Strengthening the body’s defenses with the help of orally ingested bacterial extracts can help fight respiratory infections in humans. In a recently published study, the underlying mechanisms of action of this immunological benefit were analyzed using murine coronavirus (MCoV) in a mouse model.
That ingestion of the bacterial lysate OM-85-BV (Broncho-Vaxom®) in humans results in both a significantly lower incidence of recurrent respiratory infections and a lower overall duration of respiratory infections has been demonstrated in previous studies [1–3]. To investigate what cellular and molecular mechanisms are involved, treatment effects of OM-85-BV on murine coronavirus (MCoV) A59 im were analyzed. In this regard, treatment with OM-85-BV was shown to result in a reduction in viral load, an accumulation of interstitial macrophages in lung tissue, and an associated more rapid response of interferon type-I signaling [4].
Massive viral reduction on day 4 and 10
74 laboratory mice were divided into treatment and control groups in a 1:1 ratio. Experimental animals in the verum condition received 7.2 mg orally administered OM-85-BV (dissolved in 200 μL 3% D-mannitol) for a period of 10 days [4]. Mice in the control condition received 200 μL 3% D-mannitol. Tissue samples were analyzed at 2, 4, and 10 days after intranasal MCoV infection, respectively, by quantitative PCR (qPCR), RNA sequencing, histology, and flow cytometry. To measure viral load, quantitative PCR (qPCR) was used to determine the two viral markers Nsp12 and PolyU in the lungs. This showed that mice with an immune system trained by the bacterial lysate had a massive viral reduction on day 4 that persisted on day 10.
Lung-specific accumulation of interstitial macrophages.
Macrophages represent the first line of defense until specific B and T cells fight off the infection. The homeostatic population of lung macrophages includes interstitial macrophages derived from circulating monocytes in addition to alveolar macrophages of embryonic origin [5,6]. Alveolar macrophages were not altered with treatment and were gradually reduced during infection as expected. However, an increase in interstitial macrophages was observed after OM-85-BV treatment and before viral infection [4]. In the verum group, the accumulation of interstitial macrophages in lung tissue after MCoV infection resulted in a more rapid response of interferon type-I signaling. Moreover, RNA sequencing showed that lung tissue from the experimental animals receiving OM-85-BV at day 4 resembled an intermediate stage between healthy and virally infected lung tissue, suggesting a more rapid return to normal tissue homeostasis. To determine whether the modulation of the lung immune system is organ-specific, the researchers analyzed monocytes and splenic macrophages before and during MCoV infection. Regardless of the OM-85-BV treatment, there were no differences in the amount of monocytes in the bloodstream or macrophages in the spleen, neither at baseline nor during MCoV infection. This indicates lung-specific accumulation of interstitial macrophages induced by OM-85-BV pretreatment.
Improved viral clearance and reduced apoptotic load on the lungs
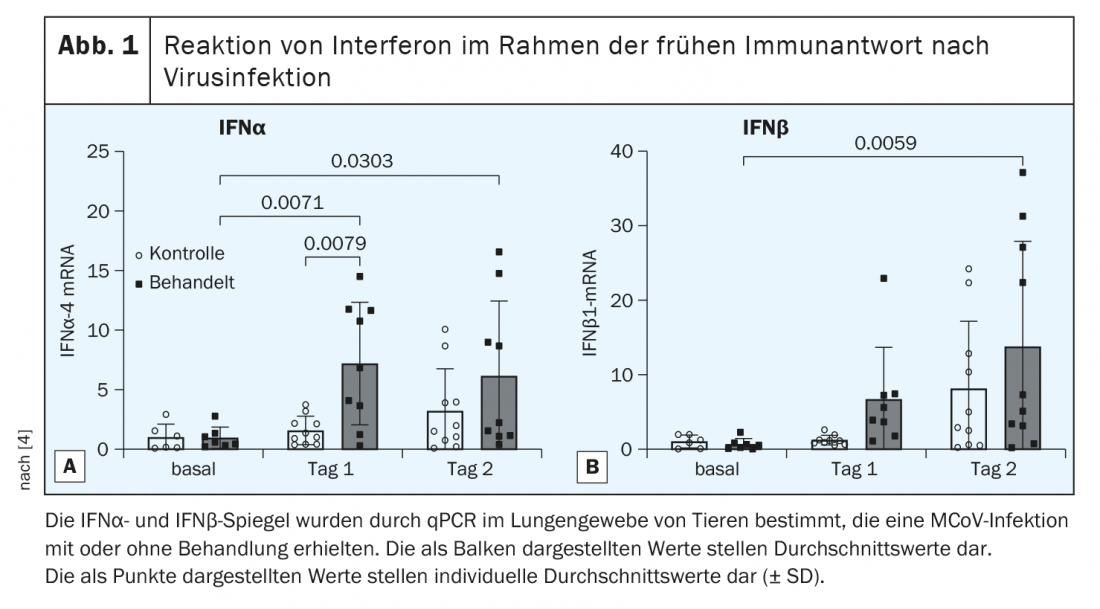
Viral infections are accompanied by host cell apoptosis [7]. Treated animals showed reduced apoptotic load on lung tissue at days 4 and 10 compared with the control group. Furthermore, the data suggest that pretreatment with OM-85-BV improved the initial response to viral infection and resulted in more rapid clearance of MCoV, probably by inducing type I interferon (IFN). Therefore, baseline and IFN pathway activation levels were measured at days 1 and 2 postinfection. Treatment with OM-85-BV did not increase baseline IFNα levels, but there was a strong and significant induction of IFNα at day 1 in OM-85-BV treated animals (Fig. 1A) [4]. IFNβ was significantly induced in treated animals at day 2 (Fig. 1B) [4]. Overall, the results indicate a strong upregulation of type I IFN response Tag. 1 after treatment with OM-85-BV. At the cellular level, flow cytometric measurement showed that on day. 1 in OM-85-BV-treated animals, particularly CD45+CD64+ macrophages and CD45 non-leukocytes had significantly more interferon-regulatory factor 1 protein than did laboratory mice in the control group.
Literature:
- Drug Information, www.swissmedicinfo.ch (last accessed Jan. 24, 2022).
- Yin J, et al: Int Immunopharmacol 2018; 54: 198-209.
- Razi, CH et al: J Allergy Clin Immunol 2010; 126(4):763-769.
- Salzmann M, et al: Journal of Innate Immunity 2021; 1-13.
- Gomez Perdiguero E, et al: Nature 2015; 518: 547-551.
- Schneberger D, Aharonson-Raz K, Singh B: Cell Tissue Res 2011; 343: 97-106.
- Herold S, et al: J Exp Med 2008; 205: 3065-3077.
HAUSARZT PRAXIS 2022; 17(2): 18