Regular exercise testing of physical fitness should be routine in patients with chronic respiratory and pulmonary disease, as should pulmonary function testing. Reasons for exercise testing may include indications such as assessment of exercise capacity, evaluation of progression and treatment effects, or preoperative risk assessment, e.g., prior to lung resection or lung transplantation.
Regular exercise testing of physical fitness should be routine in patients with chronic respiratory and pulmonary disease, as should pulmonary function testing. The following indications can be used as a reason for a stress test:
- Assessment of physical resilience
- Indication of oxygen therapy for exercise-induced hypoxemia
- Assessment of progression and treatment effects, e.g. in COPD, cystic fibrosis, interstitial lung disease, pulmonary hypertension
- Preoperative risk assessment, e.g., prior to lung resection, lung volume reduction, lung transplantation.
- Occupational medical performance diagnostics and appraisal
- Sports medicine assessment, e.g. training control
- Analysis of training effects and other interventions in pneumological rehabilitation.
In patients with chronic respiratory and pulmonary disease, in addition to limitations in pulmonary function, other associated symptoms such as limitations in strength or cardiovascular function contribute to a significant reduction in exercise capacity. These limitations tend to be more pronounced the more advanced the disease stage. Numerous studies have demonstrated that impaired physical fitness is associated with poorer quality of life and also a poorer prognosis. In this respect, regular testing of patients’ physical resilience is an important assessment in order to identify conditional deficits in good time and to counteract them with the aid of a targeted physical training program.
The possibilities of performance diagnostics are manifold. The gold standard is certainly spiroergometry. However, load tests do not always have to be associated with this high metrological effort. Over time, a number of simple exercise tests have been established which do not require a large amount of equipment and yet provide valuable information on the physical exercise capacity of pneumological patients.
6-minute walk test (6-MWT)
Walking tests on level ground are possible in both children and the elderly and are also considered safe for patients with chronic lung disease. They are easy to perform and require minimal equipment, personnel and time. The significance of individual parameters (e.g. VO2max or heart rate) is comparable to that of (spiro-) ergometry [1]. The most commonly used walk test in the world is the 6-minute walk test (6MWT).
6-MWT Execution: Physical exertion must be avoided before the 6-MWT, i.e. the patient is brought to the 6-MWT in a wheelchair if necessary. After a 10-minute seated rest period, respiratory distress and muscular leg fatigue (using a 10-point Borg scale) are recorded in addition to oxygen saturation and pulse. In addition, aids used (e.g., rollator or oxygen device including O2 flow rate) should be accurately documented. Performing re-tests under altered baseline conditions (e.g., with/without a walker or with/without oxygen) can have a significant impact on the absolute 6-MWT distance. Therefore, the intra-individual framework should always be the same for the 6-MWT. In order to ensure valid comparability of the 6-MWT (especially with repeated measurements), a strictly standardized test procedure is also mandatory. These were published by the American Thoracic Society / European Respiratory Society (ATS/ERS) in a statement [2].

This includes that the test distance should be at least 30 m and bordered by two clearly visible turning marks. A course marker should be placed every 3-5 m (so that the meters covered in the last lap can be accurately recorded) (Fig. 1) .
The verbal information before and during the test is precisely defined [2]. Key points of instruction with the patient prior to the start of the test are as follows:
- the patient should walk as far as possible in 6 minutes
- it is a stress test that can/should lead to respiratory distress
- the patient is allowed to choose the walking pace, but can also vary it
- the patient receives a time announcement every minute for a better estimation of the remaining test duration
- if necessary, breaks may be taken (the test time nevertheless continues)
During the 6-MWT, the examiner should follow the patient/proband at a distance of approximately 1 meter without obstructing him/her, noting the lowest oxygen saturation measured using a pulse oximeter and the highest pulse rate that occurred during the 6-MWT [3].
At the end of the 6 minutes, the distance traveled will be documented using the floor markers (every 3-5 m) and the perceived dyspnea and muscular leg fatigue will be asked using the Borg scale. Official discontinuation criteria of the 6-MWT according to the ATS/ERS statement are: Chest pain, intolerable shortness of breath, leg cramps, unsteady gait, cold sweats, or sudden paling [2]. A drop in oxygen saturation below 80% during 6-MWT is discussed as a reason for discontinuation [2], but no negative correlation with the occurrence of adverse events has yet been shown in COPD patients [4].
6-MWT Interpretation: Although there is a wide variation in physical performance as measured by the 6-MWT between patients with comparable disease severity, there is an overriding tendency for patients with advanced lung disease to have a lower 6-MWT distance. For example, an analysis of 1795 COPD patients showed that COPD patients in GOLD stage II managed a median 6MWT distance of 409 ± 112 m, in GOLD stage III: 356 ± 120 m, and in GOLD stage IV only 291 ± 123 m [5].
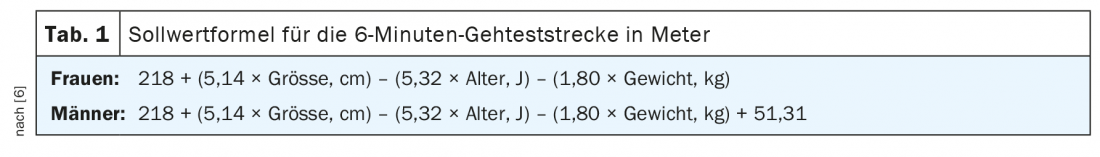
Normal values are used for inter-individual comparability of the walking performance. For the 6-MWT, the setpoint calculation listed in Table 1 has become established for German-speaking countries [6].
The domain of the 6-MWT is intra-individual comparison in the context of follow-up observations. It should be noted that when tests were repeated on the same or subsequent day, better results were obtained than on the initial test. As possible reasons for this learning effect, a better assessment of one’s own performance and less fear of stress are discussed [7]. For this reason, the ATS/ERS statement [2] recommends the performance of two 6-MWTs when precise evaluation of treatment effects or follow-up is required. If the 6-MWT is performed for a one-time assessment of disease severity or for prognosis estimation, a 6-MWT is sufficient [2]. From a recent meta-analysis by ATS/ERS, it appears that there is a significantly increased risk of mortality, especially from a 6-MWT distance of less than 300 to 350 m [7]. This threshold range was confirmed regardless of the type of lung disease.
The results of the 6-MWT generally correlate well with other severity assessment parameters in numerous pneumologic and cardiac conditions. The value of this exercise test is well documented, for example, in patients with chronic left heart failure, pulmonary hypertension, and interstitial lung disease. In addition, the 6-MWT has special significance for the multidimensional severity classification of COPD in the context of the BODE index.
The “minimally important difference” (MID) of a 6-MWT, i.e., the difference between two tests before and after an intervention that is associated with a change that is noticeable and clinically relevant to the patient, has been widely discussed. After several years of repeated shifts in the MID cutoff through different studies and in different populations, the ATS/ERS statement set the MID for all chronic lung diseases at a 6-MWT improvement of 30 m (95% CI 25-33 m) based on existing data [2]. It should be noted that MIDs are generally calculated for groups and, strictly speaking, may only be applied to cohorts. In this context, as with all MIDs, it is not excluded that the individual patient may feel a positive effect when his or her 6-MWT distance changes, e.g., significantly below or only above the MID of 30m.
Furthermore, in an analysis of 2112 COPD patients (ECLIPSE cohort), an annual decrease in 6-MWT distance of more than 30m was identified as a relevant cut-off value associated with a significantly increased mortality risk [8].
Shuttle Walk Tests
Although shuttle walk tests are widely used internationally for therapy monitoring in pneumological patients, these tests are still significantly underrepresented in German-speaking countries. Depending on the problem, they can be an interesting alternative to the 6-MWT. The procedure for the two test variants is briefly explained below.
Incremental shuttle walk test (ISWT): The ISWT is performed on a distance of 10 m (=1 shuttle), which is limited by 2 pylons. The walking speed is set by an acoustic signal (usually beeps from a CD player or an app). The patient’s task is to maintain the externally set walking speed and to be at the turning point at each beep. The walking speed increases every minute from an initial 1.8 km/h to a maximum of 8.5 km/h by shortening the interval between the beeps. The subjects are only allowed to walk, but not run. The test ends when the patient stops exertion due to dyspnea or exhaustion, or when the walking pace cannot be maintained (defined as failing to reach the turning point twice at the beep). The main result of the ISWT is the maximum distance covered in meters or the walking time in seconds. A positive response (MID) due to an intervention is assumed from an improvement of 47.5 m [9].
Endurance shuttle walk test (ESWT): following an ISWT, an ESWT can be performed after 30 minutes at the earliest, maintaining a constant walking speed of usually 85% of the maximum speed achieved during the ISWT [2]. The external control of the walking speed is also done via acoustic signals as described above. However, the intervals of the beeps remain the same here and no longer change. The primary test result is the length of time a subject can maintain the given speed. The test ends when the patient stops exertion due to dyspnea or exhaustion, or when the walking pace cannot be maintained (defined as failing to reach the turning point twice at the beep). For progress controls, the MID is assumed from an improvement of more than 65 seconds or 85 meters [2].
Compared to the 6-MWT or ISWT, the ESWT offers significantly higher sensitivity to map changes in exercise capacity (e.g., after an exercise program or administration of bronchodilators). This is a major advantage of ESWT that would more than justify its use in the context of pneumological interventions (such as pneumological rehabilitation).
Differences between the walking tests
Some aspects that may influence the selection of a walking test are discussed below. Walking tests can be applied broadly to determine a person’s physical capacity (maximal/functional capacity or endurance), factors limiting physical capacity (dyspnea, subjective fatigue, muscular limitations), and often change with intervention. Notably, the 6-MWT can also be used to predict survival probability and likelihood of hospital readmission based on thresholds. However, the 6-MWT can also be used as a basis for training control. For example, using the 6-MWT distance, the speed for treadmill training can be determined using the following formula: Walking distance (in m)/360 × 2.80 = training speed for gait training (in km/h).
Very practical considerations also include whether there is sufficient space available. If the test of choice is the 6-MWT, the test should be performed over a distance of at least 30 meters as recommended. If this space is not available, consider using the ISWT/ESWT (which requires only 10 meters). For both the 6-MWT and the ISWT, two tests are recommended for implementation to eliminate the learning effect. In this respect, the time required to perform both tests is comparable.
The 6-MWT and the Shuttle Walk Tests offer entirely different protocols: the 6-MWT is performed at a self-selected walking pace, while the speed of the Shuttle Tests is externally imposed. The load during the ISWT reflects the physiological response, comparable to that of a ramp/step test on a bicycle ergometer. There is a continuous increase in maximal oxygen uptake (VO2max) over time, while a stable plateau in oxygen uptake occurs after the third minute for the 6-MWT. The ESWT exhibits a significantly faster increase in VO2 and ventilation than the 6-MWT, with comparable VO2max values occurring at the end of these tests.
The sensitivity of the walk tests also varies widely. In COPD patients, the ESWT showed an approximately 50% greater increase after bronchodilator administration compared with the 6-MWT. Improvements in walking distance after pneumological rehabilitation were also significantly greater with ESWT, with a 92% increase, than with 6-MWT, with a 17% greater walking distance. These results suggest that the ESWT has a significantly higher sensitivity to map performance changes in functional endurance capacity.
When selecting a walking test, individual consideration must be given to which test is most appropriate given the different protocols, physiological response patterns, circumstances, and measurement characteristics of walking tests. Regardless of which test is chosen, – valid results can only be obtained if the test methodology/execution described above is carefully followed.
Sit-To-Stand Testing (STST)
To perform the test, the subject is asked to stand up from a chair and sit down again (with different objectives depending on the test form, as described in the course). The test begins and ends in a sitting position. The hands must not be used as support for standing up during this test. Therefore, they should be kept crossed in front of the chest. At the end of the stand-up movement, make sure that both the knees and the hips are completely extended for a short time. When sitting down, brief contact with the chair seat must be clearly visible. Before each stand-up test, there should be 1 to 2 repetitions for familiarization.
There are various designs for stand-up tests. In recent years, however, 2 forms have become particularly well established: the 5-repeat STST and the 1-minute STST. All that is needed for implementation is a chair with a standard seat height (usually 46-48 cm) and a stopwatch.
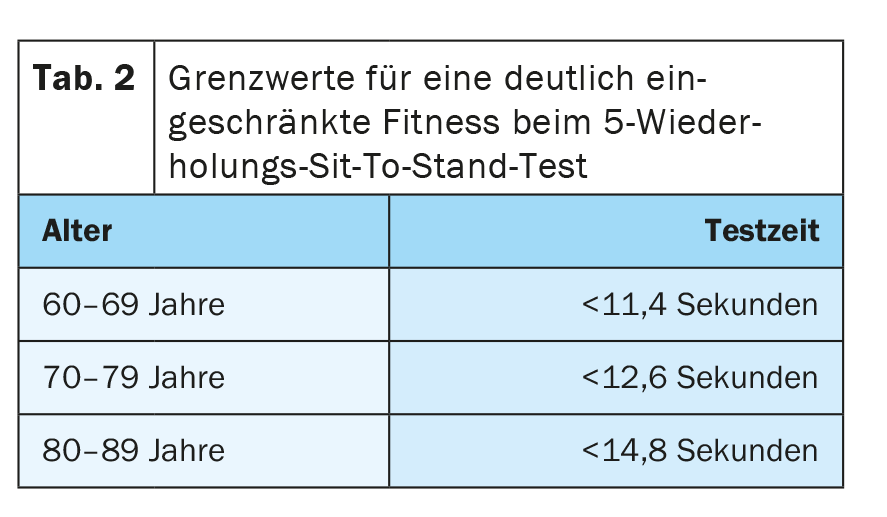
5-repetition STST: This test variant involves standing up and sitting down again as quickly as possible 5 times in succession according to the criteria mentioned. The time required for this is taken as the result. This primarily tests the strength capacity of the leg muscles as well as coordination (alternation between concentric and eccentric muscle work). In addition, this test provides an assessment of potential fall risk. If the required test time is above the thresholds listed in Table 2 , it is very likely that impaired physical performance and an increased risk of falling are present.
1-Minute STST: In this test, the subject has 1 minute to perform as many stand-up and sit-down movements as possible. The test person can choose his or her own pace and should estimate or adjust it so that the minute can be kept up if possible. Of course, breaks can also be taken if they are needed, for example, due to excessive shortness of breath. However, time continues to run during the breaks. The primary outcome of this test is the number of stand-up and sit-down movements completed in 1 minute. The 1-minute STST tests more strength-endurance ability and is much more strenuous compared to the 5-repetition stand-up test. Table 3 lists age- and sex-specific normal values (median values from a population of 7000 healthy subjects).
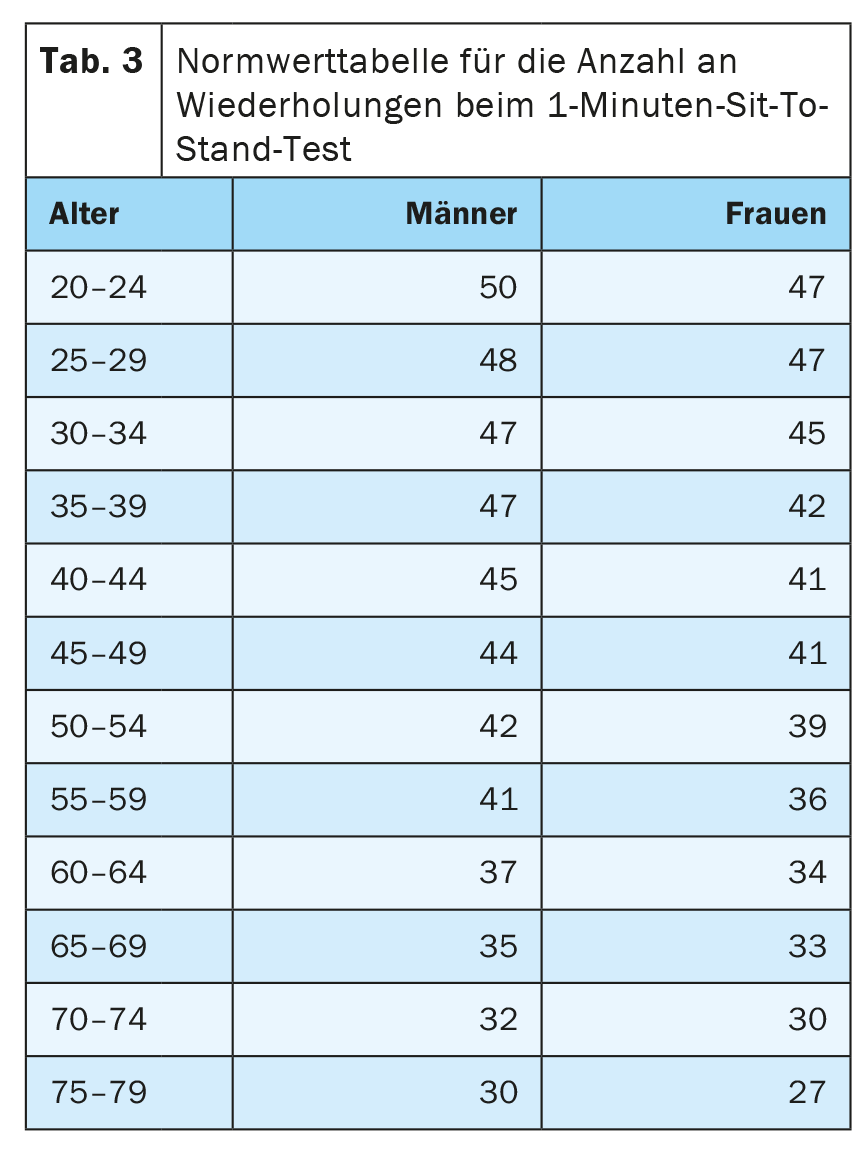
There are thresholds for the 1-minute STST developed specifically for COPD patients. Thus, patients who can do >20 repetitions in 1 minute have a significantly better probability of survival compared with patients who can do <11 repetitions [10].
Timed Up and Go Test (TUG)
The Timed Up and Go Test (TUG) is a mixture of the stand up and walk test. Here, the subject sits leaning on a chair with a backrest. On command, the subject is asked to stand up and walk straight at his normal everyday pace to a turning marker 3 meters away. Have the subject walk around this turnaround marker, walk the 3 meters back to the chair, and then sit back down. Any aids (e.g. walking stick or rollator) may be used for walking. The time required between the get-up command and the time at which the subject sits down again is noted. If the test is completed with a total duration of less than 10 seconds, full independent mobility is present. If the test takes more than 10 seconds to complete, a mobility impairment is present, which is associated with an increased risk of falling.
Take-Home Messages
- Functional exercise testing (such as walking tests or sit-to-stand tests) provides a simple way to obtain information about the exercise capacity of patients with chronic respiratory and pulmonary diseases.
- A strictly standardized test procedure is essential to obtain valid results.
- The 6-minute walk test is by far the most commonly used walk test, but shuttle walk tests are a valuable alternative.
- Sit-to-stand tests offer the advantage that they can be performed quickly without requiring much space or equipment and still provide a valid indication of patients’ physical capacity and prognosis.
Literature:
- Hill K, et al: Comparing peak and submaximal cardiorespiratory responses during field walking tests with incremental cycle ergometry in COPD. Respirology 2012; 17(2): 278-284.
- Holland AE, et al: An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. The European respiratory journal 2014; 44(6): 1428-1446.
- Chuang ML, Lin IF, Chen SP: Kinetics of changes in oxyhemoglobin saturation during walking and cycling tests in COPD. Respiratory care 2014; 59(3): 353-362.
- Roberts MM, et al: Oxygen desaturation and adverse events during 6-min walk testing in patients with COPD. Respirology 2015; 20(3): 419-425.
- Spruit MA, et al: Determinants of poor 6-min walking distance in patients with COPD: the ECLIPSE cohort. Respir Med 2010; 104(6): 849-857.
- Troosters T, Gosselink R, Decramer M: Six minute walking distance in healthy elderly subjects. Eur Respir J 1999; 14(2): 270-274.
- Singh SJ, et al: An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. The European respiratory journal 2014; 44(6): 1447-1478.
- Polkey MI, et al: Six-minute walk test in chronic obstructive pulmonary disease: minimally clinically important difference for death or hospitalization. Am J Respir Crit Care Med 2013; 187(4): 382-386.
- Singh SJ, et al: Minimum clinically important improvement for the incremental shuttle walking test. Thorax 2008; 63(9): 775-777.
- Puhan MA, et al: Simple functional performance tests and mortality in COPD. The European respiratory journal 2013; 42(4): 956-963.
InFo PNEUMOLOGY & ALLERGOLOGY 2022; 4(4): 8-12.