The natural aging process of the face leads to a loss of volume caused by the resorption of subcutaneous tissue. Over the years, not only the superficial and deep fat pads of the face are resorbed, but also the bone tissue. All these tissue changes lead to a gradual mobilization of the skin and soft tissues in a postero-anterior direction. Thus, a face that has a triangular shape when young gradually takes on a rectangular shape.
The natural aging process of the face leads to a loss of volume caused by the resorption of subcutaneous tissue. Over the years, not only the superficial and deep fat pads of the face are resorbed, but also the bone tissue. The ligaments that anchor the skin to the skull, muscles or muscle fascia also lose their elasticity over time. All these tissue changes lead to a gradual mobilization of the skin and soft tissues in a postero-anterior direction. Thus, a face that has a triangular shape when young gradually takes on a rectangular shape.
Many minimally invasive treatments are currently available to restore youthful facial shape. This article discusses hyaluronic acid fillers and some types of sutures used in thread lift.
Fillers and threads – what do they have in common?
The best-known function of thread lifting is to reposition the subcutaneous tissue in the anteroposterior direction. They also have the function of stimulating the formation of new collagen subcutaneously. The fillers, in turn, were developed mainly to fill volume loss.
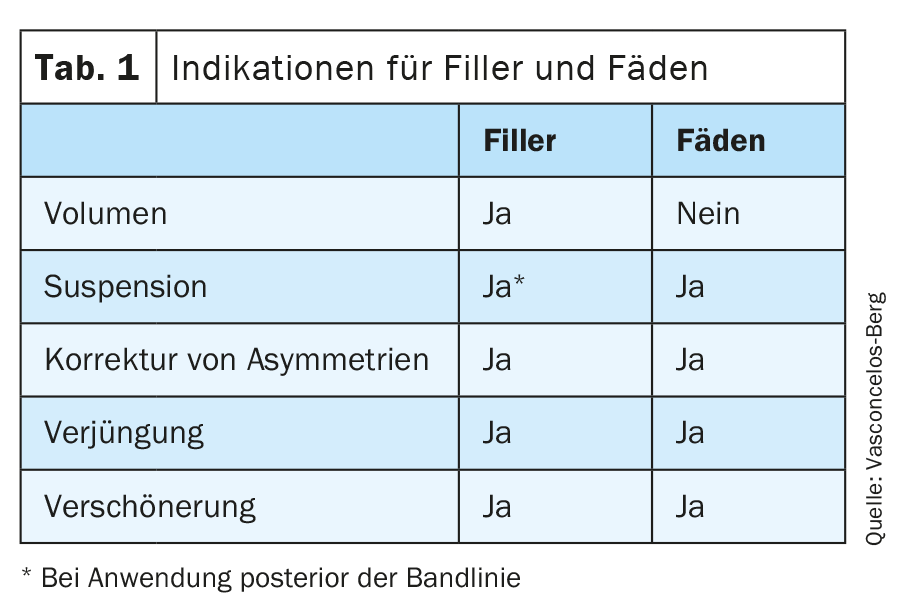
However, fillers and sutures have some common indications (Tab. 1) . Both can be used for rejuvenation as well as for beautification or correction of asymmetries. Although threads are better known for their function of suspending facial structures, fillers, when applied to strategically correct areas of the face, can also create a lifting effect.
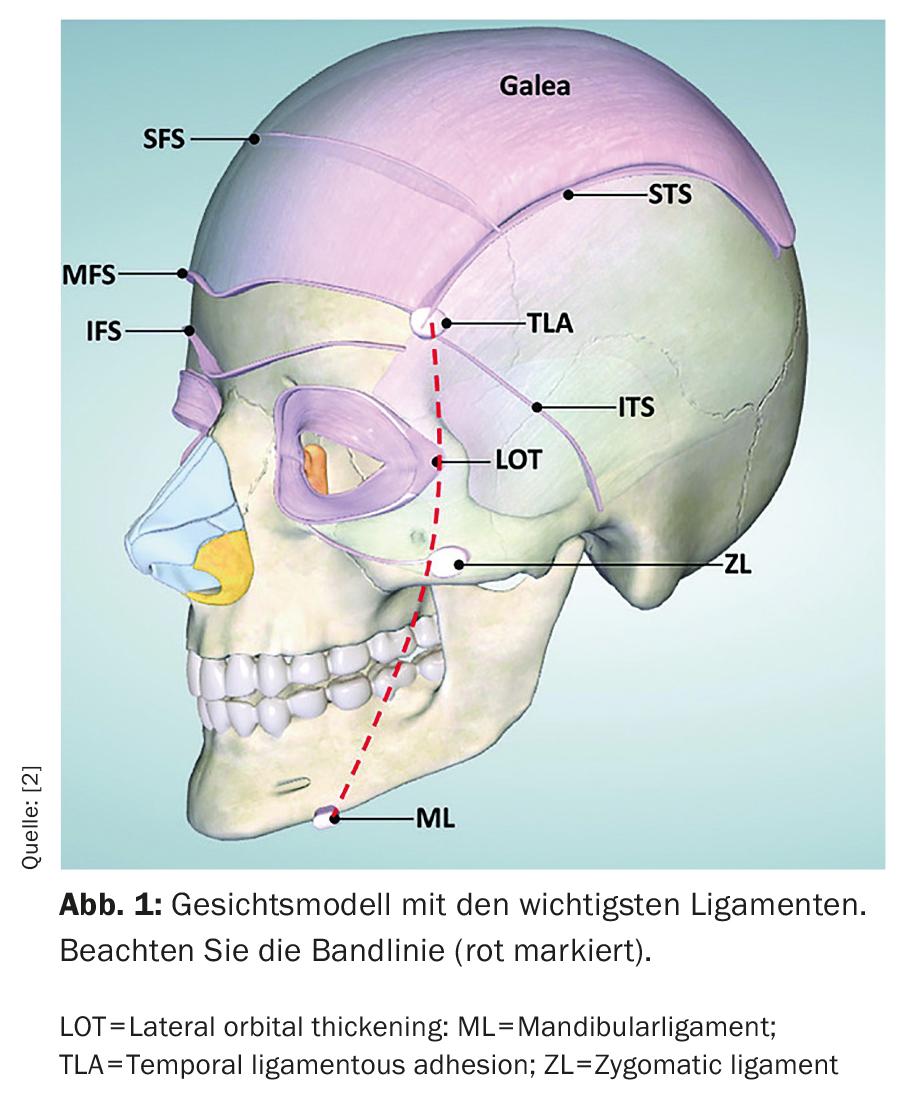
In 2019, physician Dr. Sebastian Cotofana [1] described an imaginary line that connects vertically with the ligaments of the face, which he called the “ligament line” (Fig. 1). In the same year, an interesting study by his team [2] showed that injections of hyaluronic acid subsequently applied to this line indirectly increased the volume of the medial facial region by causing a “lifting” effect. Treatment with hyaluronic acid in this region requires much smaller amounts than usual.
Filler: Classification
The first treatment with fillers was described by Neuber in Germany in 1883, when a loss of volume in the face was treated by fat grafting [3]. A few years later, liquid kerosene was used for filler purposes [4], and over the years many types of synthetic materials have been used as fillers. The ideal filler should be easy to handle, remain in the tissue for a long period of time, have no allergenic, oncogenic or biofilm-forming potential. It should still be potentially reversible, stable at various temperatures, and cost effective. Unfortunately, none of the available fillers currently fully meets all of these criteria [5].
The various fillers can be classified as absorbable, semi-permanent (or biostimulating), or permanent [5]. Currently, hyaluronic acid (HA) is the only absorbable filler available. Until 2010, this group also included bovine collagen fillers, which were withdrawn from the market due to their high allergenic potential.
The group of semi-permanent fillers or biostimulants consists of poly-L-latic acid (PLLA), calcium hydroxyapatite and polyaprolactone (PCL). These are materials that are absorbed by the organism over months and trigger a local inflammatory reaction with foreign body reactions and collagen formation types I and III. Thus, the filling is not caused by the material itself, but by the individual’s own collagen, and the effect is longer than that of hyaluronic acid, but not permanent. Permanent fillers such as silicone and polymethylacrilate (PMMA), which were widely used in the past, are very rarely used due to the greater potential for complications. In our article, we mainly discuss hyaluronic acid fillers.
Hyaluronic acid
Hyaluronic acid (HA) was first used commercially in 1942. HA is located in the intercellular matrix of connective tissue [6]. The unique properties in terms of biocompatibility, biodegradability and viscoelasticity have made HA an ideal biomaterial for cosmetic and medical purposes.
Due to its water binding capacity, HA is responsible for skin hydration, collagen retention, elasticity and flexibility. Hyaluronic acid attracts and binds more than 1000 times its weight in water. Skin hydration is critically dependent on HA-bound water content in the dermis and epidermis. HA of the dermis, together with the lymphatic and vascular systems, regulates water balance, osmotic pressure and acts as a sieve, excludes certain molecules, improves the extracellular domain of cell surfaces and stabilizes skin structures [7]. The favorable characteristics consist of limited allergic reactivity, availability of an antidote, and a wide range of products that meet different aesthetic goals.
HA is absorbed and eliminated over the course of months. To increase resistance to degradation without altering biological activity, HA molecules must be cross-linked. Cross-linked HA fillers contain solid elastic and liquid viscous components [8].
Treatment techniques
Mastery of filler techniques and knowledge of facial anatomy and its possible anatomical variations are the best way to avoid serious complications due to the use of fillers. Not only is it important to understand muscle dynamics and age-related anatomic changes, but it is also important to be familiar with the facial vascular network to avoid side effects and complications, which are discussed below.
Listed below are the most common injection techniques. The choice of injection technique depends on the indication, the filler substance, the size of the needle and the experience of the practitioner [9].The techniques include:
A) Linear or tunnel technique: The entire filler is injected during the removal process. The key to the tunnel technique is the angle at which the needle or cannula is inserted into the skin. For best results, insert the needle or cannula at an oblique angle of 30 to 45 degrees according to the direction of the fold.
B) Serial puncture: the puncture technique, also known as the “droplet” or “serial” technique, involves the injection of multiple small droplets of filler into the deeper layers of the dermis or even into the subcutaneous area.
C) Fanning: There is also a technique that allows us to spread the product over a larger area, called fanning. In a fan technique, after the needle is inserted under the skin, we place a linear product thread while pulling out the needle. Instead of removing the needle completely, we simply change the angle of the needle and then create another linear product thread back to the insertion point. We can repeat these threads in a radial pattern.
D) Cross-Hatching: In this technique we start by injecting a series of linear threads. We then change the angle of the needle so that it deviates 90 degrees and then inject another row of linear filaments, all perpendicular to the first row.
E) Depot: The physician squeezes the skin with the hand to achieve maximum penetration and pierces the skin at the thinnest entry point using a 90° angle. At the level of the bone, the needle is repositioned and slowly pushed under the soft tissue before material deposition, without causing pain to the patient.
Possible complications and how to avoid them
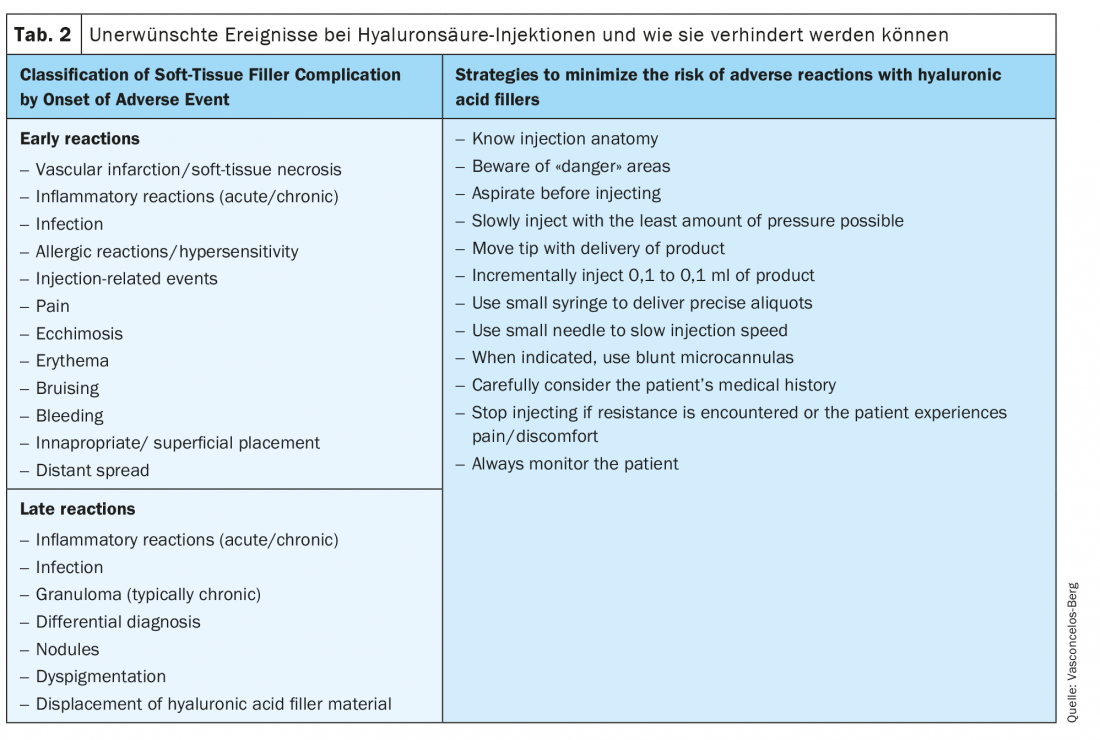
Several complications have been reported with filler injections. HA fillers can cause early-onset and delayed-onset complications. Early-onset complications occur hours to days after treatment, while delayed-onset complications typically develop weeks to years after HA filler treatment.
The most feared complication is arterial vessel occlusion with tissue necrosis or embolism. Some measures during treatment, such as the use of blunt cannulas, aspiration, and slow injection in small aliquots, reduce the likelihood of such an adverse event. Table 2 [10] summarizes the main adverse events caused by hyaluronic acid and the strategies to avoid them.
An interesting anatomical study of cadavers [11] examined the strength required to penetrate the facial arterial vasculature with blunt cannulas and needles of different calibers and concluded that blunt cannulas calibers greater than 25 gauge are significantly safer than needles of the same caliber.
Contraindication for treatment with HA
The main contraindications to the use of a filler are an active infection near the injection site, a known allergy/hypersensitivity to lidocaine. No association has been established between filler use and autoimmune diseases such as dermatomyositis, lupus erythematosus, and rheumatoid arthritis [12].
The relative contraindications are the use of anticoagulants, especially for needle procedures, dental appointments scheduled within the next 15 days, history of granulomatous reactions to HA, and the presence of unknown fillers in the area to be treated. The last factor could lead to a higher risk of late-onset reactions to hyaluronic acid.
Thread lifting
Treatment with thread lifting for aesthetic reasons was first reported in the late 1980s by Sulamanidze et al. [13] described. Sutures are another less invasive method of repositioning subcutaneous tissue that can also be used to rejuvenate the face and provide a lifting effect. They can also be used to achieve correction of minor facial imperfections.
This procedure should ideally be used when little or no additional volume is desired. Best results are achieved in patients with low or moderate skin laxity, low body mass index, and mild fat prolapse [14].
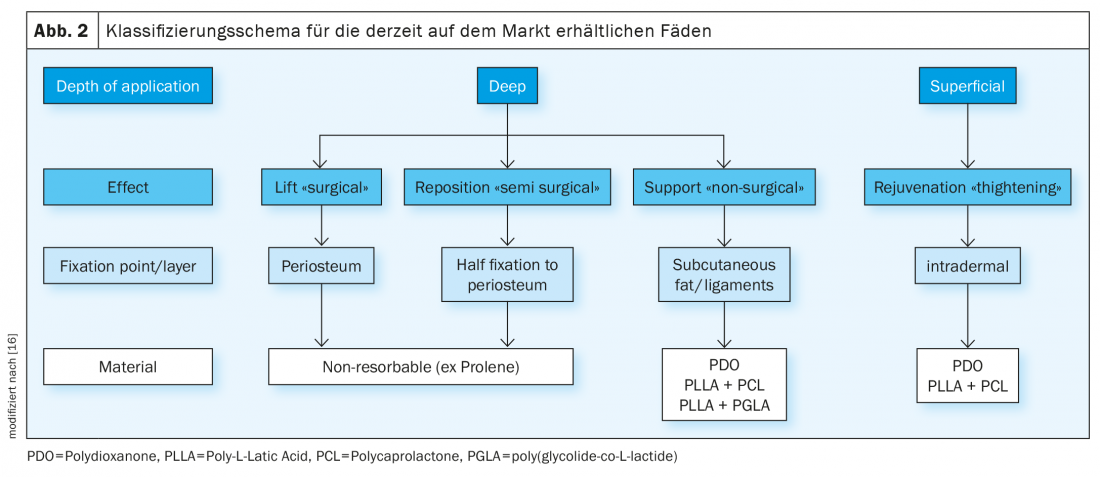
Currently, there are several types of threads on the market. Figure 2 shows the classification. In the following text we describe the threads available today:
Application depth
The sutures can be attached to the periosteum, resulting in a facelift, or anchored to the subcutaneous adipose tissue or ligaments, resulting in a repositioning of the face without causing a facelift. There are non-anchoring sutures whose function is only to remain in the intradermal area and stimulate local collagen production.
Material and absorption
The sutures can be made of different materials, be absorbable or permanent. The most commonly used absorbable sutures are made of polydioxanone (PDO), polylactic acid (PLA), polycaprolactone (PCA), or polylactide-co-glycolide (PLGA). Prolene belongs to the permanent threads.
Application path
The method of inserting the threads and their shape and texture vary depending on the material and manufacturer. Knowledge of the anatomy and application techniques is extremely important to avoid damaging the structures or applying the sutures very superficially.
The sutures can be attached to the periosteum. The application can also be done in a practice. Often a needle or blunt cannula is used, which attach to the tip of the thread. In the case of blunt cannulas, the puncture must first be made with a pointed needle. In cases where a tissue repositioning effect is desired, the sutures are inserted parallel to the skin into the superficial fat compartment and then pulled to achieve the desired direction of pull and then cut. Fixation is achieved by the presence of barbs along their length that adhere to subcutaneous tissues.
In cases where the pulling effect is not desired, such as PDO sutures where the goal is only secondary collagen stimulation, the suture usually does not have barbs for attachment. The sutures remain in the subcutaneous tissue, causing a foreign body reaction with subsequent collagen formation.
Contraindications
The contraindications to the use of sutures are:
- Active infection at the injection site (herpes, acne, impetigo, etc.)
- Systemic or local infection at the time of treatment
- Use of anticoagulants, especially for needle procedures
The sutures should not be used in areas where hyaluronic acid is present, as the hydration of hyaluronic acid may accelerate the degradation of the sutures, which normally occurs by hydrolysis. The application of sutures to sites where implants of unknown material are present may increase the risk of local reactions such as foreign body granulomas [15].
The procedure requires some care, such as analgesia, avoidance of facial massage, and excessive facial movement or exercise for about 2 to 4 weeks after treatment.
The most common side effects are swelling, bruising, skin dimpling, or buttoning and occur in most patients (Fig. 3). Patients must be informed about the expected downtime and care after the procedure. The less common adverse events are infection, pain, ecchymosis, paresthesias, inadequate cosmetic results, migration, and suture exposure. They can be avoided by good knowledge of facial anatomy, antiseptic practice, and proper training of the physician.
Take-Home Messages
- Fillers and sutures are important tools in the field of aesthetic dermatology for facial rejuvenation.
- Knowledge of the pathomechanism of deep facial aging helps in planning treatment goals.
- Fillers and sutures have some similarities and some specific indications.
- Knowledge of facial anatomy is critical to avoid complications.
- Through continuous training and practice, the treating physician can avoid unnecessary complications and side effects and achieve natural results.
Literature:
- Cotofana S, Lachman N: Anatomy of the Facial Fat Compartments and their Relevance in Aesthetic Surgery. J Dtsch Dermatol Ges 2019; 17(4): 399-413.
- Casabona G, Frank K, Koban KC, et al: Lifting vs volumizing-The difference in facial minimally invasive procedures when respecting the line of ligaments. J Cosmet Dermatol 2019; doi: 10.1111/jocd.13089. epub ahead of print.
- Kim JE, Sykes JM: Hyaluronic acid fillers: history and overview. Facial Plast Surg 2011; 27(6): 523-528.
- Gersuny R: The classic reprint. Concerning a subcutaneous prosthesis. Zeitschrift f. Heilkunde Wien u Leipzig 1900; 21: 199. Translated from the German by Miss Rita Euerle. Plast Reconstr Surg 1980; 65(4): 525-527.
- Aitzetmüller MM, Sukhova I, Huemer GM, et al: Injectable fillers – update and future perspectives [Soft tissue fillers: state of the art and future perspectives]. Handchir Microchir Plast Chir 2017; 49(6): 423-431.
- Liao YH, Jones SA, Forbes B, et al: Hyaluronan: pharmaceutical characterization and drug delivery. Drug Deliv 2005; 12(6): 327-342.
- Stern R, Maibach HI: Hyaluronan in skin: aspects of aging and its pharmacologic modulation. Clin Dermatol 2008; 26(2): 106-122.
- Lipko-Godlewska S, Bolanča Ž, Kalinová L, et al: Whole-Face Approach with Hyaluronic Acid Fillers. Clin Cosmet Investig Dermatol 2021; 14: 169-178.
- Vedamurthy M, Vedamurthy A: Dermal fillers: tips to achieve successful outcomes. J Cutan Aesthet Surg 2008; 1(2): 64-67.
- Signorini M, Liew S, Sundaram H, et al: Global Aesthetics Consensus Group. Global Aesthetics Consensus: Avoidance and Management of Complications from Hyaluronic Acid Fillers-Evidence- and Opinion-Based Review and Consensus Recommendations. Plast Reconstr Surg 2016; 137(6): 961e-971e.
- Pavicic T, Webb KL, Frank K, et al: Arterial wall penetration forces in needles versus cannulas. Plast Reconstr Surg 2019; 143(3): 504e-512e.
- Lafaille P, Benedetto A: Fillers: contraindications, side effects and precautions. J Cutan Aesthet Surg 2010; 3(1): 16-19.
- Tavares JP, Oliveira CACP, Torres RP, et al: Facial thread lifting with suture suspension. Braz J Otorhinolaryngol 2017; 83(6): 712-719.
- Tong LX, Rieder EA: Thread-Lifts: A Double-Edged Suture? A Comprehensive Review of the Literature. Dermatol Surg 2019; 45(7): 931-940.
- Shin JJ, Park TJ, Kim BY, et al: Comparative effects of various absorbable threads in a rat model. J Cosmet Laser Ther 2019; 21(3): 158-162.
- Turkevych A: Presentation at IMCAS Paris 2020.
DERMATOLOGIE PRAXIS 2021; 31(2): 4-8












