Prof. Dr. med. Jörg Leuppi, Cantonal Hospital Baselland, spoke at the SGAIM Congress in Basel on the treatment goals of COPD therapy. Does medication prevent disease progression, or even prolong survival? Or are such effects still mainly attributable to smoking cessation? And what about symptomatic treatment? These and other issues were addressed in the presentation.
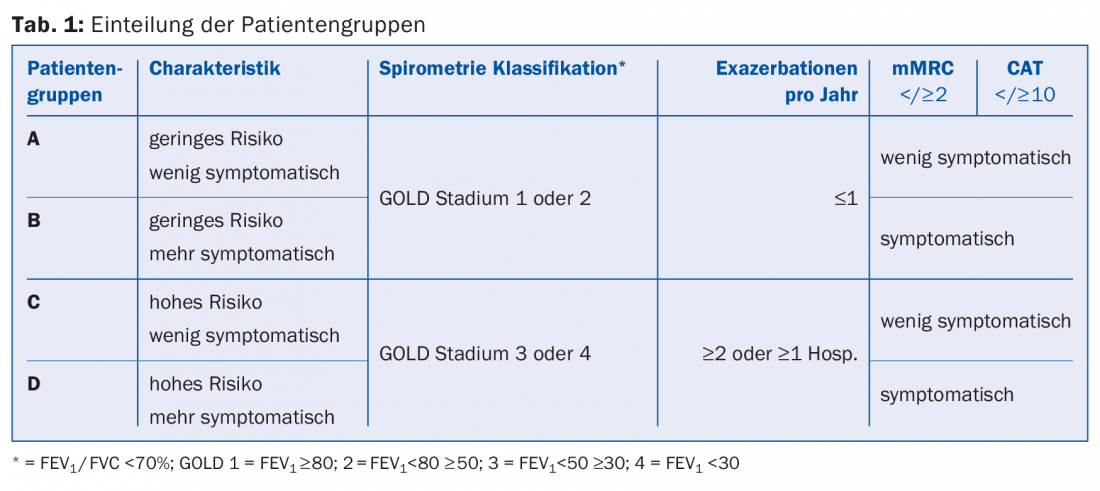
First, the ABCD classification of the different COPD patient groups was discussed. “It can be said that the new multidimensional phenotyping of COPD (Tab. 1) gives the patient a face,” explained Prof. Jörg Leuppi, MD, Kantonsspital Baselland. “Where in the past, treatment was based only on lung function, now symptomatology is included.” Depending on the severity, different first-line therapies are recommended:
- A: short-acting anticholinergic if needed or short-acting β-2-agonist if needed.
- B: long-acting anticholinergic (LAMA) or long-acting β-2-agonist (LABA).
- C: long-acting anticholinergic (LAMA) or long-acting β-2-agonist (LABA) + inhaled corticosteroid (ICS).
- D: long-acting anticholinergic (LAMA) and/or long-acting β-2-agonist (LABA) + inhaled corticosteroid (ICS).
“Whereas I suspect that in the future we will be limited to a B and D classification, since we almost never encounter A and C patients in everyday practice,” Prof. Leuppi noted.
What can we achieve?
The aim of therapy is, on the one hand, to prevent the progression of COPD, i.e. to halt the additional loss of lung function (in addition to that due to aging) and thus, optimally, also to reduce mortality. By what means is the latter possible?
Smoking cessation: “Obvious, well-tried, but not always easy to achieve is smoking cessation – best factor for survival. This has been shown many times, e.g. by Anthonisen and colleagues in 2005 [1],” Prof. Leuppi emphasized.
Oxygen therapy: An older, now ethically questionable study [2] also showed a mortality benefit for oxygen therapy. Oxygen was indicated in all 87 patients (pO2 <55 mmHg), and only some received it. Those who did not receive it were more likely to die during five years of follow-up than those with oxygen therapy over 16 h/d. Thus, when indicated, oxygen therapy is life-prolonging, it concludes.
Inhalation therapy: “With inhalation therapy, on the other hand, we cannot prolong life,” explained Prof. Leuppi. “The 2007 TORCH trial [3] of salmeterol and fluticasone narrowly missed its primary endpoint (mortality), but it missed it: the reduction in all-cause mortality with the combination versus placebo was 17.5% with a P value of 0.052.”
And the lung function? Again, quitting smoking is critical. If it succeeds, the loss of function can be slowed down. “It is perfectly normal that we lose lung function continuously from the age of 40 to 45. Smoking accelerates this process considerably if one is sensitive to it, which is the case for about one third of smokers. If one stops, the progression slows even at older ages (and then progresses again at the natural rate of decline) [4].”
Drugs may also exert a significant effect on disease progression, but the results here are less consistent [5,6].
Improve everyday life
Another important therapeutic goal is the least possible restriction of everyday life, i.e. little shortness of breath, no to rare exacerbations and more quality of life. The leading clinical findings of COPD – cough, sputum, slowly increasing dyspnea (exertional to resting dyspnea) and, depending on the phenotype, weight loss and depression – can be addressed with medication. “No human being is ever completely deflated; there is always a residual volume in the lungs, even with full exhalation. But because the lungs are overinflated in COPD, i.e. when the residual volume increases, the possible inhalation volume automatically decreases. Symptomatic patients therefore need bronchodilation. This therapy improves dyspnea, as indicated by the Transient Dyspnea Index [7],” explained Prof. Leuppi. Combinations are even more effective in this [8]. They lower the residual volume, there is less “trapped air”, which facilitates breathing [9].
COPD exacerbations should be prevented, as each exacerbation increases the likelihood of another. The periods between exacerbations shorten and mortality increases. “For the prevention of exacerbations, anticholinergics are in principle more suitable than beta-2 sympathomimetics [10]”, the speaker noted. “But the most effective is the combination [11]. The principle is that symptomatic COPD patients need bronchodilation. When monotherapy is not sufficient, dual bronchodilation helps. What they don’t seem to necessarily need is an additional inhaled steroid, as a recent study [12] showed: exacerbations are significantly less likely to be avoided with salmeterol-fluticasone than with dual bronchodilation.” In the WISDOM study [13], the number of exacerbations remained the same even when corticosteroids were gradually discontinued under dual bronchodilation. However, with complete cessation of corticosteroid therapy, lung function then deteriorated.

The current long-acting “fixed-dose” combinations (LAMA/LABA or dual bronchodilator) are listed in Table 2.
Source: SGAIM Congress, May 25-27, 2016, Basel
Literature:
- Anthonisen NR, et al: The effects of a smoking cessation intervention on 14.5-year mortality: a randomized clinical trial. Ann Intern Med 2005 Feb 15; 142(4): 233-239.
- Report of the Medical Research Council Working Party: Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Lancet 1981 Mar 28; 1(8222): 681-686.
- Calverley PM, et al: Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007 Feb 22; 356(8): 775-789.
- Fletcher C, Peto R: The natural history of chronic airflow obstruction. Br Med J 1977 Jun 25; 1(6077): 1645-1648.
- Tashkin DP, et al: A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 2008 Oct 9; 359(15): 1543-1554.
- Troosters T, et al: Tiotropium as a first maintenance drug in COPD: secondary analysis of the UPLIFT trial. Eur Respir J 2010 Jul; 36(1): 65-73.
- Donohue JF, et al: Once-daily bronchodilators for chronic obstructive pulmonary disease: indacaterol versus tiotropium. Am J Respir Crit Care Med 2010 Jul 15; 182(2): 155-162.
- Mahler DA, et al: Dual bronchodilation with QVA149 reduces patient-reported dyspnea in COPD: the BLAZE study. Eur Respir J 2014 Jun; 43(6): 1599-1609.
- Beeh KM, et al: The 24-h lung-function profile of once-daily tiotropium and olodaterol fixed-dose combination in chronic obstructive pulmonary disease. Pulm Pharmacol Ther 2015 Jun; 32: 53-59.
- Vogelmeier C, et al: Tiotropium versus salmeterol for the prevention of exacerbations of COPD. N Engl J Med 2011 Mar 24; 364(12): 1093-1103.
- Wedzicha JA, et al: Analysis of chronic obstructive pulmonary disease exacerbations with the dual bronchodilator QVA149 compared with glycopyrronium and tiotropium (SPARK): a randomised, double-blind, parallel-group study. Lancet Respir Med 2013 May; 1(3): 199-209.
- Wedzicha JA, et al: Indacaterol-glycopyrronium versus salmeterol-fluticasone for COPD. N Engl J Med 2016 May 15. [Epub ahead of print].
- Magnussen H, et al: Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med 2014 Oct 2; 371(14): 1285-1294.
HAUSARZT PRAXIS 2016; 11(7): 40-41