Diaper dermatitis is a common condition in infants and incontinent persons, which is directly related to the wearing of a diaper. It heals without complications in most cases. The symptoms correspond to those of acute to subacute eczema. Taking good care of the genital area is effective in preventing diaper dermatitis and essential in treating it. Regular, frequent diaper changes are essential.
Diaper dermatitis refers to toxic-irritant contact dermatitis in the diaper area in newborns and infants and in incontinent patients and is directly related to the wearing of a diaper. The disease occurs in about 50-65% of all babies [1]. Infants between the ninth and twelfth month of life are most affected [1]. About seven percent of parents whose infants suffer from wind dermatitis visit the pediatrician because of it [2].
The causes
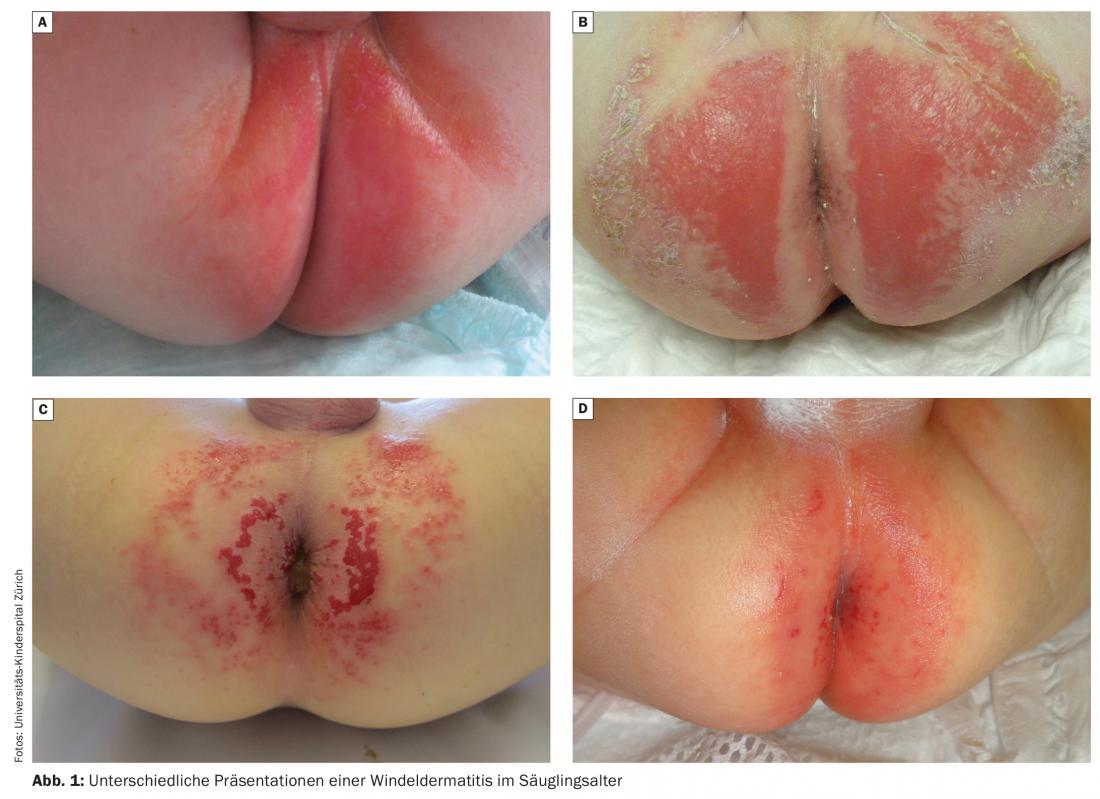
The causes of diaper dermatitis are multifactorial. Symptoms may present in different ways (Fig. 1 ) . Diaper dermatitis develops when the intrinsic barrier function of the skin is exceeded. This is determined by various factors such as genetics, occlusion, wetness, friction, contact with irritant substances and infectious agents. The risk of diaper dermatitis is significantly increased by repeated and prolonged contact with urine or stool. Moisture and heat accumulate under the occlusive diaper, creating a moist chamber. As a result, the epidermis macerates and loses its protective function. Loses [3]. The urea in the urine is partially degraded to ammonia, which leads to an alkalinization of the skin pH. This leads to an activation of proteases and lipases in the stool, causing additional damage to the stratum corneum [4].
Risk factors in the development or exacerbation of diaper dermatitis include inappropriate diapering and care products, as tight diapers can chafe the skin and irritate or damage it. The use of rough fleece cloths or terry cloth washcloths can additionally lead to skin lesions when cleaning the already impaired skin. Lack of hygiene increases the risk of developing diaper dermatitis. Further, changes in dietary habits are also factors that may promote the development of diaper dermatitis [5]. Certain underlying conditions also increase the risk of diaper dermatitis. These include bowel or diarrheal disorders, as frequent and liquid bowel movements increase skin irritation. Taking antibiotics changes the pH of the stool and can promote diaper rash. Other favoring factors are a predisposition to skin diseases, such as atopic eczema, seborrheic eczema or generally dry skin with a limited skin barrier [6]. There is evidence that episodes of diaper dermatitis can occur following viral illness [7].
Clinical presentation
Symptoms correspond to those of acute to subacute eczema and include erythematous macules, papules, plaques, and, in more severe cases, erosions and even ulceration.
Due to the pathogenesis, primarily the convex skin areas in direct contact with the diaper are affected, whereas the flexures are free, at least initially. This represents an important criterion for distinguishing irritant diaper dermatitis from diaper thrush [8]. Touching the affected skin, as well as wet or full diapers, causes pain in the child and promotes additional skin irritation. Some parents are frightened at the sight because symptoms can develop and worsen very quickly – within a few hours. Diaper dermatitis can lead to severe itching in the genital area if bacterial colonization or candidiasis is present [5].
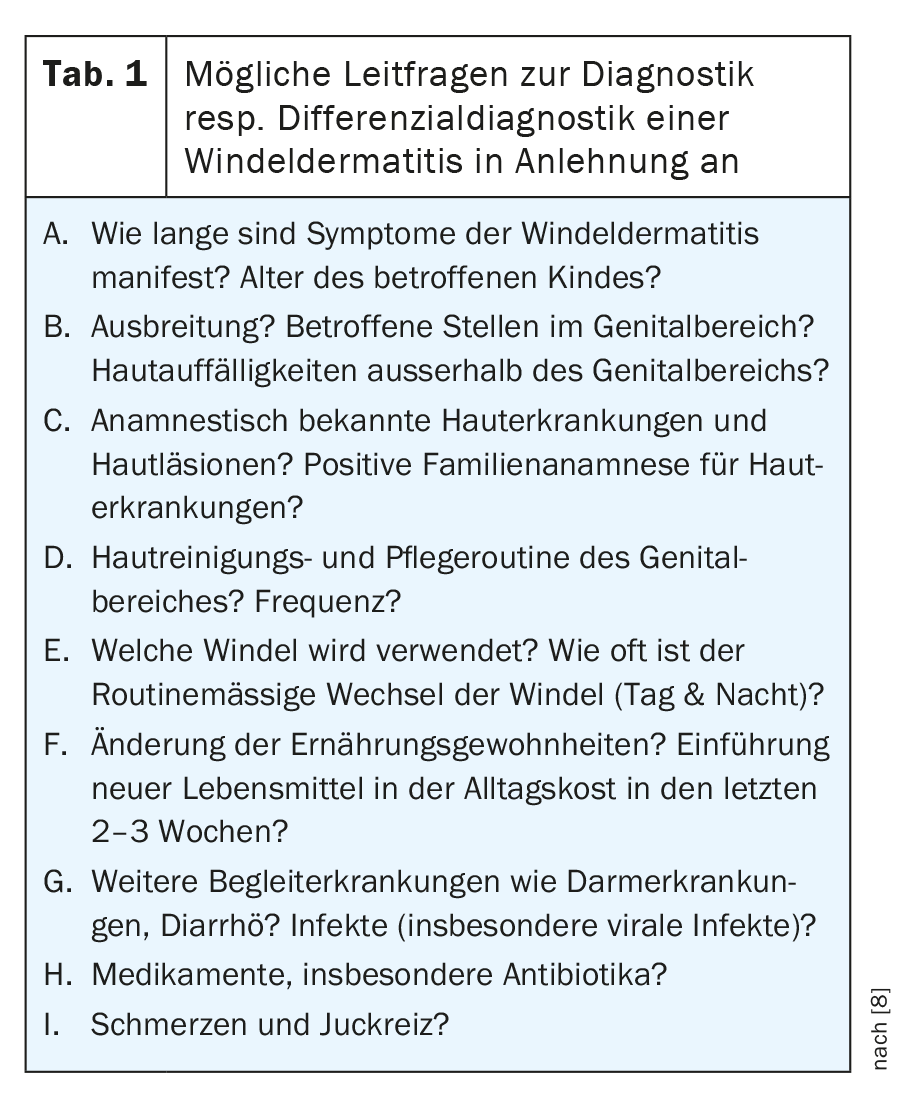
The guiding questions in Table 1 can provide support for the diagnosis and the recognition of any differential diagnoses.
Correct diagnosis of diaper dermatitis is important to reduce serious complications such as secondary infections and deep skin lesions.
Differential diagnoses of diaper dermatitis
Differential diagnoses of diaper dermatitis should be considered especially when skin manifestations in the diaper area persist for a long time without a clear external trigger and when skin manifestations exist outside the diaper area. In the following, we briefly review individual differential diagnostic manifestations. This overview represents a selection of common and/or important diagnoses and is not exhaustive:
a. Candida infection / diaper thrush
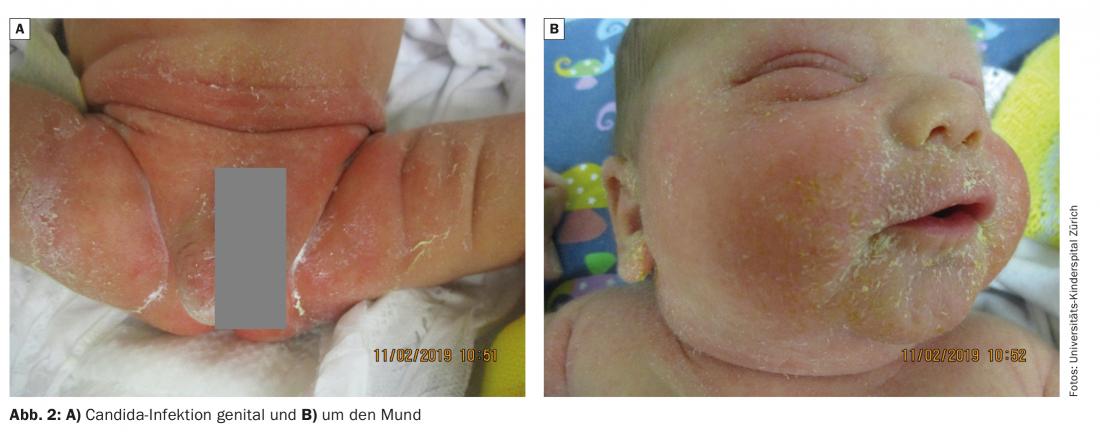
Superinfection with Candida often occurs in the course of irritant diaper dermatitis. Thus, it is assumed that in the majority of diaper dermatitis lasting longer than 3 days, a relevant Candida colonization is present. Another important risk factor is previous antibiotic treatment. This presents clinically with erythematous macules and plaques in the flexural folds and around the genitals with marginal scaling. In addition, satellite papules and pustules are characteristic. The child often suffers from severe pruritus and begins to scratch when changing diapers (Fig. 2A+B). If symptoms are unclear, a smear test is indicated. Treatment is with topical antifungal therapy [7].
b. Allergic contact dermatitis
Allergic contact dermatitis in the diaper area must be distinguished clinically from “simple” diaper dermatitis. Allergic contact dermatitis is triggered by conservatives, emulsifiers, fragrances, emulsion paints, adhesives and plastic components. Known problematic components of these ingredients are no longer used in modern disposable diapers [9]. Clinically, allergic contact dermatitis often manifests as acute eczema with vesicles, papules and plaques, some of which are weeping. The distribution may also be indicative of allergic contact dermatitis. The appearance laterally in the pelvic region, for example, suggests a contact allergy to rubber ingredients of disposable diapers and has been known as “Lucky Luke dermatitis” [10,11]. Ingredients such as methylisothiazolinone in wet wipes can also cause contact allergies [10].
c. Seborrheic eczema / psoriasis
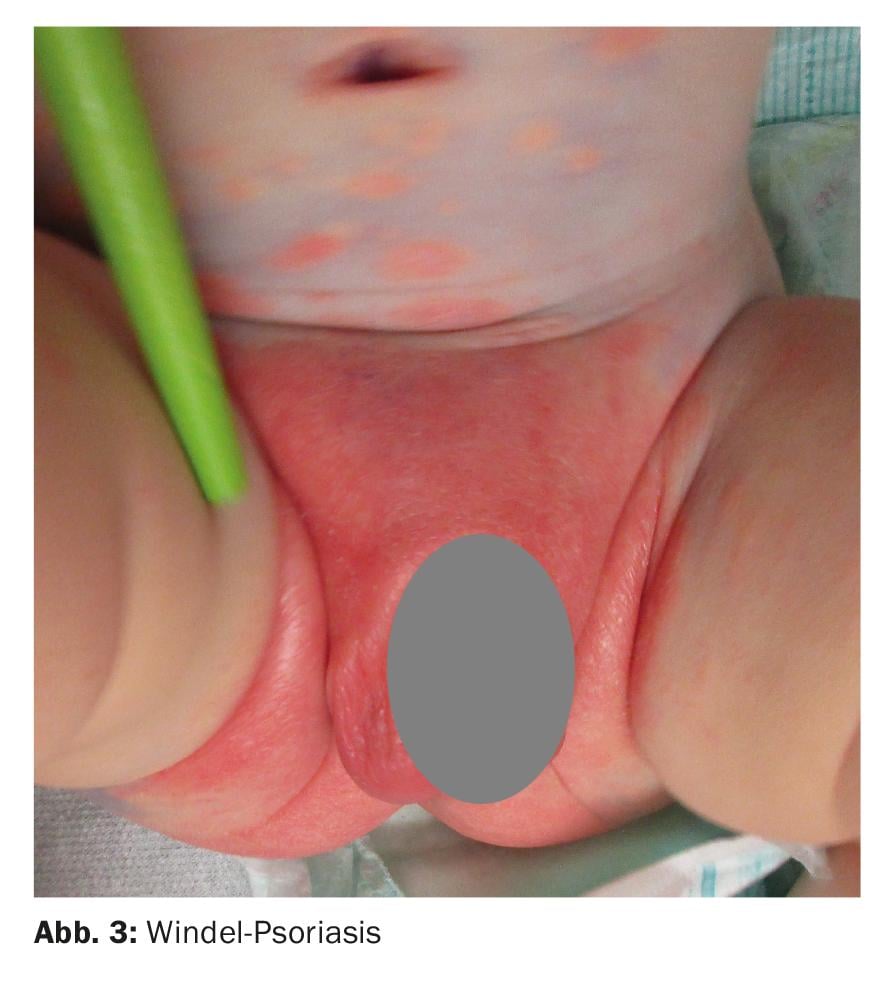
Infantile seborrheic eczema is a benign inflammatory skin disease that typically occurs in the neonatal period or shortly thereafter. The inflammatory skin lesions often occur on the face/scalp and, in more extensive forms, also characteristically in the genital region (Fig. 3). In contrast to atopic eczema, there is little itching. Sometimes difficult to distinguish from it resp. partly also overlapping is infantile psoriasis. This often primarily affects the diaper area and is characterized by very sharply demarcated, flame-red erythema with sharp borders. Other sites such as the face to the entire integument may be affected. Infantile psoriasis occurs either primarily (often with a positive family history) or more commonly as psoriasiform usually in the setting of Candida infection.
d. Langerhans cell histiocytosis
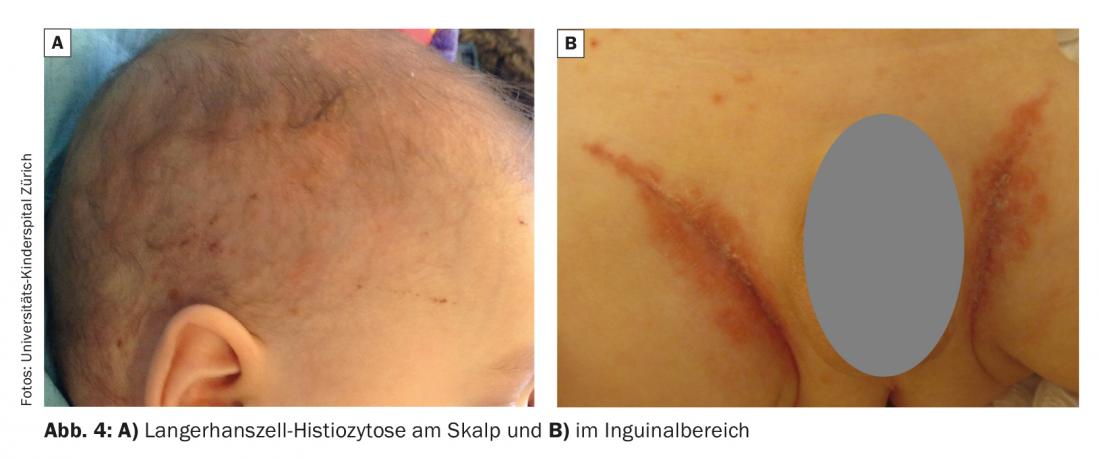
Langerhans cell histiocytosis is a rare neoplasm that usually occurs in the first 3 years of a child’s life. Skin manifestations present similarly to seborrheic eczema with papules in the scalp area as well as the inguinal region (Fig. 4 A+B) . Indicative of the diagnosis are brownish, typically crusted papules, although these may be discrete. In addition, erosions and even ulcerations often occur, especially in the inguinal region. If suspected, a rapid skin biopsy will provide diagnostic clarity.
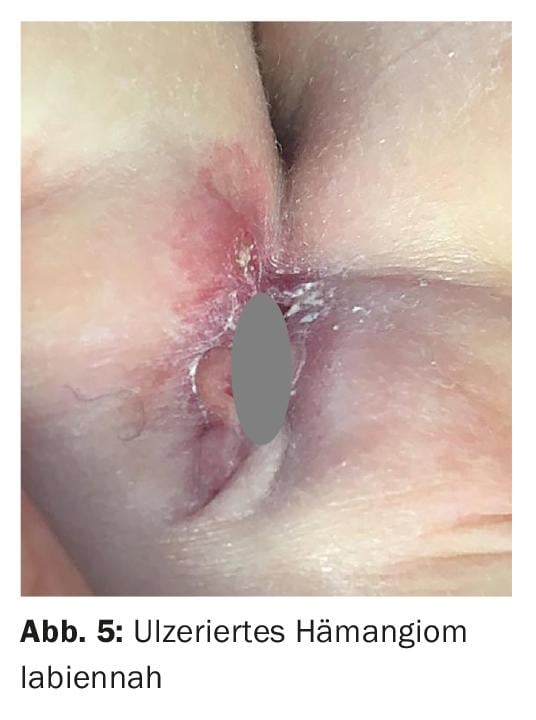
e. Ulcerated infantile hemangioma
Infantile hemangiomas are the most common benign tumor of infancy and occur in up to 5% of all children. They are often problematic in the diaper area because they tend to ulcerate. These ulcerations can occur so early that it is sometimes difficult to even identify the causative hemangioma. In particular, the appearance of a unilateral ulceration should raise the possibility of an infantile hemangioma and search for it accordingly (Fig. 5) . In addition to adequate wound care, systemic treatment with propranolol is indicated in this situation.
Proper care of the genital area in diaper dermatitis and prevention.
The treatment of diaper dermatitis aims, on the one hand, to stabilize and regenerate the affected skin and prevent a flare-up. Regular bathing of the affected child as part of general skin care is also central to the prevention of diaper dermatitis [12]. With diaper dermatitis, as with many other diseases, the earlier it is treated, the better. Special attention should be paid to the education of parents – especially in the case of a severe course or repeated occurrence.
The ABCDE principle summarizes the most important measures of care in diaper dermatitis, [2] and can be a guide in everyday life:
A = Air: Occlusion under the diaper results in increased hydration to maceration of the stratum corneum. When changing diapers regularly, always make sure to leave the diaper off for a period of time. It should be remembered that children who do not wear diapers do not develop diaper dermatitis [4].
B = Barriers: Barrier creams are widely used for skin care in the genital region and for the prevention of diaper dermatitis. Barrier creams support the skin barrier function and have a stabilizing effect on the stratum corneum. The use of barrier creams after the regular baby bath is also recommended twice a week for healthy, intact skin [14].
C = Cleansing & Care: More frequent diaper changes, regular and regular skin care and cleansing of the skin are recommended preventively and are indispensable in the treatment. The bath is superior to washing, as more gentle on the skin. The diaper area should be cleaned regularly with alkali-free preparations. Subsequently, consistent drying of the affected skin areas without mechanical irritation is central. Oil can be used for gentle cleansing, but should be removed before reapplying the diaper. Oil can burn on damaged skin and promote fungal growth. Always controversial are the recommendations for the use of baby wipes. Baby wipes have a very soft non-woven texture, which makes them superior for use on sensitive-already irritated and damaged skin. Dry baby wipes such as diaper pads or cotton pads are unsuitable for damaged skin [13]. Baby wipes should be free of irritants such as alcohol, fragrances, oils, detergents and potentially toxic preservatives [2]. Zinc oxide has been shown to be particularly effective in treating redness and sores in the diaper area. This substance has an antiseptic effect and dries weeping wounds. It is best to apply a thin layer of a cream paste containing zinc oxide after bathing and at each diaper change. Ideal is a cream paste that protects the skin from moisture and mechanically from friction, but does not increase the occlusion and can be gently removed. If the rash does not improve after two to three days, mild topical corticosteroids may be used for a few days. In addition, any superinfection should be adequately treated. For recurrent diaper dermatitis or when trigger factors (e.g., intestinal disease) cannot be resolved, longer-term use of topical calcineurin inhibitors may be helpful.
D = Diaper: Disposable diapers with superabsorbent are clearly superior to reusable diapers. Due to the super absorbent polymers, the moisture is quickly absorbed. Reusable diapers lack this superabsorber, the texture of the fabric is much rougher and therefore the skin is always additionally irritated by the constant moisture of the fabric and friction. The disposable diapers ideally adapt to the fit due to the elastic texture and thus friction is additionally minimized. Occlusion may favor diaper dermatitis that has already flared up. It is therefore imperative to change disposable diapers regularly despite their high absorbency.
E = Education: here, the focus is on educating parents about the pathogenesis of diaper dermatitis [4], and it also involves instructing parents to perform the care measures on their child themselves and to recognize risk factors [4].
|
A brochure for information and education for parents, which can be used for free, can be found here: www.kispi.uzh.ch/de/patienten-und-angehoerige/Broschueren/Seiten/default.aspx |
Take-Home Messages
- Diaper dermatitis is a common condition in infants and incontinent persons, which is directly related to the wearing of a diaper. It heals without complications in most cases.
- Symptoms correspond to those of acute to subacute eczema and include erythematous macules, papules, plaques, and, in more severe cases, erosions and even ulceration. Due to the pathogenesis, primarily the convex skin areas in direct contact with the diaper are affected, whereas the flexures are free, at least initially.
- Taking good care of the genital area is effective in preventing diaper dermatitis and essential in treating it. Regular baby bath is suitable for this and gentle. Treatment must be given at an early stage. Regular, frequent diaper changes are essential.
Literature:
- Blume-Peytavi U, Hauser M, Lussemann L, et al: Preventaion of diaper dermatitis in infants – a literature review. Pediatric Dermatology 2014; 31: 413-429.
- Blume-Peytavi U, Kanti V: Prevention and treatment of diaper dermatitis. Pediatric Dermatology 2018; 35: 19-23.
- Odio M, Thalmann L: Diapering, diaper technology and diaper area skin health. Pediatr Dermtolo 2014; 31 (suppl): 9-14.
- Höger, PH; Kinderdermatologie, Differenzialdiagnostik und Therapie bei Kindern und Jugendlichen, 3rd edition, Schattauer, Stuttgart 2011.
- Atherton DJ: Understanding irritant napkin dermatitis. Int J Dermatol 2016; 55 (suppl): 7-9.
- Merrill L: Prevnetion, treatment and parent education for diaper dermatitis. Nurs Women Health 2015; 19: 324-336.
- van Gysel D.: Infections and skin diseases mimicking diaper dermatitis. International Journal of dermatology 2016; doi: 10.1111/ijd.13372.
- Fölser-Holst R: Differential diagnosis of diaper dermatitis. Pediatr Dermatol 2018; 35: 10-18.
- Counts J, Weisbrod A, Yin S: Common diaper ingredient questions: modern disposable diaper materials are safe and extensively tested. Clin Pediatr 2017; 56 (5): 23S-27S.
- Smith WJ, Jacob SE: The role of allergic contact dermatitis in diaper dermatitis. Pediatrc Dermatol 2009; 26: 369-370.
- Roul S, Ducombs G, Leaute-Labreze C, Taïeb A: “Lucky Luke” contact dermatitis due to rubber components of diapers. Contact Dermatitis 1998 Jun; 38(6): 363-364; doi: 10.1111/j.1600-0536.1998.tb05796.x.
- Blume-Peytavi U, Garcia Bartels N: Skin care in infancy – on the influence of standardized care regimes on skin barrier function. Current Derm 2010; 36: 214-216.
- Lavender T, Furber C, Campbell M, et al: Effect on skin hydration of using baby wipes to clean the napkin area of newborn babies: assesor-blinded randomised controlled equivalence trial, BMC Pediatr 2012; 12: 59.
- Blume-Peytavi U, Lavender T, Jenerowicz D, et al: Recommendations from a European Roundtable Meeting on Best Practice Healthy Infant Skin Care. Pediatr. Dermatol 2016; 33(3): 311-321; doi: 10.1111/pde.12819.
DERMATOLOGY PRACTICE 2020; 30(6): 8-12