Approximately 60 per 1000 population undergo abdominal surgery annually. The majority of patients are initially evaluated and triaged in the primary care physician’s office. Visceral surgery is also constantly evolving, and many recent studies focus on robotic-assisted surgery as well as prognosis improvement in tumor patients.
Approximately 60 per 1000 population undergo abdominal surgery annually [1]. The majority of patients are initially evaluated and triaged in the primary care physician’s office. Visceral surgery is also constantly evolving, and many recent studies focus on robotic-assisted surgery as well as prognosis improvement in tumor patients. We present here an update on visceral surgery with special attention to aspects relevant or of interest to family practice.
Since this is an extensive area, we have split the update into two parts. In Part 1, we first describe the upper gastrointestinal tract and gastrointestinal complications in COVID-19. Another article in the upcoming issue will discuss the lower gastrointestinal tract as well as parietology and perioperative medicine.
Methodology
Literature from 2019 and 2020 was searched for thematic relevance. Searches were conducted via Pubmed (www.pubmed.gov) and UpTo-Date (www.uptodate.com/contents/search) for the following subcategories: Upper Gastrointestinal Tract, Bariatric, Hepatobiliary and Pancreatic Surgery, and Gastrointestinal Complications of COVID-19.
Esophageal Cancer
Esophageal cancer is one of the most aggressive gastrointestinal cancers. The standard operation is open abdomino-thoracic esophagectomy according to Ivor Lewis. Because of the comparatively high postoperative morbidity and limited quality of life, minimally invasive procedures in particular have been investigated in recent years. In the short term, better results were achieved with regard to postoperative pneumonia, wound infections, and sepsis. Due to the complexity of the surgery, it should be performed at a center with appropriate expertise [2]. Which endoscopic surgical techniques will become state of the art in the future is still under discussion.
Gastric Cancer
A retrospective Dutch study demonstrated that center expertise in gastric cancer patients had a significant impact on long-term patient survival. According to this study, a minimum number of cases per hospital and year required for this purpose was set at 21 cases [3]. Intensive discussions on minimum case numbers in highly specialized medicine (HSM visceral surgery) are also underway in Switzerland.
Despite the possibility of treating mucosal carcinomas (T1) by endoscopic resection, these are associated with a high risk of metastasis in undifferentiated tumors and should primarily be submitted to surgery [4]. If the affected patients find access to surgery delayed, one is therapeutically confronted with more complicated situations such as scarring or recurrence.
In selected patients with early gastric carcinoma, minimally invasive partial gastric resection with locoregional sentinel lymphadenectomy is occasionally a therapeutic option with lower morbidity and the same oncologic outcome [5,6].
Reflux disease
Nearly 20% of the population suffers from gastroesophageal reflux symptoms (Fig. 1) . These are primarily treated with proton pump inhibitors (PPI). Surgery is used for PPI-refractory or reflux-associated chest pain, with fundoplicatio achieving 16% better reflux control than the drug comparison group [7].
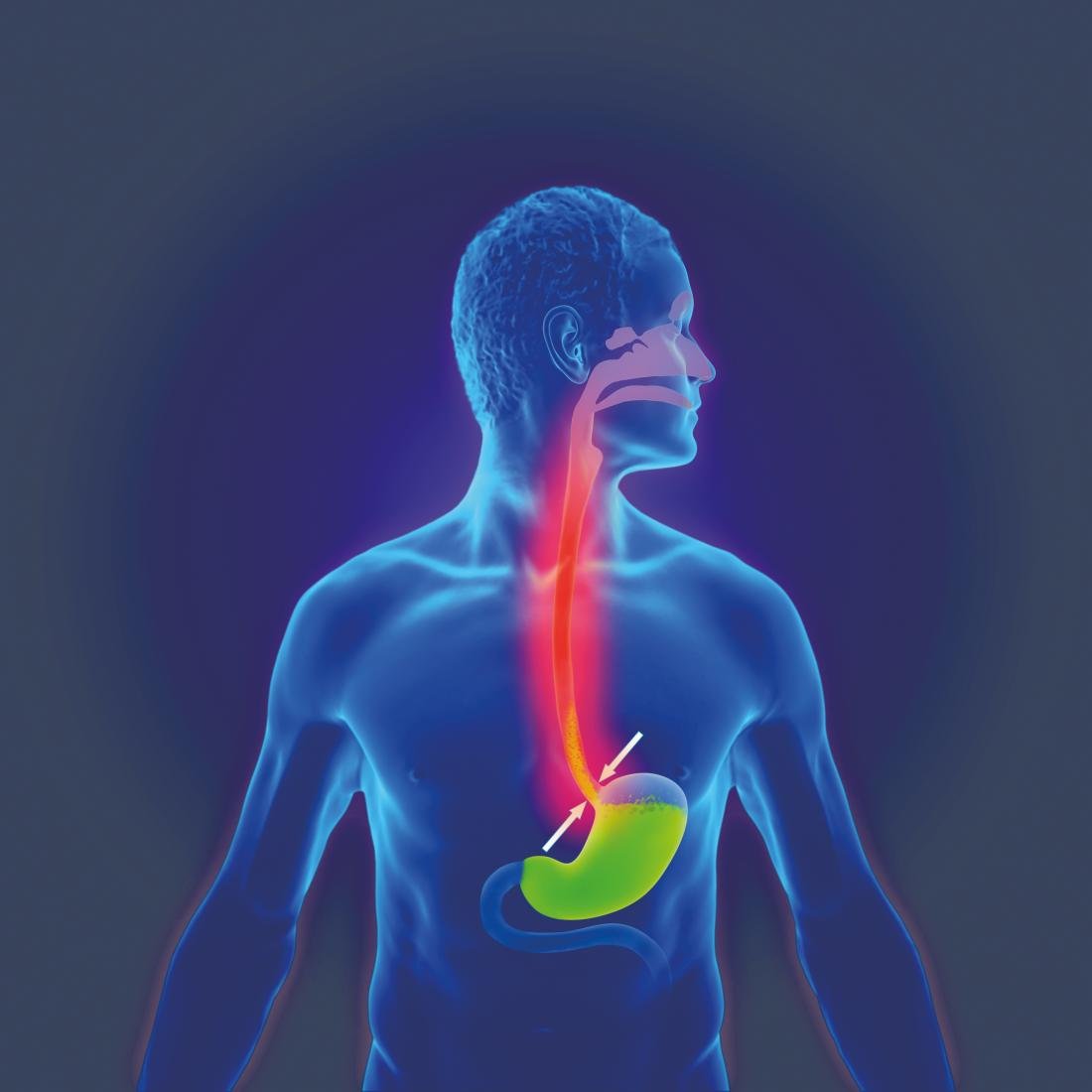
The slightly less invasive magnetic band implantation as a propagated alternative to fundoplicatio continues to be discussed in studies, but cannot be recommended as a real alternative due to lack of long-term data as well as lack of direct comparison with fundoplicatio [8].
Bariatric surgery
The risk of mortality increases with increasing BMI; for example, patients with a BMI greater than 50 kg/m² have a threefold increased risk of dying from cardiovascular, renal, or malignant sequelae [9]. Physical activity and dietary changes often result in a yo-yo effect, which is why surgery is the best option for long-term weight loss and increased life expectancy. This can extend the lifetime by up to 3 years [10]. The standard procedures remain Roux-Y gastric bypass and gastric tube formation. Higher weight losses as well as diabetes remissions can be achieved after Roux-Y gastric bypass [11,12]. The positive effects on diabetes mellitus are mainly due to weight loss. The effects on insulin sensitivity, beta-cell function as well as insulin profile are identical compared to dietary weight loss [13]. In an American study, bariatric surgery was shown to lower the risk of malignancies such as breast cancer, endometrial cancer, and colon cancer, especially in women [14]. Gastroesophageal reflux disease is a significant late complication, especially after sleeve gastrectomy, which is why preoperative reflux workups and regular gastroscopies are recommended postoperatively [15].
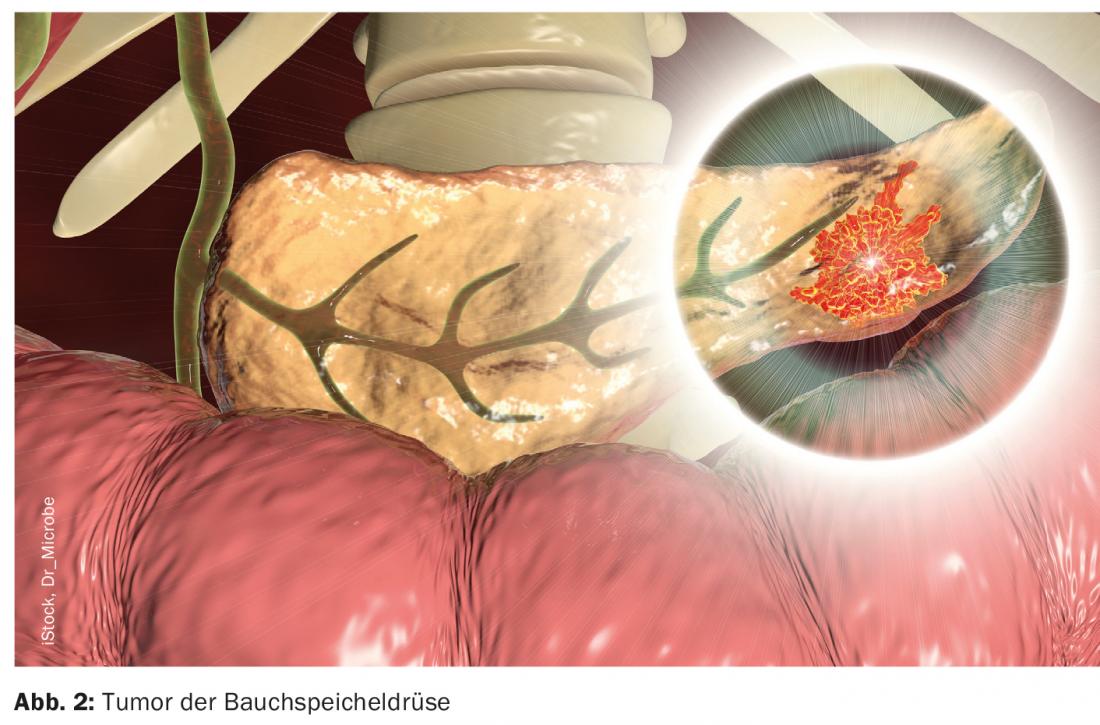
Pancreatic tumors
Minimally invasive surgical techniques are equal to open procedures in terms of surgical technique and radicality in appropriate cases of distal pancreatectomy. In terms of quality of life and postoperative delayed gastric emptying, minimally invasive procedures are superior to open procedures; a disadvantage is the high rate of postoperative pancreatic fistulas [16].
According to recent studies, neoadjuvant chemotherapy seems to have a positive impact on tumor biology and pancreatic fistula rates. This is likely due to fibrosis of the pancreatic tissue, resulting in harder tissue and reducing the rate of anastomotic insufficiency. The trend is clearly toward neoadjuvant therapy, and in selected patients neoadjuvant therapy should be considered today [17] (Fig. 2). Adjuvant therapy must be given without a long time delay. The mFOLFIRINOX regimen continues to be the standard of care, although this chemotherapy may not always come to fruition depending on the general condition of the patient [18,19]. Studies are also ongoing in the surgery of singular metastases after curative pancreatic cancer surgery. Metachronous single metastases in the lung may be submitted to curative metastasectomy in special cases, and solitary liver metastases are also discussed. The decision to do so must be made on an interdisciplinary basis at a tumor board [20].
Pancreatitis
Biliary obstruction is the most common cause of acute pancreatitis in Europe [21]. Cholecystectomy as therapy as well as prophylaxis of recurrent pancreatitis is the gold standard. A systematic literature review confirmed early selective cholecystectomy as a safe therapeutic approach in patients with mild pancreatitis during the initial stay [22]. In chronic pancreatitis, in which pain in particular, but also parenchymal destruction, is the main concern, surgery offers a good chance of long-term reduction of symptoms, reduced pancreatic tissue destruction and improved quality of life [23,24]. In this context, early referral to surgery is important in the absence of sustained therapeutic success of other (interventional) procedures.
Gall bladder and biliary tract disease
Bile duct injury is a feared complication after cholecystectomy. Especially in acute cholecystitis, the risk was considered to be increased and surgery was performed accordingly only in the inflammation-free interval (Fig. 3). However, according to current data, early cholecystectomy in acute cholecystitis does not show any differences in terms of morbidity [25].

Hepatocellular carcinoma
Hepatocellular carcinoma is the most common primary liver tumor. In early stages, surgical resection is an option in addition to local ablative procedures. A retrospective case-control study from 2019 demonstrated a significant benefit for surgical resection in terms of survival. Crucial for this is the operability of the patient with appropriate residual liver function [26].
Liver metastases
In colorectal liver metastases, especially at stage T3/T4 of the primary tumor, contrast-enhanced ultrasound (CEUS) detected liver metastases in up to 4% of all patients. CEUS is recommended as primary imaging after CT-graphically detected liver lesions [27]. In cases of extensive liver metastasis, hypertrophy concepts such as the ALPPS procedure (Associating Liver Partition and Portal vein Ligation for Staged hepatectomy) and other “staged” hepatectomy procedures remain in the forefront. Postoperative liver failure after resection could be reduced, but corresponding procedures are associated with -high perioperative morbidity and should be performed only in selected patients and appropriate centers [28].
Gastrointestinal complications of COVID-19.
Since the onset of corona pandemic, several extrapulmonary illnesses have been observed. These include ileus, intestinal ischemia, pancreatitis, or liver dysfunction [29]. Causally, the focus is on the increased expression level of angiotensin-converting enzyme 2 receptor in intestinal epithelial cells, which serve as receptors for SARS-CoV-2 [30].
Coronavirus-induced coagulopathy, as well as increased opioid requirements, may explain the increased intestinal ischemia, but also the high ileus rates [31]. Therefore, in corona-positive pa-tients with abdominalgia, surgical pathology should be considered because of the concomitant diseases. Conversely, covid-19 infection must be included in the differential diagnosis for otherwise unexplained abdominal problems.
Concerns have been expressed repeatedly that patients will visit health care facilities later or not at all during the pandemic. This may be due to quarantine measures, other restrictions, or fear of infection in the hospital. As an indication, the proportion of severe appendicitis in the pandemic was shown to have significantly increased to 92% (prevalence 57.1%; p=0.003) [32]. A noted 2-day delay in medical care was also referred to as collateral damage of the pandemic [33]. The total number of emergency abdominopelvic computed tomography scans decreased significantly in emergency departments during the pandemic, and significantly fewer acute diverticulitis were diagnosed. One possible interpretation for this is that patients with less highly acute conditions were hospitalized less frequently overall [34].
In tumor patients, in addition to the general mortality risk due to tumor disease, there is also increased lethality from SARS-CoV-2 infection. Physicians must balance the risk -of-delayed malignancy therapy with the patient’s risk of exposure to SARS-CoV-2 infection. Several studies have described the incidence regarding corona infection of less than 5% in tumor patients, which definitely does not justify delayed malignancy therapy [35,36].
Take-Home Messages
- In abdominal tumor surgery, there is a clear trend toward center surgery, which is also increasingly supported by robust data with better outcomes.
- Bariatric surgery is the best therapeutic option with regard to cardiovascular, renal, or malignant obesity-associated sequelae.
- Neoadjuvant chemotherapy in pancreatic cancer can have a favorable impact on tumor biology and surgical outcome.
- For chronic pancreatitis, surgery offers more long-term pain relief, decreased pancreatic tissue destruction, and improved quality of life.
- During the corona pandemic, increased abdominal illnesses, such as ileus, intestinal ischemia, pancreatitis, and others, were also observed.
- In abdominalgia, corona infection should be considered as a differential diagnosis.
Part 2 in HAUSARZT PRAXIS 2/21
Literature:
- Swiss Federal Statistical Office – Hospital Medical Statistics (MS); www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/erhebungen/ms.assetdetail.7369.html.
- Yoshida N, et al: Can Minimally Invasive Esophagectomy Replace Open Esophagectomy for Esophageal Cancer? Latest Analysis of 24,233 Esophagectomies From the Japanese National Clinical Database. Ann Surg 2020; 272: 118-124.
- Claassen YHM, et al: Effect of Hospital Volume With Respect to Performing Gastric Cancer Resection on Recurrence and Survival: Results From the CRITICS Trial. Ann Surg 2019; 270: 1096–1102.
- Lin JX, et al: Risk factors of lymph node metastasis or lymphovascular invasion for early gastric cancer: a practical and effective predictive model based on international multicenter data. BMC Cancer 2019; 19: 1048.
- Yu J, et al: Effect of Laparoscopic vs Open Distal Gastrectomy on 3-Year Disease-Free Survival in Patients With Locally Advanced Gastric Cancer: The CLASS-01 Randomized Clinical Trial. JAMA 2019; 321: 1983.
- Lee HJ, et al: Short-term Outcomes of a Multicenter Randomized Controlled Trial Comparing Laparoscopic Distal Gastrectomy With D2 Lymphadenectomy to Open Distal Gastrectomy for Locally Advanced Gastric Cancer (KLASS-02-RCT). Ann Surg 2019; 270: 983-991.
- Spechler SJ, et al: Randomized Trial of Medical versus Surgical Treatment for Refractory Heartburn. N Engl J Med 2019; 381: 1513-1523.
- Guidozzi N, et al: Laparoscopic magnetic sphincter augmentation versus fundoplication for gastroesophageal reflux disease: systematic review and pooled analysis. Dis Esophagus 2019.
- Moussa OM, et al: Mortality of the Severely Obese: A Population Study. Ann Surg 2019; 269: 1087-1091.
- Carlsson LMS, et al: Life Expectancy after Bariatric Surgery in the Swedish Obese Subjects Study. N Engl J Med 2020; 383: 1535-1543.
- Poelemeijer YQM, et al: Gastric Bypass Versus Sleeve Gastrectomy: Patient Selection and Short-term Outcome of 47,101 Primary Operations From the Swedish, Norwegian, and Dutch National Quality Registries. Ann Surg 2020; 272: 326-333.
- Hofsø D, et al: Gastric bypass versus sleeve gastrectomy in patients with type 2 diabetes (Oseberg): a single-centre, triple-blind, randomised controlled trial. Lancet Diabetes Endocrinol 2019; 7: 912-924.
- Yoshino M, et al: Effects of Diet versus Gastric Bypass on Metabolic Function in Diabetes. N Engl J Med 2020; 383: 721-732.
- Schauer DP, et al: Bariatric Surgery and the Risk of Cancer in a Large Multisite Cohort: Ann Surg 2019; 269: 95-101.
- Yeung KTD, et al: Does Sleeve Gastrectomy Expose the Distal Esophagus to Severe Reflux: A Systematic Review and Meta-analysis. Ann Surg 2020; 271: 257-265.
- de Rooij T, et al: Minimally Invasive Versus Open Distal Pancreatectomy (LEOPARD): A Multicenter Patient-blinded Randomized Controlled Trial. Ann Surg 2019; 269: 2-9.
- Hank T, et al: Association Between Pancreatic Fistula and Long-term Survival in the Era of Neoadjuvant Chemotherapy. JAMA Surg 2019; 154: 943.
- Conroy T, et al: FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N Engl J Med 2018; 379: 2395-2406.
- Michael N, et al: Timing of palliative care referral and aggressive cancer care toward the end-of-life in pancreatic cancer: a retrospective, single-center observational study. BMC Palliat Care 2019; 18: 13.
- Ilmer M, et al: Oligometastatic pulmonary metastasis in pancreatic cancer patients: safety and outcome of resection. Surg Oncol 2019; 31: 16-21.
- Zilio MB, et al: A systematic review and meta-analysis of the aetiology of acute pancreatitis. HPB 2019; 21: 259-267.
- Moody N, et al: Meta-analysis of randomized clinical trials of early versus delayed cholecystectomy for mild gallstone pancreatitis. BJS 2019; 106: 1442-1451.
- Löhr JM, et al: United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United Eur Gastroenterol J 2017; 5: 153-199.
- Ahmed Ali U, et al: Endoscopic or surgical intervention for painful obstructive chronic pancreatitis. Cochrane Database Syst Rev 2015; 3: CD007884.
- Mytton J, et al: Outcomes Following an Index Emergency Admission With Cholecystitis: A National Cohort Study. Ann Surg 2019; Publish Ahead of Print.
- Lee GC, et al: Surgical resection versus ablation for early-stage hepatocellular carcinoma: A retrospective cohort analysis. Am J Surg 2019; 218: 157-163.
- Sawatzki M, et al: Contrast-enhanced ultrasound can guide the therapeutic strategy by improving the detection of colorectal liver metastases. J Hepatol 2020; S0168827820336825.
- Jiao L, et al: Rapid Induction of Liver Regeneration for Major Hepatectomy (REBIRTH): A Randomized Controlled Trial of Portal Vein Embolisation versus ALPPS Assisted with Radiofrequency. Cancers 2019; 11: 302.
- El Moheb M, et al: Gastrointestinal Complications in Critically Ill Patients With and Without COVID-19. JAMA 2020; 324: 1899.
- Qi F, et al: Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses. Biochem Biophys Res Commun 2020; 526: 135-140.
- Levi M, et al: Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol 2020; 7: e438-e440.
- Romero J, et al: Acute Appendicitis During Coronavirus Disease 2019 (COVID-19): Changes in Clinical Presentation and CT Findings. J Am Coll Radiol 2020; 17: 1011-1013.
- Masroor S: Collateral damage of COVID-19 pandemic: Delayed medical care. J Card Surg 2020; 35: 1345-1347.
- Gibson AL, et al: Impact of the COVID-19 pandemic on emergency department CT for suspected diverticulitis. Emerg Radiol 2020; 27: 773-780.
- Yu J, et al: SARS-CoV-2 Transmission in Patients With Cancer at a Tertiary Care Hospital in Wuhan, China. JAMA Oncol 2020; 6: 1108-1110.
- Lewis MA: Between Scylla and Charybdis – Oncologic Decision Making in the Time of Covid-19. N Engl J Med 2020; 382: 2285-2287.
HAUSARZT PRAXIS 2021; 16(1): 4-7











