For moderate to severe depressive episodes, the efficacy of treatment with antidepressants is considered proven. Remission-stabilizing maintenance therapy is an important aspect to reduce the risk of relapse. As a relapse prophylaxis, antidepressant treatment should be continued for several months in patients with unipolar depression after successful acute therapy. In addition to efficacy, good tolerability is a decisive criterion for long-term therapy adherence.
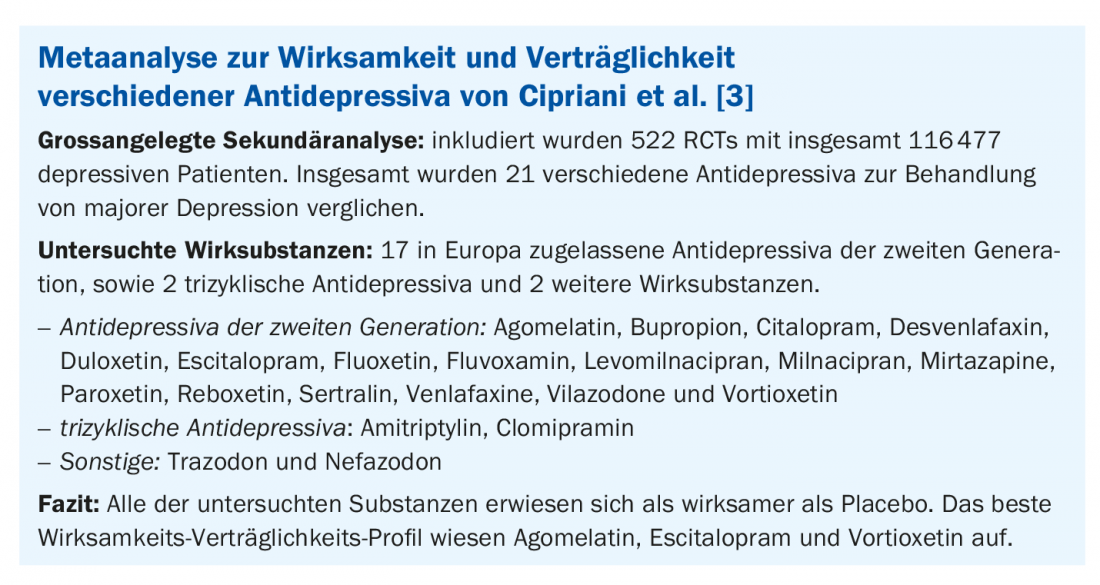
According to current guidelines, pharmacological treatment is recommended for moderate and severe depression, and for mild depressive episodes only if specifically requested by the patient [1]. In a meta-analysis, Fournier et al. show that with increasing severity of depression, the benefit of drug treatment increases in a placebo comparison. Above a Hamilton Depression Rating Scale score of 25, the difference proved to be clinically significant [2]. Included in this secondary analysis were 6 randomized-controlled trials (RCTs) with a total of over 700 patients, each treated with antidepressants for a duration of at least 6 weeks. Further confirmation that antidepressant medication therapy is effective in patients with major depression is provided by a meta-analysis published in the Lancet, which compared 21 different antidepressants in more than 116,000 patients (box) [3]. One conclusion was that all of the antidepressant agents studied were more effective in placebo comparisons in this patient population. Clinically relevant efficacy was operationalized as a reduction of at least 50% in the total score of a standardized depression scale after a treatment period of 8 weeks. The best performers in terms of efficacy and tolerability were agomelatine, escitalopram, and vortioxetine. Vortioxetine (Brintellix®) is one of the newer antidepressants; it was approved in Switzerland in 2016 [1,7].
Adequate maintenance therapy has been shown to reduce the risk of relapse
Good tolerability is an important criterion in selecting the appropriate antidepressant medication. The current DGPPN guideline recommends continued use of an antidepressant for at least 4-9 months beyond remission of a depressive episode because this can significantly reduce the risk of relapse [4]. In older patients, a longer duration of therapy is also discussed, especially in the presence of depression-promoting factors or recurrent depression. In the maintenance phase, the same dosage as in the acute phase should be continued. Dose reduction increases the risk of relapse, the authors of the DGPPN guidelines state. However, when discontinuing remission-stabilizing treatment, antidepressants should be phased out. It is recommended that discontinuation of an antidepressant be gradual over a period of 4 weeks with regular progress monitoring [4].
Therapy goal full remission achieved?
The importance of complete remission also stems from the fact that patients with only partially remitted depression have a significantly increased risk of relapse. The more severe depressive episodes were, the more likely there is an indication for relapse prophylaxis. The goals are to protect against relapse and to prevent possible worsening of symptoms. The remission-stabilizing effect has been demonstrated for numerous antidepressants. Adequate maintenance therapy can reduce the risk of relapse by up to 70% [4].
Individually adjusted recurrence prophylaxis recommended
Long-term relapse prophylaxis is indicated in patients at high risk of relapse [4]. Medication options include antidepressants and dosages already effective in acute and maintenance therapy [5]. Studies show that maintaining the dosage effective in acute therapy is associated with a recurrence prophylactic effect, whereas conversely there is no empirical evidence for dose reduction [6]. The individual propensity for recurrence can most readily be inferred from the previous individual course. The more depressive phases a patient has already had and the shorter the interval between them, the more likely it is that further relapses will occur soon. In this assessment, the course of the recent past is of greater significance than the course in years far in the past. Other important criteria to consider for or against the indication of long-term relapse prophylaxis include the severity of previous episodes of illness, previous suicidality, and previous response to antidepressants.
Literature:
- Cattapan K, Seeher C: Pharmacologic management of unipolar depression: acting with a biopsychosocial perspective. InFo Neurology & Psychiatry 2019(17) 2: 20-25.
- Fournier JC, et al: Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA 2010; 303(1): 47-53.
- Cipriani A, et al: Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet 2018; 391(10128): 1357-1366.
- DGPPN: S3-Leitlinie/Nationale VersorgungsLeitlinie Unipolare Depression Langfassung 2. Auflage, 2015 Version 5, AWMF-Register-Nr.: nvl-005.
- American Psychiatric Association (APA). Practice guideline for the treatment of patients with major depressive disorder. Arlington: American Psychiatric Association (APA); 2010.
- Geddes JR, et al: Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review. Lancet 2003; 361(9358): 653-661.
- Technical Information, www.swissmedicinfo.ch (last accessed 11/19/2021).
InFo NEUROLOGY & PSYCHIATRY 2022; 20(1): 24.