The implantation of knee and hip prostheses is one of the most frequently performed operations in Switzerland, with around 40,000 procedures per year. Despite the established methodology, studies show that up to 20% of patients are not satisfied with the achieved result after implantation of a total knee prosthesis. The revision risk for a knee prosthesis is about 6% within the first 5 years. Approximately 60% of these revisions occur due to surgical errors. Thus, there is a continuing need to improve surgical precision and minimize surgical errors.
The implantation of knee and hip prostheses is one of the most frequently performed operations in Switzerland, with around 40,000 procedures per year. Despite the established methodology, studies show that up to 20% of patients are not satisfied with the achieved result after implantation of a total knee prosthesis [1]. According to the Swiss Prosthesis Register, in which all knee and hip prosthesis implantations are compulsorily recorded, the revision risk for a knee prosthesis is approximately 6% within the first 5 years [2]. Looking critically at the reasons for these revisions, it can be formulated that approximately 60% of these revisions occur due to surgical errors. Malpositioning of prosthetic components and joint instabilities together account for a significant proportion of revisions. The affected patients often have a long period of suffering and there are significant costs for the health care system due to additional treatments, operations and possibly the inability to work. Thus, there is a continuing need to improve surgical precision and minimize surgical errors.
In a large proportion of the remaining dissatisfied patients, the knee prosthesis has been implanted correctly according to the currently valid technical aspects and the patient nevertheless reports limitations in knee function and resilience. In this context, a great deal of discussion has recently arisen in the literature regarding the correct objective for prosthesis positioning. Numerous authors proclaim a necessary individualization of therapy and prosthetic alignment based on the high variability of patient anatomy [3–5]. However, the established manual surgical methods aim at a standardized and systematic mechanical prosthesis alignment and a reproducible individualization is only possible to a limited extent here. Accordingly, many authors see the need for technical support for the surgeon to be able to implement new concepts in knee prosthetics and thus reduce the aforementioned high number of dissatisfied patients [6,7].
Previous developments of computer assistance in joint replacement surgery.
As early as the end of the 1990s, computer navigation was introduced to increase implantation accuracy and avoid incorrect positioning of knee and hip prostheses. Today’s established systems are based on passive, imageless navigation. During surgery, the surgeon scans specific anatomical landmarks with an infrared probe. A generic model joint from a stored database is then projected into these coordinates, which is available for angle measurement and sizing of the prosthesis. The surgeon gets real-time visualization of the alignment of his saw cut and implant on the computer screen during surgery. So he has a passive control of his actions.
According to current data, this technique is very well suited to increase implantation accuracy. In different meta-analyses it is presented that in almost all levels less deviations to the set alignment target are shown [8,9]. That this in turn already leads to a reduction in the revision rate is not so clearly proven. In large centers, this effect is certainly described [10], whereas in prosthesis registries it is only visible in special subgroup analyses of e.g. very young patients [11]. However, no effect can be demonstrated in terms of patient outcome and satisfaction [12]. One of the possible explanations of this data situation is the continued lack of individualization of therapy through the use of standard models, which can only represent the specific anatomical conditions to a limited extent. In Switzerland today, about 10% of knee prostheses are implanted with the support of navigation.
A next step in technical surgical support is represented by patient-specific saw-cut templates (PSI), which were first used in knee prosthetics around 2006 [13]. With this technology, MRI or CT imaging is performed prior to surgery and segmented to create a customized knee model of the patient. Individual surgery planning can then take place on the computer. To transfer this planning to the operating room, individual saw-cut templates are calculated and manufactured (3D printing), which can be positioned intraoperatively on the knee joint. You define the position of the prosthesis.
According to current data, a reduction of alignment outliers compared to manual implantation has also been described for this technique [14]. However, PSI is particularly interesting because of the possibility of individualizing the position of the prosthesis according to the patient’s anatomy. Some studies and meta-analyses show that improvements in patient outcome can be achieved with such personalized care [15,16]. However, there are also reports in the publications about an increased susceptibility to error of the templates and sometimes large deviations of the prosthesis position to the preoperative planning in individual patients [14,13]. There is also criticism that only anatomical image data can be used in computer planning and that dynamic parameters such as soft tissue tension are not addressed. These limitations, as well as the time-consuming planning, have not yet led to the technology becoming widespread. Currently, about 15% of knee prostheses are implanted with the help of PSI in Switzerland. Currently, PSI technology is being further developed with combination with augmented reality glasses to make computer planning visible intraoperatively and avoid alignment errors. However, there is currently no data on this, rather initial feasibility reports [17].
Robotic systems for joint replacement surgery
The first approaches to robot-assisted surgery in joint prosthetics date back to the late 1990s. The “RoboDoc” introduced at that time was a fully automated milling system that performed the preparation of the femur bone during the implantation of a hip prosthesis. Technologically, it was a little modified industrial robot that depended on the object – the bone – not moving during the milling process. It had to be fixed accordingly. This has caused numerous problems and also specific complications, so the technology has been completely abandoned in Europe (even after much negative PR).
Since that time, robotic technologies have advanced immensely. As an example, modern systems can now react to external influences – e.g. the surgeon – and dynamically adjust their operation plan in three dimensions in space in real time. The bone can therefore now move during the milling or sawing process and the robotic tool is no longer necessarily guided autonomously by the robot, but can be guided by the surgeon (so-called haptic technology). The robot therefore rather supports the surgeon by checking the correct sawing plane and, if necessary, braking the surgeon if he were to leave the surgical plan. In contrast to the computer navigation discussed, this is now an active tool that not only provides data on prosthesis alignment, but also more or less actively supports the implementation of the surgical plan.
What specifically constitutes a surgical robot is not further defined, except for the characteristic of actively supporting one or more work steps. To date, four assistance systems for joint prosthetics have been approved in Switzerland, which describe themselves as “robotic surgical assistance” (Tab. 1) . However, they differ significantly in their technological details, handling and possibilities. Accordingly, it is critical to consider robotic-assisted surgery as something uniform, also in terms of clinical data, their benefits and added value! In the following, we will first briefly discuss the main differences between the technologies in order to be able to assess this in the discussion of the evidence, because not all robots are the same.

MAKO technology
The so-called MAKO technology has already been in clinical use since 2006, initially isolated for partial knee prosthetics [18]. Later, applications for total hip prostheses were added, and most recently total knee prosthesis in 2016. This makes it currently the only system that can be used to cover the entire range of the knee and hip and for which clinical experience of more than 10 years exists. In 2018, the first 2 of these MAKO systems were put into operation in Switzerland at Hirslanden Bern, and to date over 1000 procedures have already been performed with them. In the meantime, there are 2 more machines in Switzerland.
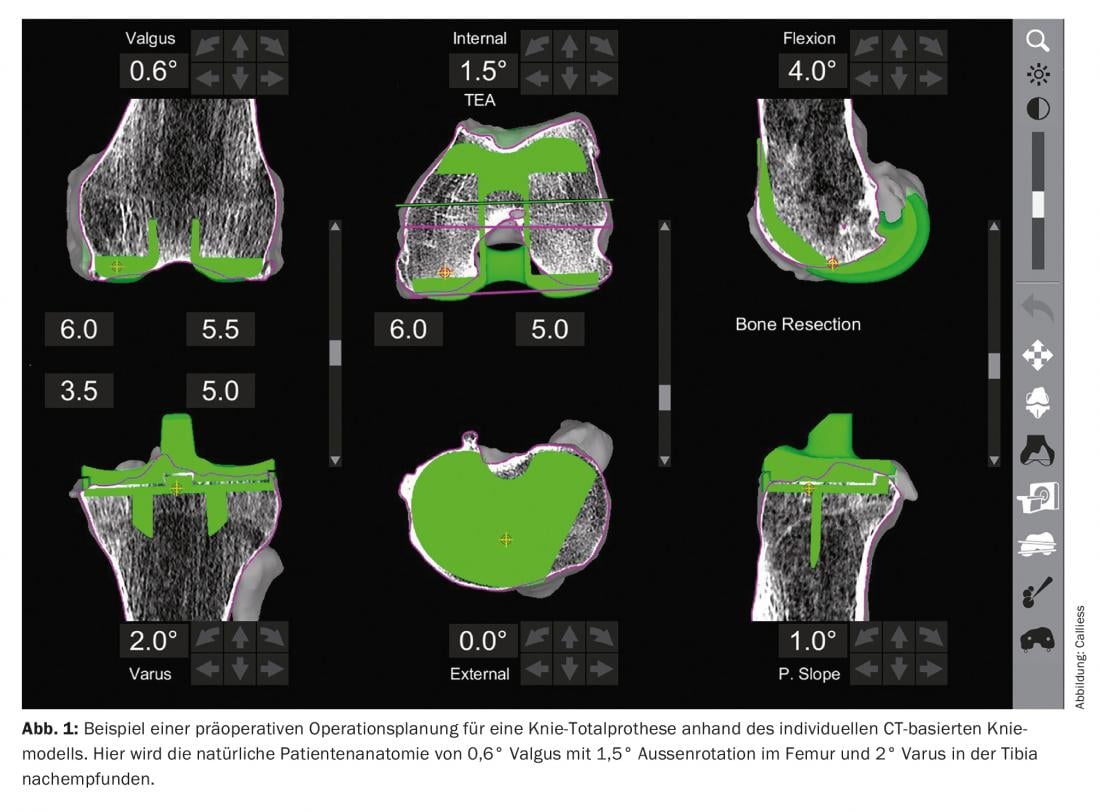
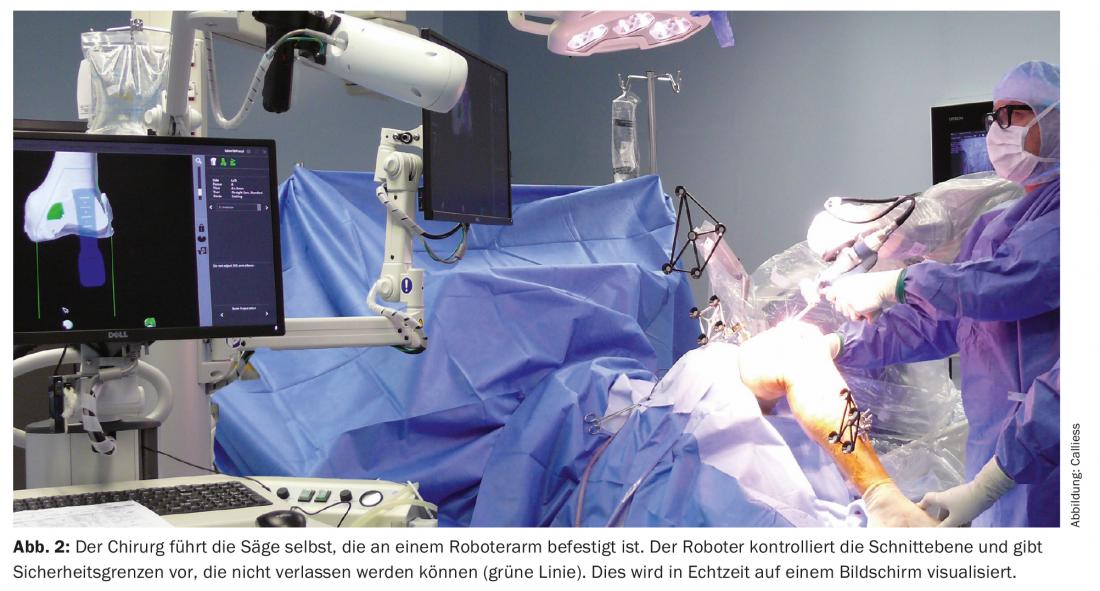
What is special about this technology is that it is based on image data of the patient (similar to PSI technology). Preoperatively, a CT of the hip, knee, and ankle is taken and segmented to create an individual bone model. Based on this, the surgeon is able to create an operation plan individualized to the patient already preoperatively (Fig. 1) . This is checked and fine-tuned intraoperatively on the basis of dynamic parameters – the ligament tension, the motion profile of the knee joint. After virtual determination of the specific prosthesis alignment based on this information, the corresponding saw cuts, or milling of the implant bed, are then performed with the support of the haptic robot arm. The working tool is guided by the surgeon, and the robot maintains the correct plane or sets limits for the activation of the tool by braking or stopping the working tool (Fig. 2). Thus, the surgeon cannot leave the plan and the surrounding soft tissues are actively protected. Image-guided planning can visualize osteophytes and also objectively verify the final prosthesis position such as ligament stability. Compared to PSI, therefore, additional parameters can be taken into account and the robot support can reduce so-called alignment outliers.
NAVIO/CORI
The second robotic system goes by the name of NAVIO or CORI in the 2nd generation [19]. It has been available on the European market since around 2015. Again, applications for partial and total knee prosthetics are available, while hip applications are still under development. There are currently no CORI machines in use in Switzerland.
Technologically, in contrast to the MAKO, this is a so-called imageless, model-based system. Analogous to the computer navigation discussed, bone coordinates are determined intraoperatively, which are used to create a generic bone model. What is special then is that in addition to this model, the surgeon can also tap the actual bone surface intraoperatively with a probe. This creates a pseudo-CT on the screen that is available for individualized planning. Dynamic motion and stability parameters can also be recorded here, which can be incorporated into virtual surgery planning and prosthesis alignment. The robotic part consists of a navigated handpiece with milling head. The denture bed is milled with this. The milling head retracts as soon as the defined milling area is left. Alternatively, positioning holes can be made with the milling machine, into which conventional saw-cut blocks are then inserted. In this case, the surgeon applies a conventional hand-guided saw through the positioned cutting block without this being robotically guided.
OMNIBOT
The OMNIBot system is a navigation platform augmented with a passive robotic unit [20]. The first clinical application was carried out in 2007, and some devices have been in use in Switzerland since 2019. Currently, only one application is available for total knee prostheses.
The OmniBot system is based exclusively on the described principles of model-based computer navigation. The tibial saw cut is performed in the conventional way (without robotic assistance). What is special then is that, unlike the other systems, a pressure-controlled ligament tensioner is introduced, which, unlike the surgeon’s subjective determination of ligamentary stability, determines it according to objective parameters. A stability curve is recorded over the entire radius of motion. This data is then used to plan the virtual alignment of the prosthesis until optimal ligament tension is achieved with the prosthesis. Currently, assistance is being developed by the system for the surgeon for this purpose. Making the saw cuts on the femur is assisted by a small robotic unit on the femur bone that adjusts a conventional saw cut template to the correct plane. The surgeon therefore uses his usual hand saw in the same way as in the system described above. The focus of this system is therefore less on the correct reproduction of the bone anatomy than primarily on optimized ligament tension.
ROSA
The youngest representative of robot-assisted joint surgery is the ROSA system [21], in use in some clinics in Switzerland since 2021. This can also currently only be used for total knee prosthetics; partial prosthetics are currently limited to selected development centers.
Technologically, ROSA, like the previous two, is an imageless, model-based navigation system. However, there is the possibility to pre-select the generic knee model preoperatively on the basis of standardized radiographs, which allows for a pre-planning of the prosthesis position preoperatively and should also reduce the error rate when recording the intraoperative coordinate system.
Analogous to the systems described above, it is possible to read in the ligament stability intraoperatively and incorporate it into the virtual surgical planning. When performing the operation, a saw-cutting template is then used, which is positioned in the correct plane by means of a robotic arm. The saw cut itself is made manually with a conventional saw as described above.
Other systems are currently under development, each with specific peculiarities. However, they do not yet have marketing authorization for Switzerland. Overall, robotics in Switzerland is still at an early stage. In 2021, less than 3% of primary knee replacements were implanted using the aforementioned robotic systems [2].
Current Evidence Base
Increase precision and accuracy
Corresponding to the different lengths of clinical availability of the systems described, the evidence base is very heterogeneous. Common to all systems is the goal of increasing surgical precision and avoiding implant misplacements. This is easy to verify methodologically using radiological outcome analyses. Unsurprisingly, there are corresponding positive reports for all of the technologies mentioned that this primary goal certainly seems to have been achieved [19,20,22,23]. High precision in achieving the desired prosthesis position and reduced deviations (outliers) in the leg axis position compared to manual implantation have been proven. Clear differences between the systems and technologies have not yet been described.
In our own comparative work, we once investigated the precision for correct sizing of the prosthesis between conventional, manual implantation, the image-guided MAKO system and the imageless NAVIO system for partial denture prosthetics [24]. Both robot-assisted methods are shown to be superior to the manual technique in clinically relevant parameters. A direct comparison of the technologies shows a benefit for the CT-based MAKO technique. Thus, there seems to be an advantage in planning due to the preoperatively visible bone anatomy; intraoperatively difficult to see regions are clearly visualized and a distinction between native bone and formed osteophytes is possible. In addition, the source of error “surgeon” in the acquisition of the coordinate system is reduced.
Reduction of complications and revisions
Based on the positive evidence for increased surgical precision and error prevention, the question arises again whether this also (automatically) leads to a reduction in the revision rate and complications?
Two recent meta-analyses were published last year on this aspect of complication rates, which initially found no difference in robotic-assisted knee replacements compared with the manual standard [25,26]. However, it is important to note that literature from 2007-2019, or 2019-2020, was included – i.e., fairly early publications on each technology relative to clinical experience, potentially including the learning curve. Furthermore, the literature invariably considers the early revision rate (usually first 90 days!), which is often not primarily related to technical errors in prosthesis positioning – i.e. infections, wound healing disorders or fractures.
If one looks at the parameter revision rate for robot-assisted knee prostheses compared to manual implantations, the Australian Prosthesis Registry is particularly interesting to consider [11]. In Australia, there is very detailed recording of the surgical technique used (unlike most other registries) and a good 70% of knee replacement implantations there are done using computer and robotic technology. Robot-assisted methodology has already accounted for 16.6% of total knee replacements in 2021 and as much as 30% of partial replacements.
In the registry data from 2021, there is a minimal advantage for robotics in total knee arthroplasty for the 3-year revision rate recorded to date, but currently without clear statistical significance. Here, the longer follow-up remains to be seen.
In partial knee arthroplasty – usually an operation in which the precision of prosthesis positioning plays a greater role and is more prone to error – an interesting picture emerges: The annual report of the Prosthesis Registry from 2019 showed a highly significant advantage of the robot-assisted partial knee prosthesis over the manual standard after 3 years. At the time, it was almost exclusively the MAKO system that was represented in these data, and large, specialized centers that were the first to adopt the technique. In the current report from 2021, this effect of the reduced complication rate is no longer significant. One possible explanation for this is the now very different technologies that are summarized here under the term “robot-assisted” and also the numerous new users, who possibly influence the data with their learning curve. As before, the partial prosthesis used in conjunction with MAKO technology is the one with the lowest revision rate in the Australian Registry. Similarly, only the MAKO partial prosthesis can be uniquely identified in SIRIS [2]. Again, this shows a significantly lower 2-year revision rate than average: 1.8% vs. 4.6%. If we look again at data from meta-analyses and large centers specifically for partial knee prostheses, we also find a statistically significant difference in the revision rate Pro Robotic Technology [27,28].
Learning curve and costs
As just mentioned, it is quite conceivable that the learning curve of the operator has an influence on the parameters discussed. Currently, the literature mainly evaluates the learning curve in relation to the operation time. Here it is shown that an efficient work with the robot is learned quickly and already after a few cases (7-20 depending on the author) a reproducible and only slightly prolonged operation time is achieved [26,29]. Some work can even demonstrate that as it progresses, a further reduction in surgical time is possible until it is neutral to the pre-robotic workflow after about 100 cases. However, this requires a high number of cases and high percentage adaptation of the technology.
In terms of surgical precision – making accurate saw cuts – there does not appear to be a significant learning curve [30]. We were able to prove ourselves in a study that even a surgeon with little experience can realize a high implantation accuracy thanks to the robotic technique [31]. However, the complication rate was still elevated in these inexperienced operators compared with the data presented for the robot-experienced specialty centers.
This brings me to a key learning curve discussion point that is underrepresented in the literature: proper intraoperative decision making. Robotic assistance clearly helps the surgeon in the improved execution of a surgical plan, but not in the creation and fine-tuning of that plan (at least according to the current state of the art). It provides a lot of additional data and information about the joint and dynamic parameters that must be recorded and interpreted by the surgeon. Errors can also occur and the prosthesis may not be optimally positioned during the planning stage. In this respect, a high level of experience with the systems is required, as well as permanent learning based on the available parameters to improve and further develop the decision algorithms. This circumstance represents a certain hurdle for many operators in adapting to the new technology. Thus, a high level of specialization and caseload with robotics appears essential despite active technology support.
A second factor in this context relates to the additional costs of the technologies, which are not reflected in the current remuneration system and make the widespread use of robotics difficult. According to a separate study, the additional cost is approximately 1600-2500 CHF per procedure, depending on the technology used (imageless vs. CT-assisted) [32]. There is a partial dependence on the number of cases and also on the efficiency of workflows of the surgeon and the surgical department. Here, pure intraoperative planning and setting seems to be more time-consuming than a preoperative planning option.
Patient Outcome
Last but not least, one of the critical factors for evaluating the added value of robotics in joint interventions remains the improvement of patient outcome and satisfaction. This is the only way to ultimately justify the additional costs, if the effect of reducing costs by reducing revision operations is currently rather small.
There are already some quite good, reliable data on partial knee prosthetics in this regard. Canetti and co-authors describe a more rapid return to sports ability after robotic-assisted partial prosthesis [33]. The research group led by Marc Blyth was able to show in a prospective, randomized, double-blind study that the robotic knee joints showed a faster average rehabilitation and less postoperative pain than the conventionally operated comparison group [34]. However, 1 year postoperatively, no significant difference was detectable. This effect has been described in other studies. In interpretation, the reduced postoperative pain is probably due to the more soft-tissue-sparing surgical technique, which is especially true for the robotic-controlled burrs (MAKO, NAVIO).
The data situation for total knee prostheses is also quite positive. In a recently published meta-analysis, a significant benefit for knee function and Patient Reported Outcome is shown with regard to robotic-assisted total knee replacement – Evidence level: good [26]. Analogous to the experiences described with PSI, the studies that stand out in particular are those that use the possibility of three-dimensional virtual planning in such a way that the prosthesis is implanted individualized for the patient. Several authors clarify that the outcome is significantly best when the prearthrotic anatomy can be reconstructed with the prosthesis [35-37]. Following the same mechanically oriented concepts as those derived from manual technique does not improve patient outcome.
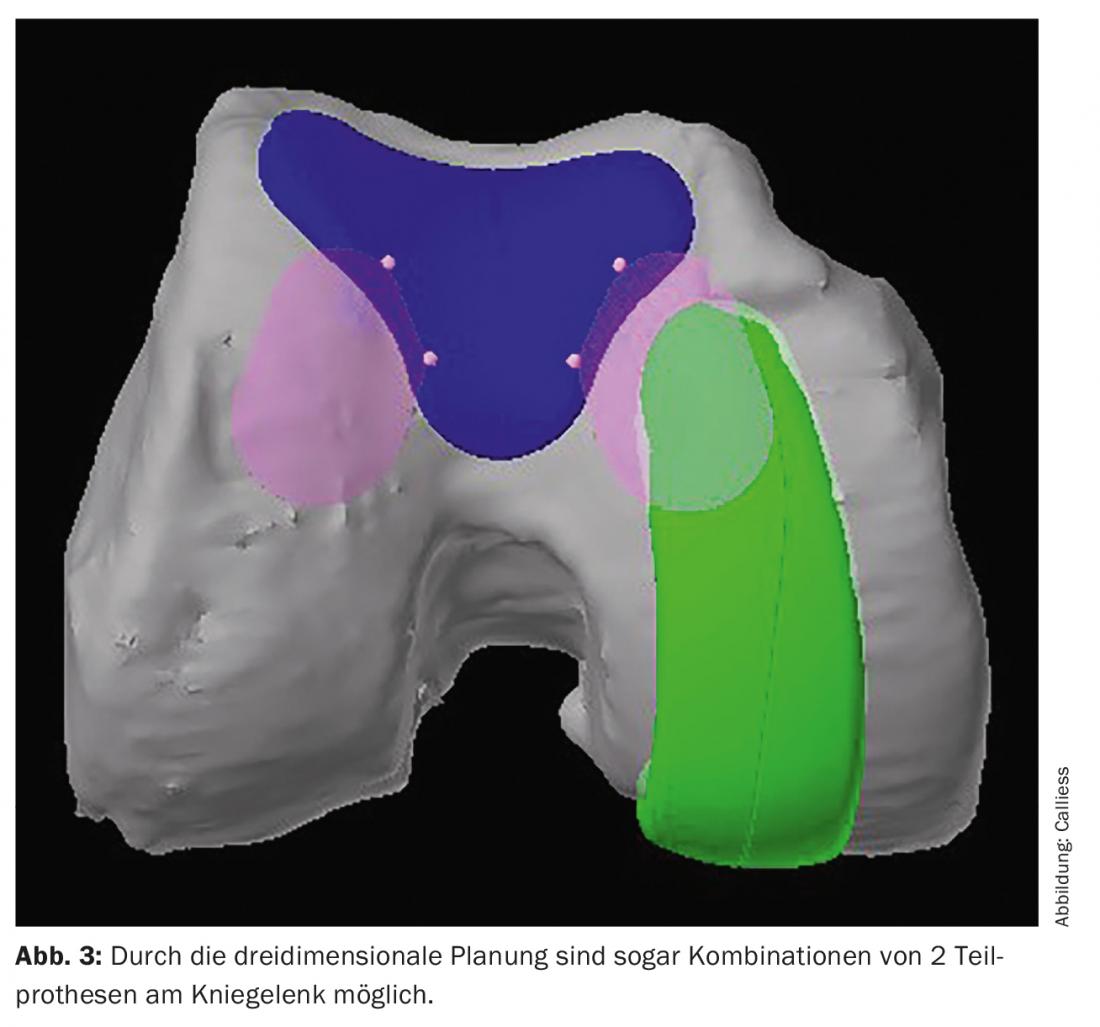
Another interesting aspect for improving patient outcome is the more frequent use of partial prosthetic solutions instead of total prosthesis with the help of robotics. Or the combination of two partial prostheses with preservation of the cruciate ligaments instead of a total prosthesis resecting the cruciate ligaments (Fig. 3). As shown, a major counter-argument of the partial prosthesis – the increased revision rate – seems to be well addressed by robotic support. Since the partial denture is superior to the total denture in terms of patient outcome when indicated correctly, increasing the proportion of partial dentures is already an improvement in patient outcome. For example, we now perform about 45% of our knee prosthesis implantations as partial prostheses, contrary to the Swiss average of currently about 17% [2].
Added value or marketing?
So if we now briefly return to the somewhat publicistically formulated initial question, it can be summarized that in the area of partial knee prostheses, a real added value has been demonstrated by robotic support. Although the patient outcome of a robot-assisted partial prosthesis in the medium term is not necessarily better than a conventionally operated one, rehabilitation is shortened and the risk of revision is significantly reduced. If more partial prostheses are implanted instead of total prostheses as a result of the use of robots, the health care system will also benefit in macroeconomic terms: partial prostheses have comparatively fewer complications, a higher quality of life and lower treatment costs overall. The additional costs resulting from the use of robots are offset by these effects.
For total knee prostheses, the scientifically confirmed added value in terms of rehabilitation and revision risk is even less clearly demonstrated. However, robotics demonstrates the added value of being able to better take into account the natural patient anatomy and to individualize therapy based on objective decision parameters. This has been shown to have the potential to improve quality of care and outcomes. However, if the same surgical principles of conventional knee arthroplasty are used, the added value is low.
Take-Home Messages
- In Switzerland, currently only about 3% of knee prostheses with robotic support.
- Image-guided robotic assistance results in a significant reduction in revision rate for knee hemiprostheses (1.8% vs. 4.6% at 2 years).
- For total knee prostheses, individualized prosthesis fitting/alignment with high precision is made possible. This improves patient outcome.
- Current disadvantages: high operating costs and learning curve for the individual operator.
Literature:
- Rodriguez-Merchan EC: Patient Satisfaction Following Primary Total Knee Arthroplasty: Contributing Factors. Arch Bone Jt Surg 2021; 9 (4): 379-386; doi: 10.22038/abjs.2020.46395.2274.
- Annual Report of the Swiss National Joint Registry, Hip and Knee 2012-2021. https://swiss-medtech.ch/news/siris-report-2021
- Beckmann J, Meier MK, Benignus C, et al: Contemporary knee arthroplasty: one fits all or time for diversity? Arch Orthop Trauma Surg 2021; 141 (12): 2185-2194; doi: 10.1007/s00402-021-04042-4.
- Riviere C, Lazic S, Boughton O, et al: Current concepts for aligning knee implants: patient-specific or systematic? EFORT Open Rev 2018; 3 (1): 1-6; doi: 10.1302/2058-5241.3.170021.
- Riviere C, Iranpour F, Auvinet E, et al: Alignment options for total knee arthroplasty: A systematic review. Orthop Traumatol Surg Res 2017; 103 (7): 1047-1056; doi: 10.1016/j.otsr.2017.07.010.
- Ettinger M, Tucking LR, Savov P: [Kinematic alignment in total knee arthroplasty with image-based and image-independent robotic support]. Orthopaedics 2020; 49(7): 604-610; doi: 10.1007/s00132-020-03924-6.
- Urish KL, Conditt M, Roche M, Rubash HE: Robotic Total Knee Arthroplasty: Surgical Assistant for a Customized Normal Kinematic Knee. Orthopedics 2016; 39(5): e822-827; doi: 10.3928/01477447-20160623-13.
- Cheng T, Zhao S, Peng X, Zhang X: Does computer-assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized controlled trials? Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA 2012; 20(7): 1307-1322; doi: 10.1007/s00167-011-1588-8.
- Fu Y, Wang M, Liu Y, Fu Q: Alignment outcomes in navigated total knee arthroplasty: a meta-analysis. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA 2012; 20 (6): 1075-1082; doi: 10.1007/s00167-011-1695–1696.
- Baier C, Wolfsteiner J, Otto F, et al: Clinical, radiological and survivorship results after ten years comparing navigated and conventional total knee arthroplasty: a matched-pair analysis. International orthopaedics 2017; 41(10): 2037-2044; doi: 10.1007/s00264-017-3509-z.
- Australian Orthopaedic Association National Joint Replacement Registry Annual Report 2021. https://aoanjrr.sahmri.com/annual-reports-2021.
- Lee DY, Park YJ, Hwang SC, et al: No differences in mid- to long-term outcomes of computer-assisted navigation versus conventional total knee arthroplasty. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA 2020; 28(10): 3183-3192; doi: 10.1007/s00167-019-05808-5.
- Calliess T, Ettinger M, Stukenborg-Colsmann C, Windhagen H: [Custom-fit kinematic alignment in total knee arthroplasty using PSI. The story of ShapeMatch technology]. The Orthopaedic Surgeon 2016; 45 (4): 314-321; doi: 10.1007/s00132-016-3240-2.
- Thienpont E, Schwab PE, Fennema P: Efficacy of Patient-Specific Instruments in Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. The Journal of bone and joint surgery American 2017; 99 (6): 521-530; doi: 10.2106/JBJS.16.00496.
- Woon JTK, Zeng ISL, Calliess T, et al: Outcome of kinematic alignment using patient-specific instrumentation versus mechanical alignment in TKA: a meta-analysis and subgroup analysis of randomised trials. Arch Orthop Trauma Surg 2018; 138(9): 1293-1303; doi: 10.1007/s00402-018-2988-8.
- Calliess T, Bauer K, Stukenborg-Colsman C, et al: PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 2017; 25(6): 1743-1748; doi: 10.1007/s00167-016-4136-8.
- Fucentese SF, Koch PP: A novel augmented reality-based surgical guidance system for total knee arthroplasty. Arch Orthop Trauma Surg 2021; 141(12): 2227-2233; doi: 10.1007/s00402-021-04204-4.
- Roche M: The MAKO robotic-arm knee arthroplasty system. Arch Orthop Trauma Surg 2021; 141(12): 2043-2047; doi: 10.1007/s00402-021-04208-0.
- Sicat CS, Chow JC, Kaper B, et al: Component placement accuracy in two generations of handheld robotics-assisted knee arthroplasty. Arch Orthop Trauma Surg 2021; 141(12): 2059-2067; doi: 10.1007/s00402-021-04040-6.
- Shatrov J, Murphy GT, Duong J, Fritsch B: Robotic-assisted total knee arthroplasty with the OMNIBot platform: a review of the principles of use and outcomes. Arch Orthop Trauma Surg 2021; 141(12): 2087-2096; doi: 10.1007/s00402-021-04173-8.
- Batailler C, Hannouche D, Benazzo F, Parratte S: Concepts and techniques of a new robotically assisted technique for total knee arthroplasty: the ROSA knee system. Arch Orthop Trauma Surg 2021; 141(12): 2049-2058; doi: 10.1007/s00402-021-04048-y.
- Parratte S, Price AJ, Jeys LM, et al: Accuracy of a New Robotically Assisted Technique for Total Knee Arthroplasty: A Cadaveric Study. J Arthroplasty 2019; 34(11): 2799-2803; doi: 10.1016/j.arth.2019.06.040.
- Batailler C, Fernandez A, Swan J, et al: MAKO CT-based robotic arm-assisted system is a reliable procedure for total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 2021; 29(11): 3585-3598; doi: 10.1007/s00167-020-06283-z.
- Batailler C, Bordes M, Lording T, et al: Improved sizing with image-based robotic-assisted system compared to image-free and conventional techniques in medial unicompartmental knee arthroplasty. Bone Joint J 2021; 103-B(4): 610-618; doi: 10.1302/0301-620X.103B4.BJJ-2020-1453.R1.
- Chin BZ, Tan SSH, Chua KCX, et al: Robot-Assisted versus Conventional Total and Unicompartmental Knee Arthroplasty: A Meta-analysis of Radiological and Functional Outcomes. J Knee Surg 2021; 34(10): 1064-1075; doi: 10.1055/s-0040-1701440.
- Zhang J, Ndou WS, Ng N, et al: Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2021; doi: 10.1007/s00167-021-06464-4.
- Batailler C, White N, Ranaldi FM, et al: Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2019; 27(4): 1232-1240; doi: 10.1007/s00167-018-5081-5.
- Sun Y, Liu W, Hou J, et al: Does robotic-assisted unicompartmental knee arthroplasty have lower complication and revision rates than the conventional procedure? A systematic review and meta-analysis. BMJ Open 2021; 11(8): e044778; doi: 10.1136/bmjopen-2020-044778.
- Chen Z, Bhowmik-Stoker M, Palmer M, et al: Time-Based Learning Curve for Robotic-Assisted Total Knee Arthroplasty: A Multicenter Study. J Knee Surg 2022; doi: 10.1055/s-0042-1744193.
- Vermue H, Luyckx T, Winnock de Grave P, et al: Robot-assisted total knee arthroplasty is associated with a learning curve for surgical time but not for component alignment, limb alignment and gap balancing. Knee Surg Sports Traumatol Arthrosc 2022; 30(2): 593-602; doi: 10.1007/s00167-020-06341-6.
- Savov P, Tuecking LR, Windhagen H et al: Robotics improves alignment accuracy and reduces early revision rates for UKA in the hands of low-volume UKA surgeons. Arch Orthop Trauma Surg 2021; 141(12): 2139-2146; doi: 10.1007/s00402-021-04114-5.
- Christen B, Tanner L, Ettinger M, et al: Comparative Cost Analysis of Four Different Computer-Assisted Technologies to Implant a Total Knee Arthroplasty over Conventional Instrumentation. J Pers Med 2022; 12(2); doi: 10.3390/jpm12020184.
- Canetti R, Batailler C, Bankhead C, et al: Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg 2018; 138 (12): 1765-1771; doi: 10.1007/s00402-018-3042-6.
- Gilmour A, MacLean AD, Rowe PJ, et al: Robotic-Arm-Assisted vs Conventional Unicompartmental Knee Arthroplasty. The 2-Year Clinical Outcomes of a Randomized Controlled Trial. J Arthroplasty 2018; 33 (7S): S109-S115; doi: 10.1016/j.arth.2018.02.050.
- Huber K, Christen B, Calliess S, Calliess T: True Kinematic Alignment Is Applicable in 44% of Patients Applying Restrictive Indication Criteria-A Retrospective Analysis of 111 TKA Using Robotic Assistance. J Pers Med 2021; 11 (7); doi: 10.3390/jpm11070662.
- Winnock de Grave P, Luyckx T, Claeys K, et al: Higher satisfaction after total knee arthroplasty using restricted inverse kinematic alignment compared to adjusted mechanical alignment. Knee Surg Sports Traumatol Arthrosc 2022; 30 (2): 488-499; doi: 10.1007/s00167-020-06165-4.
- Elbuluk AM, Jerabek SA, Suhardi VJ, et al: Head-to-Head Comparison of Kinematic Alignment Versus Mechanical Alignment for Total Knee Arthroplasty. J Arthroplasty 2022; doi: 10.1016/j.arth.2022.01.052.
HAUSARZT PRAXIS 2022; 18(4): 6-13











