The use of medicinal cannabinoids that are reimbursable through health insurance has come a long way in recent years. This is also reflected in various consensus statements and current guidelines. An overview of current recommendations was presented at the German Pain Congress in Mannheim.
There are several reimbursable cannabis active ingredients on the market that are derived from the hemp plant. First and foremost is dronabinol (tetrahydrocannabinol, THC), which is the pure substance for the production of prescription drugs, so it is free of other substances. In Switzerland, it is mainly used for chronic and/or neuropathic pain and spasticity. Nabiximols is available as an on-label oral spray for the treatment of painful spasticity, e.g. in MS. However, some patients report that it causes irritation of the oral mucosa. Nabiximols consists of a THC:CBD (cannabidiol) ratio of 2.7:2.5. Cannabis extracts contain defined ratios of THC to CBD, similar to nabiximols, but in addition all other ingredients extracted from the cannabis plant, such as terpenes. Nabilone is a synthetic derivative of THC and is available in North America and also Germany as 1mg capsules on label for nausea and vomiting after chemotherapy. However, the drug is not registered in Switzerland.
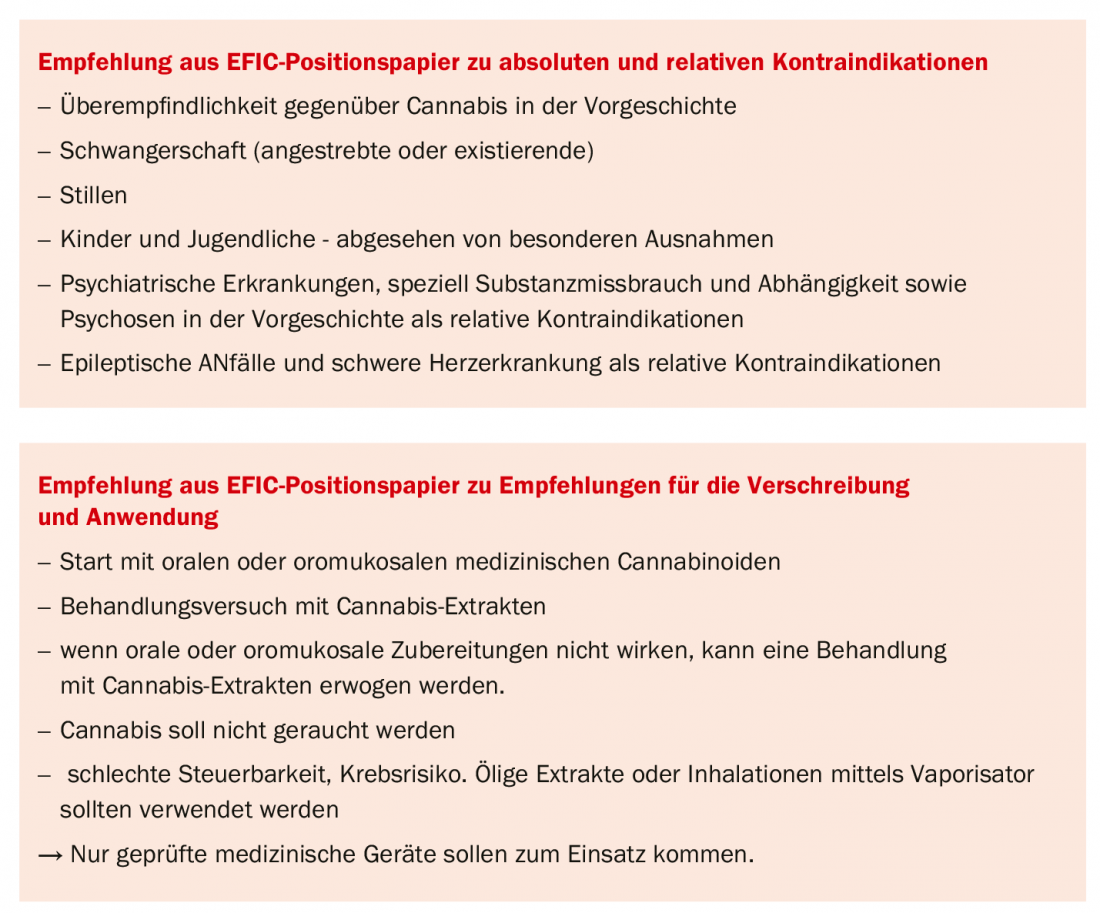
Finally, cannabis flowers are available for preparation in inhalers, as tea, pastries, or even for smoking. But here caution is required with regard to the correct dosage. “I am cautious with flowers. The rapid flooding through inhalation and vaporization results in a peak after 60-120 seconds – but I don’t want that at all in a pain therapy,” Prof. Dr. Roman Rolke, specialist in neurology, additional qualification in palliative medicine, Clinic for Palliative Medicine at the University Hospital RWTH Aachen, pointed out. Extracts or oily drops, on the other hand, provide a slow onset, which allows for better control in chronic pain. In tumor pain alone, there is a recommendation to always co-prescribe a fast-acting requirement. This is not true for other chronic forms of pain.
Caution with cannabis flowers
The neurologist acknowledged that there are certainly situations in which the flowers work individually and can be a good solution. In the case of frequent, prolonged spasticity, for example, Prof. Rolke can well imagine an application, as well as in certain resorption disorders, e.g. patients with ileus due to cancer, in whom oral intake is no longer reasonably possible and inhalation offers an alternative. But in general, he also has concerns about accuracy in flower application and about smoking: “A lot of patients smoke the flowers without a filter – and that carries a significantly increased risk of cancer, even over regular smokers. Also, as a tea or a pastry, you often don’t get the right temperature to extract all that’s in the flower.”
Indications in hospice and palliative work
Medicinal cannabinoids are indicated for lack of appetite, anxiety, pain, nausea, and vomiting. Not however with depression, there are effective anti-depressants available, as the expert explained. “But if someone is feeling very bad, there is of course nothing to say against simply taking the mood-lifting effect.” In the practice guideline Cannabis in Pain Therapy of the German Society for Pain Medicine (DGS), the authors write that pain in particular is an important indication in many areas: Spastic pain (in MS), chronic pain, tumor pain, non-tumor-related pain, and neuropathic pain are all assigned recommendation grade A (= high). Sleep disorders in chronic pain, visceral pain rheumatologic pain, muscle pain, and fibromyalgia with recommendation grade C.
Other indications in the guideline: chemotherapy-induced nausea, Tourette’s syndrome, but also glaucoma, dystonia, Parkinson’s disease, dementia, ADHD, respiratory diseases, irritable bowel syndrome. In contrast, there is no clear recommendation for the indications bladder dysfunction and epilepsy [1]. Basically, Prof. Rolke feels that the long list of A recommendations is a bit too optimistic. Other guidelines, such as those of the German Pain Society, are more cautious – which the physician feels is justified in view of the studies. “We’re certainly allowed to be optimistic for our patients, but we should be careful not to pour it all out on them.”
Literature:
- Horlemann J, et al: DGS Practice Guideline Cannabis in Pain Management 2018.
- Häuser W, et al: Eur J Pain 2018; 22: 1547-1564.
Source: Industry Symposium “Update Medical Cannabis – From Consensus Statements to Experiences in Practice” at the Rahman of the German Pain Congress 2019 in Mannheim (D); Organizer: Tilray.
HAUSARZT PRAXIS 2019; 14(11): 36 (published 11/21/19, ahead of print).
InFo PAIN & GERIATURE 2019, 1(1): 26-27.











