Few patients with locally advanced laryngeal or hypopharyngeal cancer are spared surgical laryngectomy. This is because in such squamous cell carcinomas there is some uncertainty as to what effect non-surgical preservation of the larynx might have on survival prognosis – it is not uncommon for affected individuals to subsequently face laryngectomy or even death after all. Researchers from Leipzig therefore propose a new score for better decision-making.
In general, it is recommended that tumor response or tumor reduction be assessed by endoscope after one cycle of induction chemotherapy. The study authors around Prof. Gunnar Wichmann, MD, Clinic and Polyclinic for Otolaryngology/Plastic Surgery, University of Leipzig, supplemented this approach with a volume determination by CT and the results of a PET/CT.
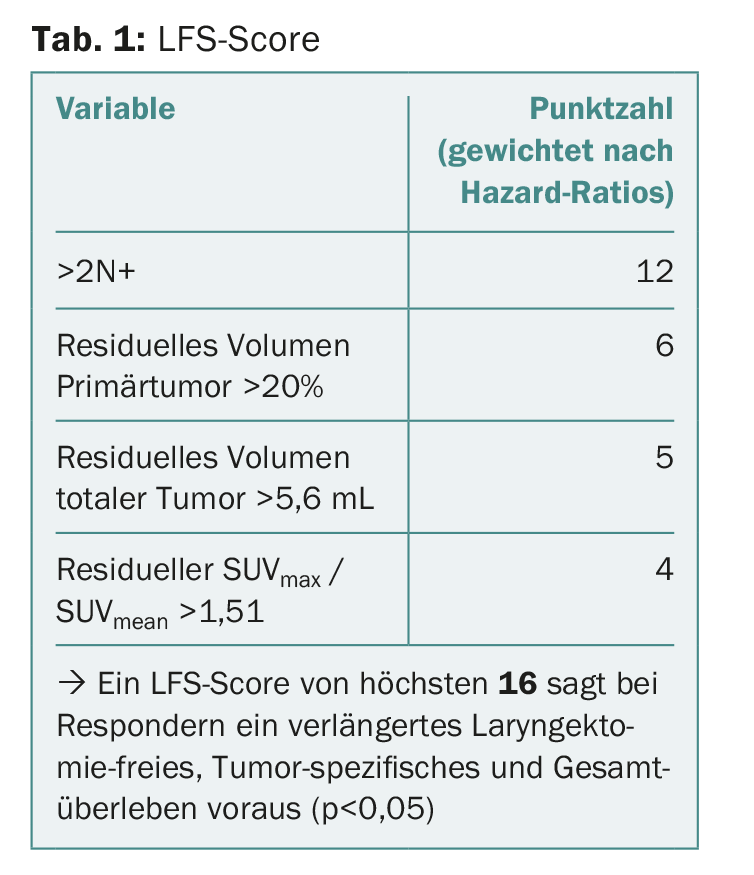
From this, they eventually formed a score that could be used to define certain patients as suitable for laryngectomy (because their prognosis of surviving longer without laryngectomy was significantly better than that of the rest of the patients). The score was based on hazard ratios, the odds of laryngectomy-free survival for each group.
Together with endoscopic examination, researchers say this score – in addition to the risk of subsequent laryngectomy – can predict which patients will live longer without dying from cancer or another cause. Decision making on whether to retain a larynx after one cycle of induction chemotherapy would be facilitated.
Derivation of the score
This much up front: responders with an endoscopic tumor reduction of at least 30% and a score of highest 16 have prolonged laryngectomy-free, tumor-specific, and overall survival. But what exactly does this score consist of?
The prospective study initially tested which tumors had an early response to induction chemotherapy according to regimen TPF (docetaxel, cisplatin, and fluorouracil ± cetuximab) in 52 patients. Non-responders were those with endoscopic tumor reduction of less than 30%. These underwent total laryngectomy. In all others, 39 of the 52 patients, induction chemotherapy was continued, along with radiation. In addition to endoscopic examination, CT was performed to measure the volume of the primary tumor and cervical lymph nodes, and 18F-FDG PET/CT was performed for a survey of the maximum and average standard uptake value (SUV).
Baseline and residual values after the first cycle of chemotherapy were correlated with laryngectomy-free, tumor-specific, and overall survival, resulting in the score in question. It showed:
- Non-responders who had undergone laryngectomy and responders with endoscopic tumor reduction greater than 70% had the best overall survival.
- Early response to the first cycle of therapy again predicted a complete response to subsequent induction chemotherapy plus radiation.
- The number of CT-graded positive cervical lymph nodes, the residual volume of primary and total tumor, and the ratio of residual maximum and average SUV were significant independent predictors of laryngectomy-free survival in responders-that is, these variables could be used to predict whether the patient has a good chance of surviving for an extended period without laryngectomy after responding to induction.
What is the “magic formula”?
The formula, or score, is shown in Table 1. Patients who do not exceed a score of 16 benefit most from nonsurgical laryngeal preservation because they survive for a long time without needing laryngectomy after all. Conversely, and the authors consider this to be almost the more important message, patients with scores above 16 are not suitable for maintenance with the study’s treatment regimen. It goes without saying that a validation of this score, which is to be understood as a suggestion for the time being, is now indicated.
Interdisciplinarity required
The relevance of the study and the score is self-evident: Preserving such an important organ as the larynx, which is closely linked to the character and identity of a person through the production of the voice, corresponds to the natural wish of the patient – but only if this does not severely limit his further prognosis. Selecting appropriate patients is therefore a first step towards personalized decision making and therapy. Apparently, you need not only the endoscope, but also a CT and a PET/CT. Interdisciplinary cooperation is therefore required. ENT physicians, radiologists, nuclear medicine specialists, radiation oncologists and pathologists must cooperate closely to make the optimal treatment choice together with the patient and under assessment of now better assessable risks.
Source: Wichmann G, et al: Induction chemotherapy followed by radiotherapy for laryngeal preservation in advanced laryngeal and hypopharyngeal cancer: outcome prediction after one cycle induction chemotherapy by a score based on clinical evaluation, computed tomography-based volumetry and 18F-FDG-PET/CT. EJC 2017; 72: 144-155.
InFo ONCOLOGY & HEMATOLOGY 2017; 5(4): 4.











