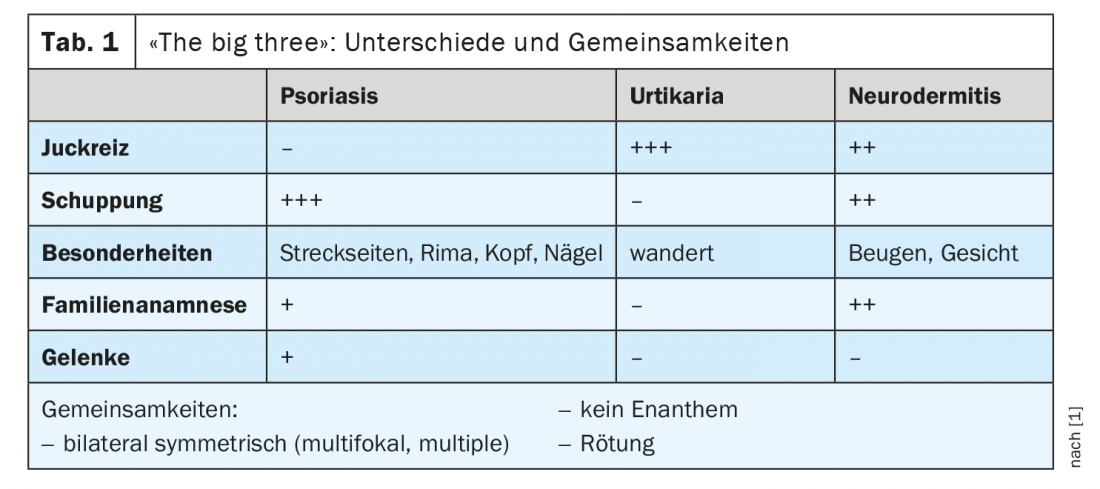
In psoriasis as well as in atopic dermatitis and urticaria, the primary goal of treatment is to achieve symptom control and symptom relief, respectively. The therapy is stage-adapted. Because these are relapsing-remitting dermatoses, it is important to recognize exacerbations early and treat them adequately. Thus, the correct assignment of clinical manifestations is crucial.
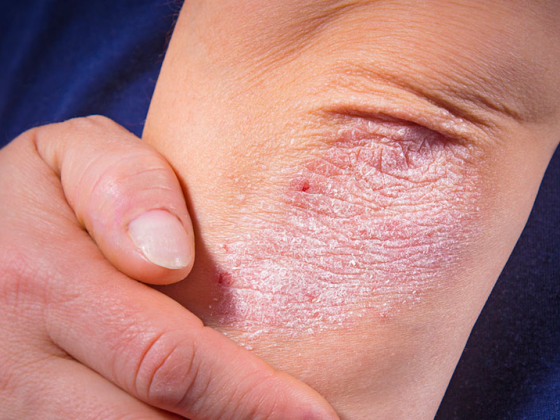
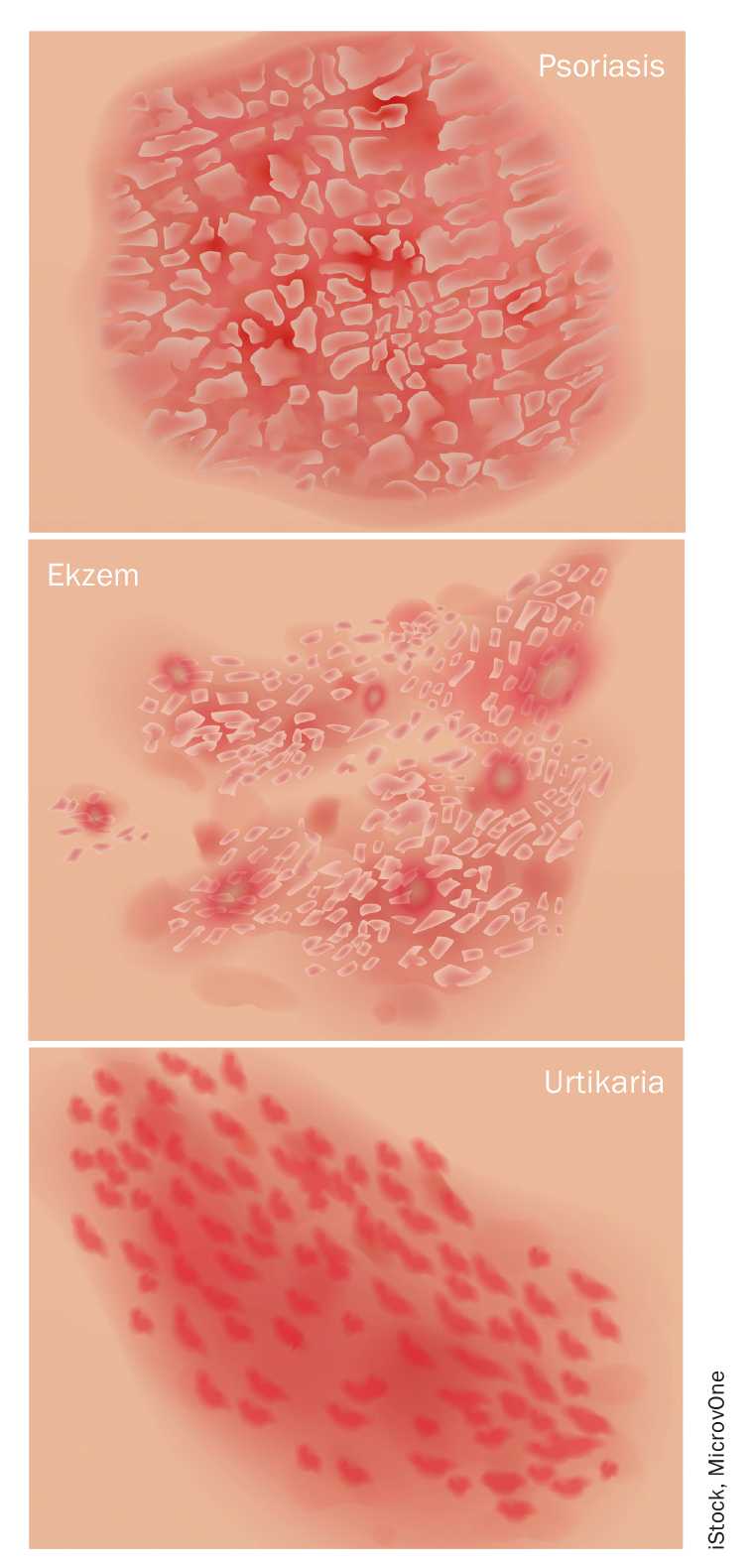
Scaly and inflammatory red skin – is it psoriasis or not? “Psoriasis is a very heterogeneous disease with different forms of manifestation,” explains Dr. med. E. Paul Scheidegger, Allergie & Haut AG, specialist in dermatology and venereology, especially allergology and clinical immunology, Brugg [1]. 80-90% of psoriatic patients are affected by plaque psoriasis. Typical symptoms are focal scaly plaques with a rough surface. Predilection sites are knee, elbow, sacrum or scalp. Nail and joint involvement is common (overview 1) . Other forms include guttate psoriasis (<10%), inverse psoriasis (<5%), pustular psoriasis (<5%), and erythrodermic psoriasis (<2%). Psoriasis inversa is often confused with Candida intertrigo. In the pustular psoriasis subtype, small pustules form on the skin and are filled with sterile pus, a differentiating feature from bacterial pyoderma. Most often, palms and the arch of the foot are affected.

Psoriasis – basic care and when systemic therapy is needed
In all stages of psoriasis, adequate basic care is important, emphasizes Dr. Scheidegger. In this context, keratolytic therapy for desquamation is central (e.g. Excipial® Kerasal ointment, Excipial® U Lipolotio 4% Urea, Lotio Decapans (Scalp)®) [2]. The next step in the treatment regimen is vitamin D preparations (calcipotriol) and topical class III corticosteroids, e.g. Daivobet® ointment or Enstilar® foam [2]. UVB light therapy can also alleviate the symptoms of psoriasis, but is relatively costly, as several irradiations per week are necessary. In the case of moderate to severe symptoms, it is important to initiate systemic therapy at an early stage, the speaker emphasized. Classic systemic agents for the treatment of patients with psoriasis include methotrexate, ciclosporin, acitretin, and fumaric acid esters.
To minimize side effect risks, recommendations regarding dosing regimens and laboratory diagnostic follow-up should be followed [2]. The use of the oral phospodiesterase (PDE)-4 inhibitor apremilast is particularly appropriate when enthesitides are present. “Steroids should rather be avoided, only in case of emergency, 50-100 mg over a few days,” said Dr. Scheidegger [1]. If >30% of the body surface is affected by psoriasis or joint involvement is present and methotrexate has proven insufficiently effective or tolerated, he recommends a rapid switch to biologicals. These modern therapeutics are veritable “game changers,” he said. The biologics used in psoriasis therapy today include TNFα, IL-17, IL-12/23, or IL-23 antagonists. Therapy with the new generation of monoclonal antibodies can continue during the corona pandemic, the speaker said.
Atopic dermatitis – barrier disruption and Th2-mediated inflammation.
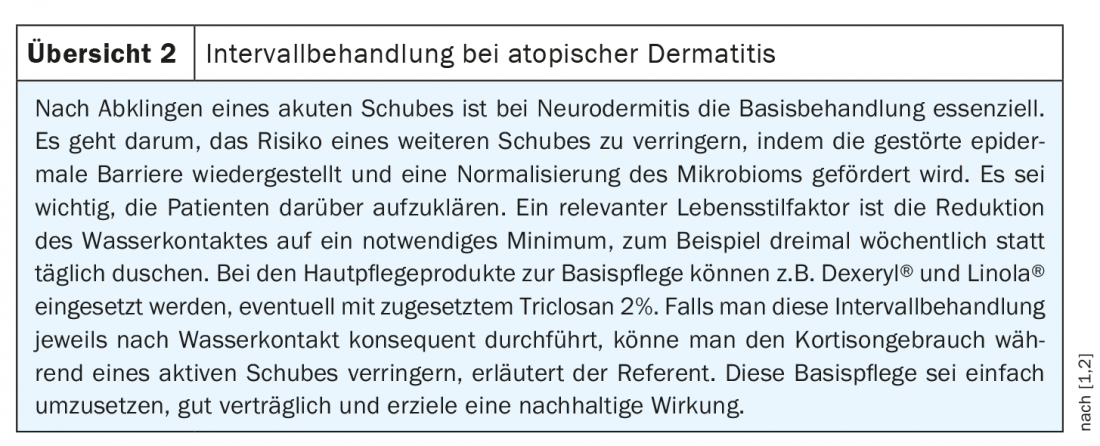
According to current understanding, atopic dermatitis is an immune-mediated chronic inflammatory dermatosis. Th2-mediated inflammation and an epidermal barrier defect are among the most important pathogenetic factors. Features of atopic dermatitis are symmetrical, red, rough, itchy, stationary lesions with predilection sites at the flexures. A positive family history is present in up to 75% of cases. Therapy is adapted to the different stages, with interval treatment playing an important role (overview 2). Corticosteroids (e.g. Fucicort® cream 2%) or calcineurin inhibitors can be used for topical acute treatment [2]. “On the face, we always use the calcineurin inhbitors because the skin is much thinner there,” Dr. Scheidegger said. Tacrolimus (Protopic 0.03%®) or pimecrolimus (Elidel®) have good efficacy, the myth of long-term side effects has never been proven, the speaker said [1,2]. A slight burning sensation at the beginning of the treatment is a harmless local reaction. With regard to light therapy (UVB), as with psoriasis, the high expense is an obstacle. For moderate or severe atopic dermatitis, a systemic treatment is the therapy of choice. When cyclosporine is used, blood pressure and creatinine levels should be checked regularly. Methotrexate and azitretin are nowadays only of secondary importance. If cyclosporine treatment does not lead to the desired improvement within a reasonable period of time, one often switches directly to therapy with the monoclonal antibody Dupilumab (Dupixent®), said the speaker [1,2]. Treatment with Dupixent® is effective in 60-70% of cases, so that hospitalization of severely ill neurodermatitis patients is usually unnecessary nowadays.
Urticaria – Spontaneous or induced form?
Characteristic of hives/urticaria are red, itchy wheals or blisters on the skin. It is a common condition with a lifetime prevalence of approximately 20% [3]. A mast cell-mediated pathomechanism is far more common than a bradykinin-mediated one. If the symptoms persist for more than 6 weeks, it is chronic urticaria, whereby a distinction is made between an inducible and a spontaneously occurring form. By far the most common, he said, is chronic recurrent postinfectious urticaria. However, the idiopathic forms are also very common [6]. If autoimmune diagnostics are considered, Dr. Scheidegger recommends determination of TSH and anti-nuclear antibodies (ANA) [7].
Since urticaria is often drug-induced, the following active substances should be discontinued or replaced by drugs from another group of active substances if possible: NSAIDs, aspirin, gliptins, ACE inhibitors, sartans [1]. Apart from certain substances, inducible urticaria can also be triggered by physical stimuli (e.g. cold, heat, pressure, light, mechanical irritation, vibration, sports activity). Non-sedating second-generation H1 antihistamines are considered first-line treatment for chronic urticaria; if not effective, biologic therapy (omalizumab) may provide relief [1,5] (box ). “Very rarely, acute urticaria may be a partial symptom of an allergic, life-threatening situation. This occurs in less than 1% of those affected by acute urticaria,” he said. In these cases, the exanthemas occur a short time after contact with the allergen, e.g. after consumption of certain foods or an insect sting, and are accompanied by shortness of breath, dyspnea, and dizziness as typical symptoms of a severe drop in blood pressure. Angioedema without urticaria is a “red flag” that requires further workup.
Congress: FomF Family Doctor Training Days St. Gallen
Literature:
- Scheidegger EP: Dermatology 2021. The big three in dermatology – neurodermatitis, urticaria, psoriasis. FomF, Family Physician Continuing Education Days, Mar. 11, 2021.
- Drug Information, www.swissmedicinfo.ch, (last accessed 05/10/2021).
- Zuberbier T, et al: The EAACI/GA²LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy 2018; 73(7): 1393-1414.
- Maurer M: Urticaria, Angioedema, in: Allergo Update 2014, Handbuch Allergologie 2014. http://marcus-maurer.com (last accessed 10.05.2021).
- Maurer M, et al: Chronic urticaria – What does the new guideline bring? JDDG 2018; 16(5): 585-595.
- Maurer M, et al: Pathogenesis of chronic spontaneous urticaria. Medical Journal Dermatology 2018; 2: 20-22.
- (Allergy 2017) Kolkhir P, et al: Comorbidity of chronic spontaneous urticaria and autoimmune thyroid diseases: A systematic review. Allergy 2017; 72(10): 1440-1460. doi: 10.1111/all.13182. epub 2017.
HAUSARZT PRAXIS 2021; 16(6): 30-31 (published 8.6.21, ahead of print).