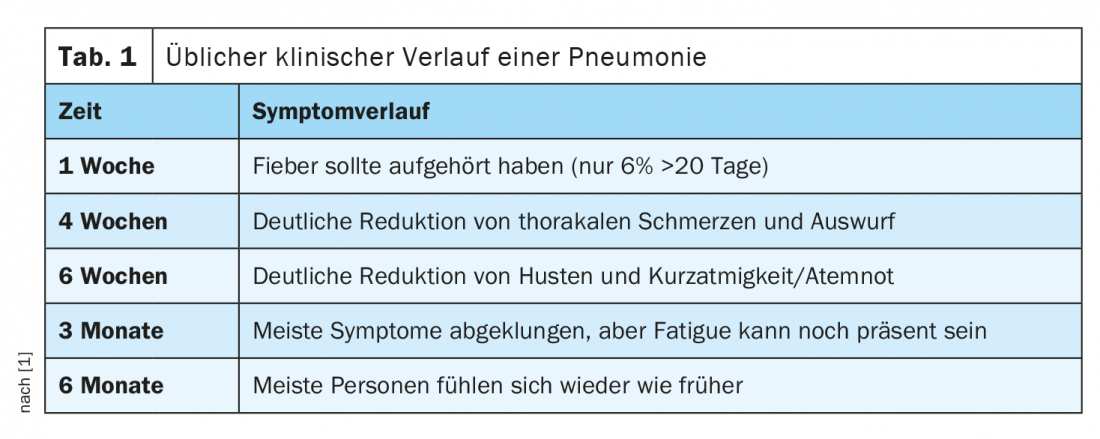
After 3 months, most symptoms of pneumonia should have resolved. If this does not occur, the pneumonia may be progressive or protracted. Primary or secondary treatment failure may also be present. – Or non-healing pneumonia may be present, but will not become apparent for several weeks.
What does non-resolving mean?
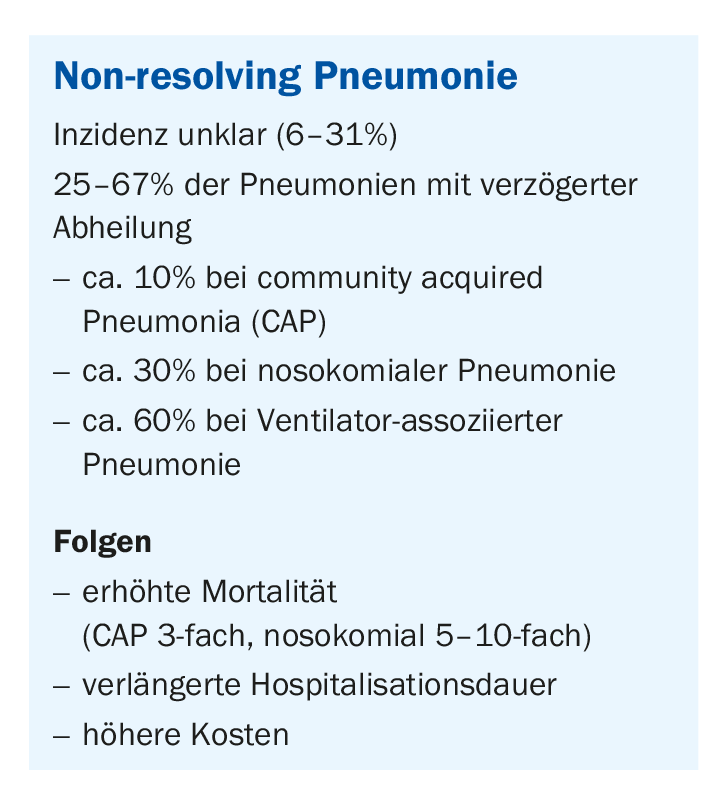
Non-resolving, or non-healing, pneumonia is usually a radiologic definition, but this is not uniformly defined. The time factor is important in such cases: after 4 weeks, at least two-thirds of the infiltrates should have receded so that one can speak of a delayed but still normal course. Such a situation does not occur so rarely, Dr. Laube reported. Commonly (15-25%) found in hospitalized patients who have had nosocomial pneumonia. In patients with ventilators who were mechanically ventilated, it is found in as many as 60% of cases (box) .
Non-healing can also mean persistent symptomatology, as is increasingly seen in COVID-19 patients. The symptoms decrease significantly in intensity after 2 weeks, but then continue for several months. Patients complain of symptoms, but the laboratory is inconclusive and nothing can be found on X-ray. The risk factors in slow healing can have a mortality increase of 17.74% after one month and a 60-day mortality up to even 25.81%, the expert warned. Therefore, slow healing implies an independent risk factor for 60-day mortality.
Procedure for non-resolving pneumonia
Diagnosis is initially based on the patient’s medical history, which highlights various aspects such as medication and antibiotic use, dosage or stay abroad (tab. 2) . According to Dr. Laube, if the patient can provide sputum, it is worthwhile to examine it for microbiology. At the onset of pneumonia, this usually does not happen. Blood cultures are recommended if fever is present, and urine should be tested for Legionella antigen if Legionella pneumonia is suspected. However, it should be noted here that false-negative results may occur. In most cases, bronchoscopy and bronchoalveolar lavage (BAL) for further diagnosis are not feasible to search for rare pathogens such as mycobacteria, viruses, Legionella, Nocardia, fungi, cell differentiation and other causes.
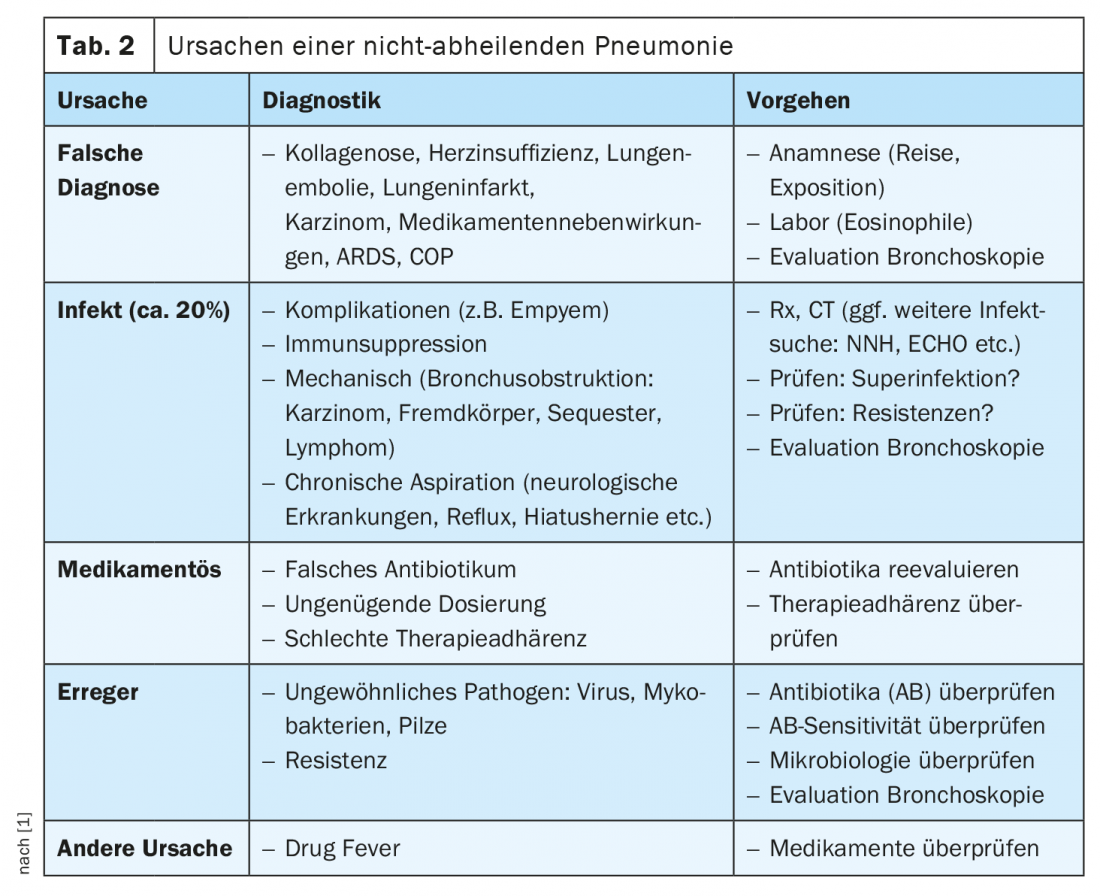
Early pleural ultrasonography is very important to avoid missing an empyema, he said. In particular, patients with pneumococcal pneumonia may develop early empyema, which may be septated and then inaccessible to simple drainage. Should this occur, the thoracic surgeon must be consulted. A pleural effusion that is caught early can be drained or punctured.
A CT thorax can also help in the diagnosis. If an enlarged heart is apparent in a chest radiograph, pneumococcal pneumonia must also be thought of as pericardial empyema. Echocardiography is then the next step. In addition, immunosuppression should be excluded.
CT thorax, Dr. Laube concluded, thus forms an add-on aid before bronchoscopy when abscess formation or fungal infection is present or a tumor is suspected. However, in the case of bronchoscopy, current data are unclear as to whether it has an impact on patient mortality, he said.
Congress: 60th Medical Congress Davos – Online event
Source:
- Workshop “The non-healing pneumonia”; 60th Medical Congress Davos – Online event, 11. February 2021.
InFo PNEUMOLOGY & ALLERGOLOGY 2021; 3(3): 22-23.