A large multicenter study led by the DKFZ-Hector Cancer Institute at the University Medical Center Mannheim confirms substantial differences in treatment response and provides important insights for treatment planning.
Lung cancer is one of the most common malignant diseases in Germany. As a rule, malignant growth of cancer cells is based on changes in the genetic material. Such changes, summarized as driver mutations, can be manifold: from the simple exchange of DNA building blocks to the loss of gene segments to fusions, rearrangements or duplications of genetic material.
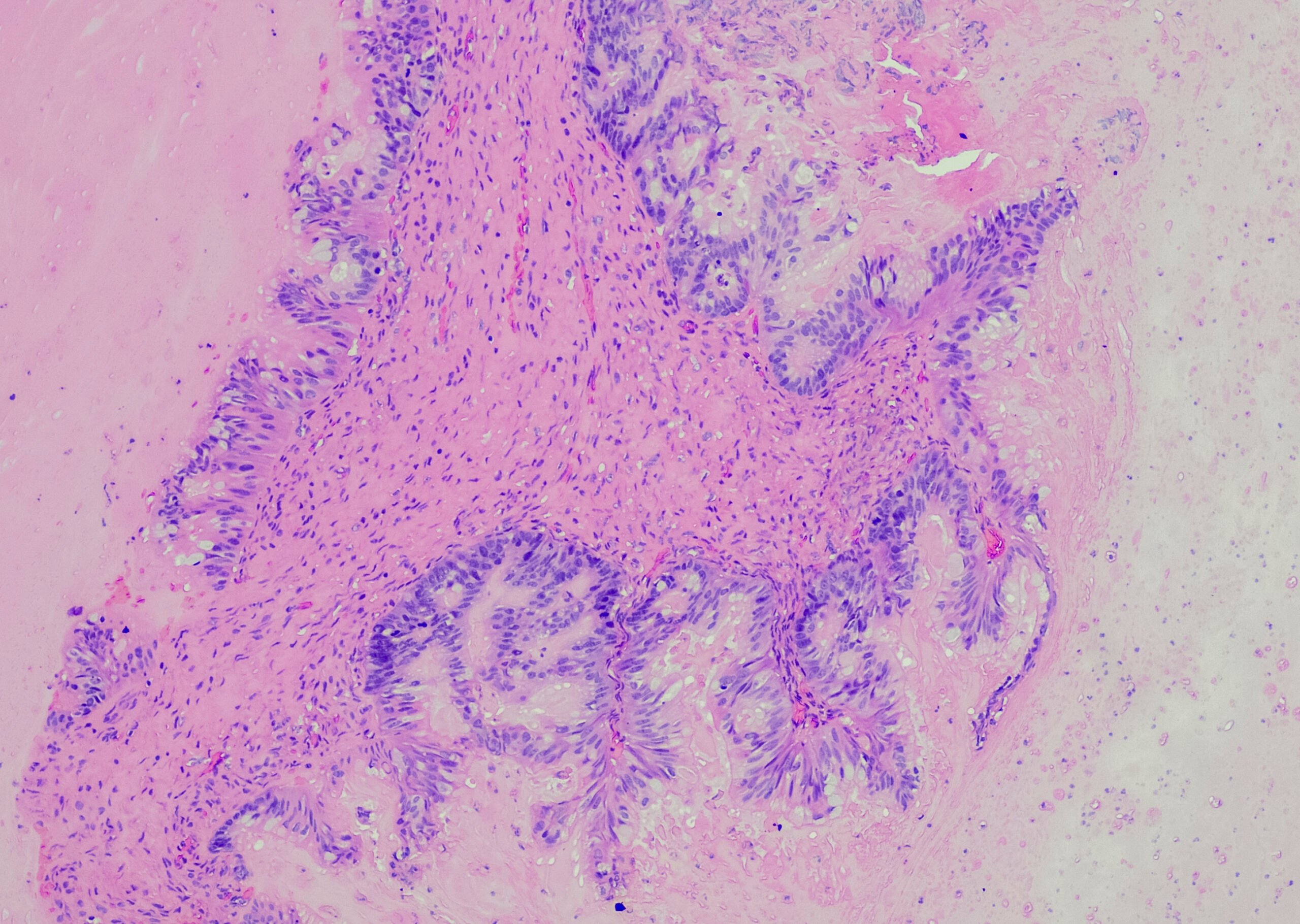
Non-small cell lung cancer (NSCLC) develops from epithelial cells of the lung. It accounts for three-quarters of all lung cancers and is one of the leading causes of cancer-related death. The most common alterations in non-small cell lung cancer include various mutations in the epidermal growth factor receptor (EGFR) gene, some of which occur in combination. The mutations cause increased growth signals to be received and transmitted into the cell interior, which leads to uncontrolled proliferation of the tumor cells.
Systemic therapy for non-small cell lung cancer includes chemotherapy and immunotherapies as well as targeted therapies with EGFR inhibitors, which bind to the EGF receptor and thus block growth signals. These drugs were developed for so-called classical EGFR mutations. Until now, it was unclear in which atypical or complex EGFR mutations, which affect 10 to 30 percent of patients depending on ethnicity, these drugs are also effective. In the past, this had only been studied in case reports or small case series.
However, in order to choose the optimal therapy, it would be important to know which of these patients would benefit from targeted therapy. NSCLC patients who are unlikely to benefit from treatment with EGFR inhibitors would be better treated with the otherwise standard chemotherapy combination.
Information is now provided by a retrospective multicenter study of the National Network Genomic Medicine (nNGM) in Germany, led by Professor Dr. Dr. Sonja Loges of the DKFZ-Hector Cancer Institute and the Department of Personalized Oncology at the University Medical Center Mannheim. In it, the scientists analyzed data from more than 850 patients with a total of 276 different, rare EGFR mutations and the response to the various systemic therapies: targeted EGFR therapy, chemotherapy and immunotherapy.
The study includes the largest group to date of NSCLC patients with very rare EGFR single and combination mutations treated with various systemic therapies. It clarifies whether or not EGFR inhibitors are effective in the variety of different activating EGFR mutations underlying non-small cell carcinomas, thereby helping to guide treatment decisions.
The scientists were able to show that especially NSCLC patients with previously hardly described, very rare point mutations as well as certain complex EGFR mutations – with two or more changes, one of which is a classic EGFR mutation – also benefit from EGFR therapies compared to chemotherapy.
“The data analyzed in the study from treatment outcomes of patients with rare EGFR mutations are of great importance when making treatment decisions in these patients,” said Melanie Janning, M.D., first author of the study. “To be able to collect such large data sets, a network like the nNGM is essential,” emphasizes Professor Loges, adding, “The results of our study have led to a new classification of lung cancer patients with rare EGFR mutations, which is highly relevant for therapy planning in clinical practice.”
Original publication:
M. Janning, J. Süptitz, C. Albers-Leischner, P. Delpy, A. Tufman, J.-L. Velthaus-Rusik, M. Reck, A Jung, D Kauffmann-Guerrero, I Bonzheim, S. Brändlein, H.-D. Hummel, M. Wiesweg, H.-U. Schildhaus, J. A. Stratmann, M. Sebastian, J. Alt, J. Buth, I. Esposito, J. Berger, L. Tögel, F. C. Saalfeld, M. Wermke, S. Merkelbach-Bruse, A. M. Hillmer, F. Klauschen, C. Bokemeyer, R. Buettner, J. Wolf*, S. Loges*: Treatment outcome of atypical EGFR mutations in the German National Network Genomic Medicine Lung Cancer (nNGM).
Ann Oncol. 2022 Mar 6; S0923-7534(22)00361-1; DOI: https://doi.org/10.1016/j.annonc.2022.02.225