Models of human skin produced by 3D bioprinting have already found their way into medical research. However, further research efforts are needed to open up this technological achievement for immediate clinical therapeutic application.
The skin of laboratory animals differs in its biological properties from human skin [1]. This concerns, for example, the thickness of the epidermis in murine skin or the dermal contractility after wounding. A three-dimensional human full-thickness skin model has already been established as an in vitro test system in biomedical research [1].
Wound healing as an application area for 3D bioprinting
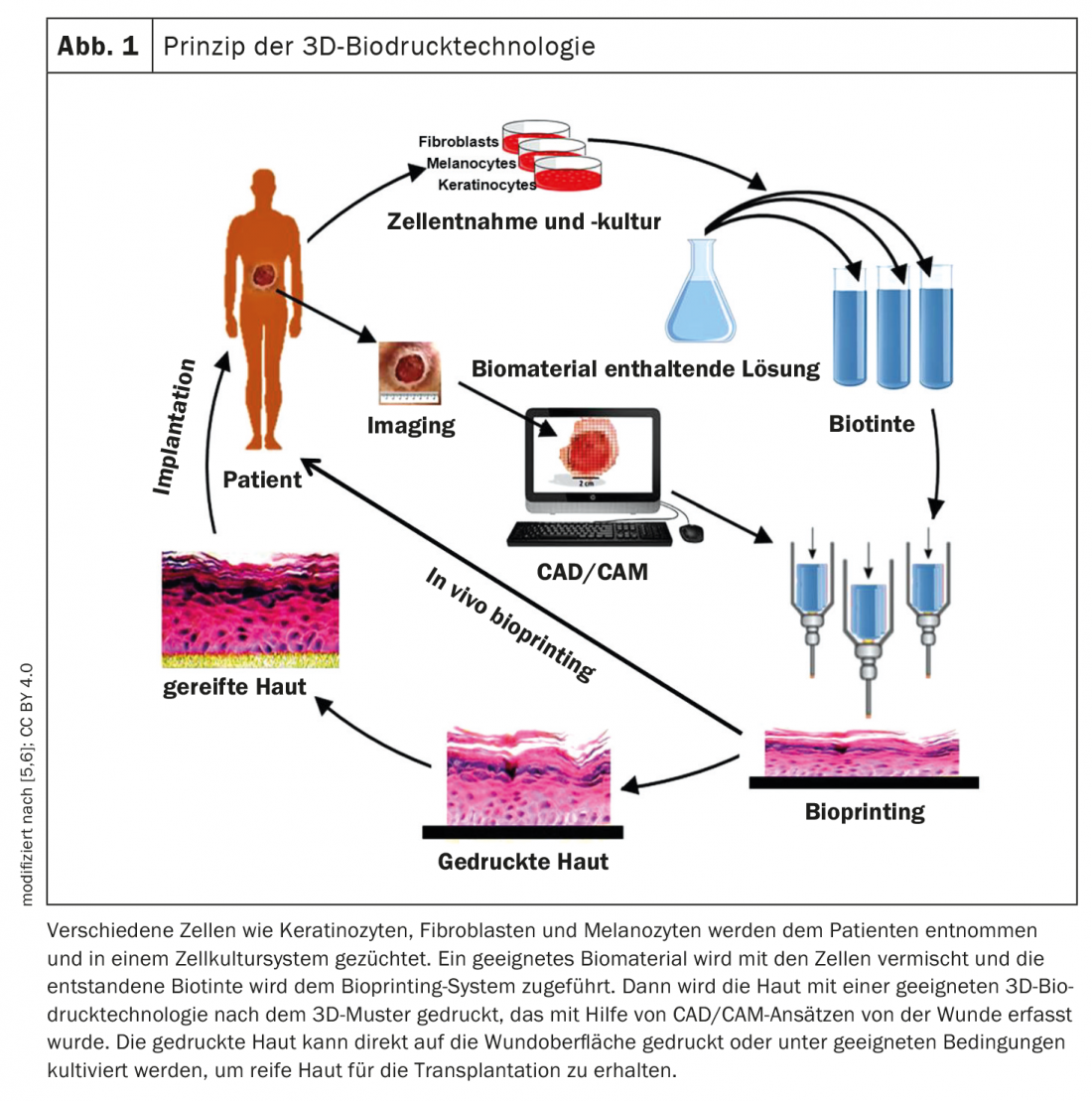
Mapping the wound is a prerequisite for creating a bionic structural model [5,6]. Three-dimensional modeling and digital image processing technology are then used to obtain morphological information about the skin defect, and a layered skin model is created by adaptive layering methods to generate appropriate pressure commands (Fig. 1) [7]. Subsequently, skin samples are taken from the patient to obtain keratinocytes and dermal fibroblasts for subsequent cell sorting and enrichment [8]. An optimal ratio of cell suspension and hydrogel is used to produce bioink. Subsequently, the skin is 3D bioprinted and either transplanted directly onto the wound surface or cultured under appropriate conditions to obtain mature skin for transplantation. Hennessy et al. showed that the structure and function of bilayer skin substitutes is more similar to natural human skin than single-layer skin substitutes [9].
Researchers produced complete skin model
Kim et al. were able to produce a complete skin model consisting of dermis and an epidermis stratified very similarly to human skin by using a combined extrusion and multi-jet 3D printer in 2017 [3]. For this purpose, they used material extrusion to construct a carrier structure of polycaprolactone and gelatin hydrogel and additionally imprinted it with collagen-embedded human primary dermal fibroblasts. These steps were repeated until the desired thickness of the structure was 3.5 mm. Multi-jet printing was used to apply a final layer of human epidermal keratinocytes. After two weeks of incubation of the artificial tissue, in addition to a stretching behavior of fibroblasts very similar to human skin, the expression of collagen and dermis-specific differentiation markers, among others, were shown to be indicative of a completely artificially produced and fundamentally functional skin tissue [4].
Literature:
- Marquardt Y, Huth S, Baron JM: Dermatologic research: potential applications of 3-D skin models. Dtsch Arztebl 2020; 117(24): [20]; DOI: 10.3238/PersDerma.2020.06.12.05
- Kocak E, Yildiz A, Acarturk F: Three dimensional bioprinting technology: Applications in pharmaceutical and biomedical area. Colloids Surf B Biointerfaces 2020; 197: 111396.
- Kim BS, et al: Direct 3D cell-printing of human skin with functional transwell system. Biofabrication 2017; 9(2):025034.
- “3D Printing Technologies for Soft and Hard Tissue Regeneration,” 03/16/2022, www.zwp-online.info/fachgebiete/oralchirurgie/grundlagen/3d-druck-techno…,(last accessed 12/07/2022).
- Xu J, et al: Polymers 2020; 12(6): 1237. www.mdpi.com/2073-4360/12/6/1237
- Augustine R: Skin bioprinting: A novel approach for creating artificial skin from synthetic and natural building blocks. Prog. Biomater 2018; 7: 77-92.
- Malik HH, et al: Three-dimensional printing in surgery: A review of current surgical applications. J Surg Res 2015; 199: 512-522.
- Gutierrez-Rivera A, et al: A protocol for enrichment of CD34+ stromal cell fraction through human skin disaggregation and magnetic separation. J Dermatol Sci 2010; 59: 60-62.
- Hennessy R, Markey MK, Tunnell JW: J Biomed Opt 2015; 20: 27001.
- “Research Landscape Switzerland. A Technological Panorama,” www.satw.ch/fileadmin/user_upload/SATW_Forschungslandschaft_Schweiz_SBFI…,(last accessed 07.12.2022).
DERMATOLOGY PRACTICE 2022; 32(6): 31











