Urticaria is a diagnostic chameleon and a major therapeutic challenge. While the acute form usually disappears after a few days, chronic urticaria can persist for years. Therapy in both cases is usually with antihistamines. The search for the cause is particularly difficult: The spectrum ranges from physical factors to food-induced irritants to cross-reacting allergies. The physician can confirm the diagnosis with various test methods.
Acute urticaria (<6 weeks, usually 1-2 days) can be distinguished from acute recurrent urticaria (acute urticaria repeatedly). Chronic urticaria, which can also be recurrent (free intervals of days to weeks) or continuous (daily), lasts longer than six weeks in any case, and even longer than five years in about 50% of patients. Disease duration is usually shorter when treatment is started early [1]. A chronic spontaneous form (without an external physical trigger) and a chronic inducible form (with a detectable trigger) can be distinguished. In about 30-40% of cases, urticaria occurs together with angioedema (Fig. 1).
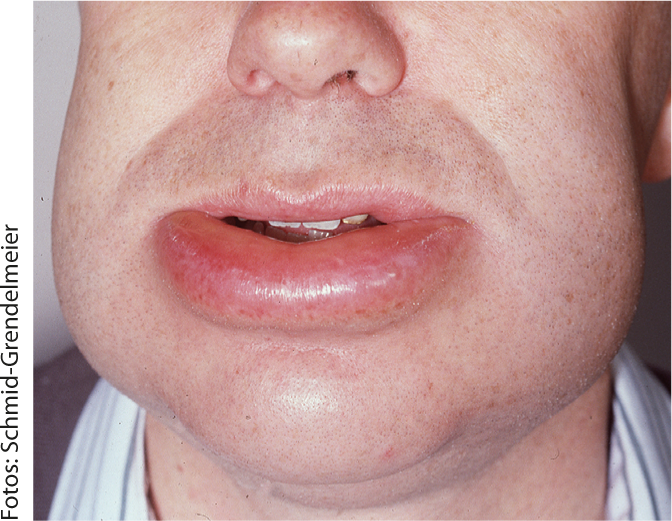
Fig. 1: Quincke’s edema
Acute urticaria
The acute form is very common: 15-25% of the population go through such an episode at least once in their lifetime. Patients look for the cause in food in over 60% of cases. While in acute recurrent urticaria, in addition to infections and medications, about 10% of cases are actually IgE-mediated, this is the case in less than 1% of the acute single form [2]. A special case and further evidence of the chameleon-like appearance of urticaria is tropomyosin cross-allergy. The protein tropomyosin, an allergen of crustaceans and molluscs, is cross-reactive to the allergen of the house dust mite. For example, individuals who consume seafood and subsequently experience an allergic reaction are affected [3].
In any case, a precise anamnesis is part of the diagnosis. If it is a one-time episode, no further clarification is needed. In case of recurrent occurrence, details of medications taken should be collected and the possibility of atopic disease should be checked. If necessary, allergological tests are conceivable here.
Symptomatic therapy is based on the administration of antihistamines (usual dosage: 1×/day for 3-5 days) and glucocorticosteroids (1 mg/kgKG, 2-3 days, then reduce). In addition, an emergency kit consisting of two tablets of prednisone 50 mg each and two tablets of an H1 blocker can be dispensed.
Chronic urticaria
The prevalence for both types of chronic urticaria is approximately 0.5-1.0% [4]. Women are affected almost twice as often as men, with the peak occurring between the ages of 20 and 40, usually in the working years.
Idiopathic, physical, cholinergic, and IgE-mediated causes, as well as urticarial vasculitis, infection, or hereditary angioedema, are all possible causes of chronic urticaria. Not infrequently, however, the specific trigger remains unclear and is difficult to determine. Interestingly, a case report of a 27-year-old REGA physician who repeatedly visited Southeast Asia and subsequently developed urticaria over two months showed an allergy to fish parasites as the most likely trigger (“sushi allergy”). The so-called herring worm (Anisakis) is partly contained in raw fish (sushi), can lead to abdominal pain, diarrhea and even urticaria or anaphylaxis. Specific IgE against anisakis are effective here.
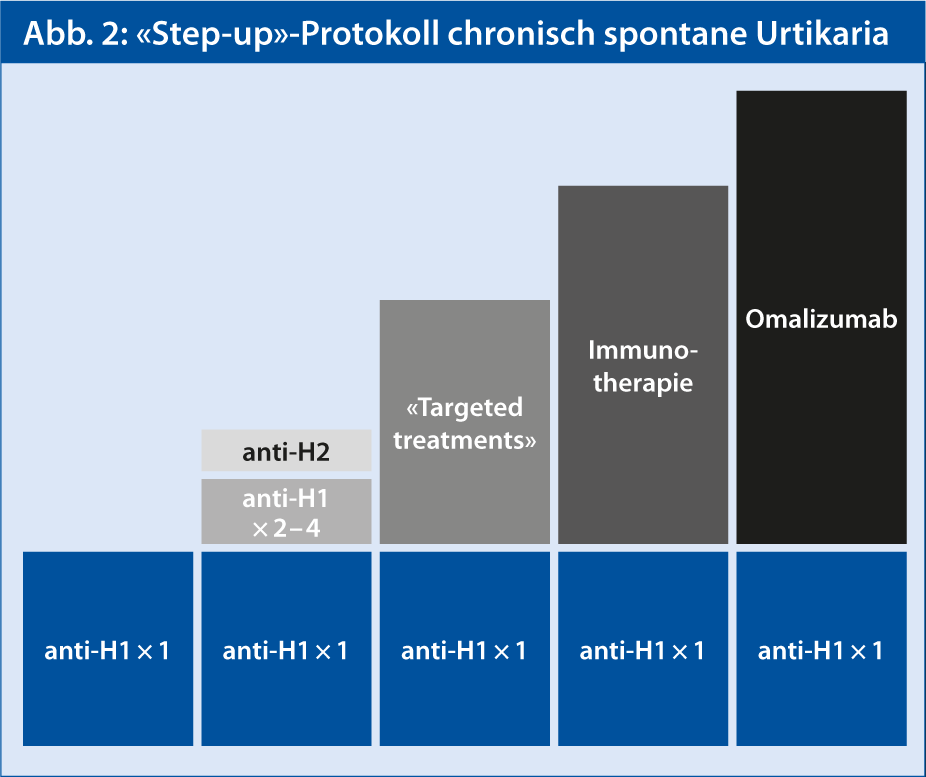
Therapy of chronic urticaria is primarily based on antihistamines (H1 blockers), in ascending doses. This treatment is successful in about 50-60% of patients with chronic spontaneous urticaria [5]. The “step-up” protocol highlights some additional options available for the therapy of such patients (Fig. 2). Immunomodulators such as omalizumab are currently in Phase III trials. Initial results on omalizumab show that it can act quickly and safely. In patients who were under-responsive to antihistamines, this effectively reduced clinical symptoms and signs of chronic spontaneous urticaria [6]. However, this is an off-label indication that requires a special cost approval.
Physical urticaria
Physical urticaria can be caused by pressure, friction, cold, heat, vibration, or light (especially UV radiation), among other things.
The most common physical cause of chronic urticaria is immediate mechanical pressure (urticaria factitia). The urticarial dermographism in urticaria factitia includes wheals appearing after shear force, with a delay of 1-5 min. show and are associated with itching (Fig. 3) . This makes it possible to “write” on the skin, in that the symptomatic elevations appear shortly after brushing the skin with a blunt object. Most often, this physical form of urticaria occurs in young adults, lasting on average a full 6.5 years.
Therapy is by means of non-sedating H1 antagonists, the efficacy of which has already been proven at low doses. Continuous therapy for at least two weeks is recommended. 4-6 weeks; if there is a response, it can be reduced gradually on a probationary basis. Dose reduction should be done every 4 weeks.
There is evidence that cold urticaria is associated with infections such as Lyme disease, syphilis, measles, varicella-zoster virus, hepatitis, glandular fever, HIV, giardasis, strongyloidosis, as well as neoplasia and autoimmune diseases. Routine diagnostics are performed using cold provocation and a sulfur test (ice cubes, cold water, or wind). An advanced diagnostic program may include laboratory tests (ESR/CRP, “Differential Blood Count”). This should rule out other diseases, especially infections.

Fig. 3: Urticaria factitia
The autoimmune urticaria, infections, allergy
The cause of autoimmune urticaria is autoantibodies against the IgE receptor. The diagnosis can be confirmed using the Autologous Serum Skin Test (“ASST”). When injected with autologous serum, after 30 min. characteristic wheals [7].
Infections with parasites can cause urticaria, especially in endemic areas. Bacteria and worms, which are also responsible for gastrointestinal problems, are commonly found in rural, tropical areas and less commonly in industrialized areas. These parasites should always be treated when gastrointestinal symptoms are also present, when patients originate from or enter endemic regions, in the case of amebiasis, or when no other causes of urticaria can be found.
Allergies as triggers are rather rare in chronic urticaria. Nevertheless, there are examples such as the so-called. “Wheat-dependent, exercise-induced anaphylaxis” (WDEIA), which is measured by increased sensitivity of specific IgE antibodies to the wheat component rω-5 gliadin [8].
Mastocytosis
Mastocytosis is also associated with urticarial skin lesions. In the cutaneous form, mast cell collections occur in the skin; in the systemic form, the bones, blood, gastrointestinal as well as cardiovascular organs are also affected. Danger is also posed by insect bites, which can result in severe anaphylaxis if the patient is also allergic.
Literature:
- Van der Valk PG, et al: Br J Dermatol 2002; 146: 110-113.
- Chong SU: Int Arch Allergy Immunol 2002; 129: 19-26. doi:10.1159/000065181.
- Kütting B, Brehler R: Dermatologist. 2001; 52: 708-711.
- Maurer M, et al: Allergy 2011 Mar; 66(3): 317-30. doi: 10.1111/j.1398-9995.2010.02496.x. Epub 2010 Nov 17.
- Kaplan AP: Allergy Asthma Immunol Res 2012 Nov; 4(6): 326-31. doi: 10.4168/aair.2012.4.6.326. Epub 2012 May 14.
- Maurer M, et al: N Engl J Med 2013 Mar 7; 368(10): 924-35. doi: 10.1056/NEJMoa1215372. Epub 2013 Feb 24.
- Konstantinou GN, et al: Allergy 2009 Sep; 64(9): 1256-68. doi: 10.1111/j.1398-9995.2009.02132.x. Epub 2009 Jul 24.
- Matsuo H, et al: Allergy 2008; 63(2) : 233-236.











