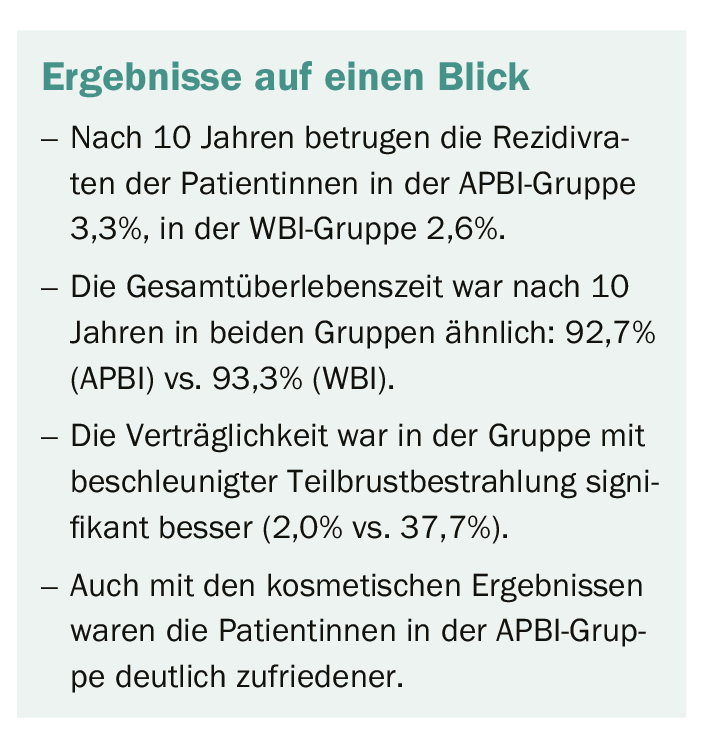
Results of a 10-year follow-up show that partial breast irradiation should become the new standard of care for patients with early, low-risk breast cancer. This is because there are significantly fewer adverse events with better cosmetic results compared to whole breast irradiation.
Many patients diagnosed with early breast cancer undergo lumpectomy followed by radiation. Postoperative radiation remains a mainstay of adjuvant breast cancer treatment, capable of significantly reducing local recurrence rates. In recent years, researchers have tried to determine whether partial-breast irradiation might be as effective as full-breast irradiation in preventing recurrences. A 10-year follow-up study of patients with breast cancer who had received accelerated partial breast irradiation (APBI) after surgery now showed that their disease recurrence rates were similar to those of patients who had received whole breast irradiation (WBI).
The Phase III trial, which included 520 patients with early-stage breast cancer, aimed to determine the long-term efficacy, safety and cosmetic outcomes of partial or total breast irradiation. All enrolled patients were at least 40 years old and had a maximum pathological tumor size of 25 mm. Patients were randomized in a 1:1 ratio to receive either whole breast irradiation (WBI) at a dose of 50 Gy in 25 fractions, followed by 10 Gy in five fractions delivered to the tumor bed or APBI delivered to the tumor bed at a dose of 30 Gy in five daily fractions. The primary endpoint was recurrence of ipsilateral breast tumor (IBTR). Secondary endpoints were overall survival, breast cancer-specific survival, distant metastasis-free survival, locoregional recurrence, and contralateral breast cancer. Adverse events and cosmetic aspects were also evaluated.
Five-year data confirmed
Interim results published after five years showed no significant difference in survival rates or IBTR between treatment techniques, and the results of the present 10-year analysis confirmed these. No significant differences were observed between groups for any of the primary or secondary endpoints, indicating that the main efficacy outcomes were not affected by the type of irradiation. Overall survival at 10 years showed 92.7% for women treated with APBI and 93.3% for those receiving WBI. Breast cancer-specific survival was 97.6% for women who received APBI and 97.5% for women who received WBI. The distant metastasis-free survival rate was 96.9% for both groups.
Better tolerance with more beautiful results
However, the safety profiles and cosmetic outcomes differed significantly. Adverse events of all severities occurred significantly more frequently with WBI than with APBI. Acute adverse events grade 2 or higher occurred in 37.7% of patients treated with WBI compared with only 2.0% of patients treated with APBI. The rate of grade 2 or higher adverse events remained significantly higher in the late phase in the WBI group than in the APBI group, although with a smaller margin than in the acute phase (2.7% versus 0%). Skin toxicity rates followed a similar pattern, favoring APBI in both the acute phase (66.5% vs. 21.1%) and the late phase (30.0% vs. 4.5%). In further support of APBI, cosmetic outcomes, as measured by the Harvard Breast Cosmetic Scale, were significantly better in the APBI group than in the WBI group. Both physicians and patients were significantly more likely to report good or excellent cosmetic outcomes with APBI than with WBI.
Source: www.abstractsonline.com/pp8/#!/7946/presentation/1921;
SABCS 2019
InFo ONCOLOGY & HEMATOLOGY 2020, 8(1): 30 (published 2/24/20, ahead of print).