One of the most important decisions that must be made at the onset of symptomatic myeloma is that of adequate therapy. While not yet curable, a number of good options exist that can delay progression. Based on intensive research and better understanding of the pathophysiology, effective treatment options could be added to chemotherapy.
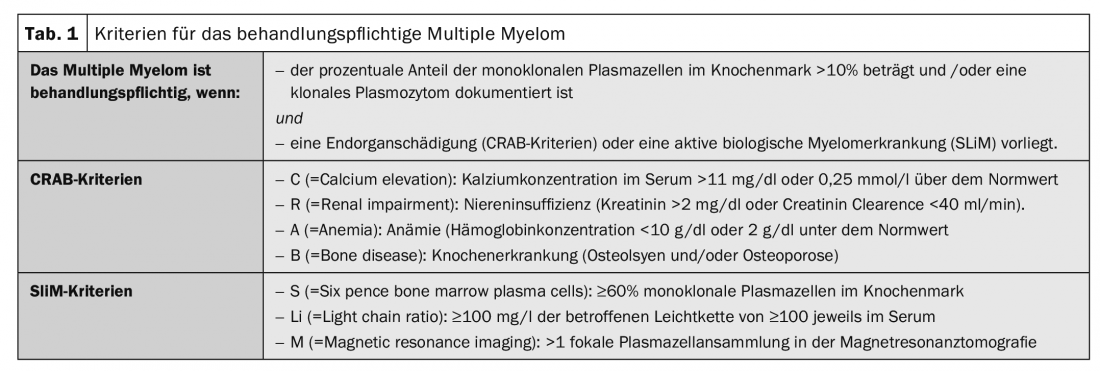
Not all multiple myeloma requires therapy from the outset. If there are no clinical signs yet, the patient can be closely monitored and observed for the time being. However, as soon as bone changes become apparent, for example, effective treatment is indicated. Symptomatic disease is present when the CRAB criteria are met: C = elevated blood calcium concentration (hypercalcemia), R = renal dysfunction (renal insufficiency), A = anemia, B = bone destruction ( Table 1) . In order to decide on a suitable therapy regime, staging and prognostic classification are essential. The goal is to improve myeloma symptomatology, lower M protein, and thus control the disease.
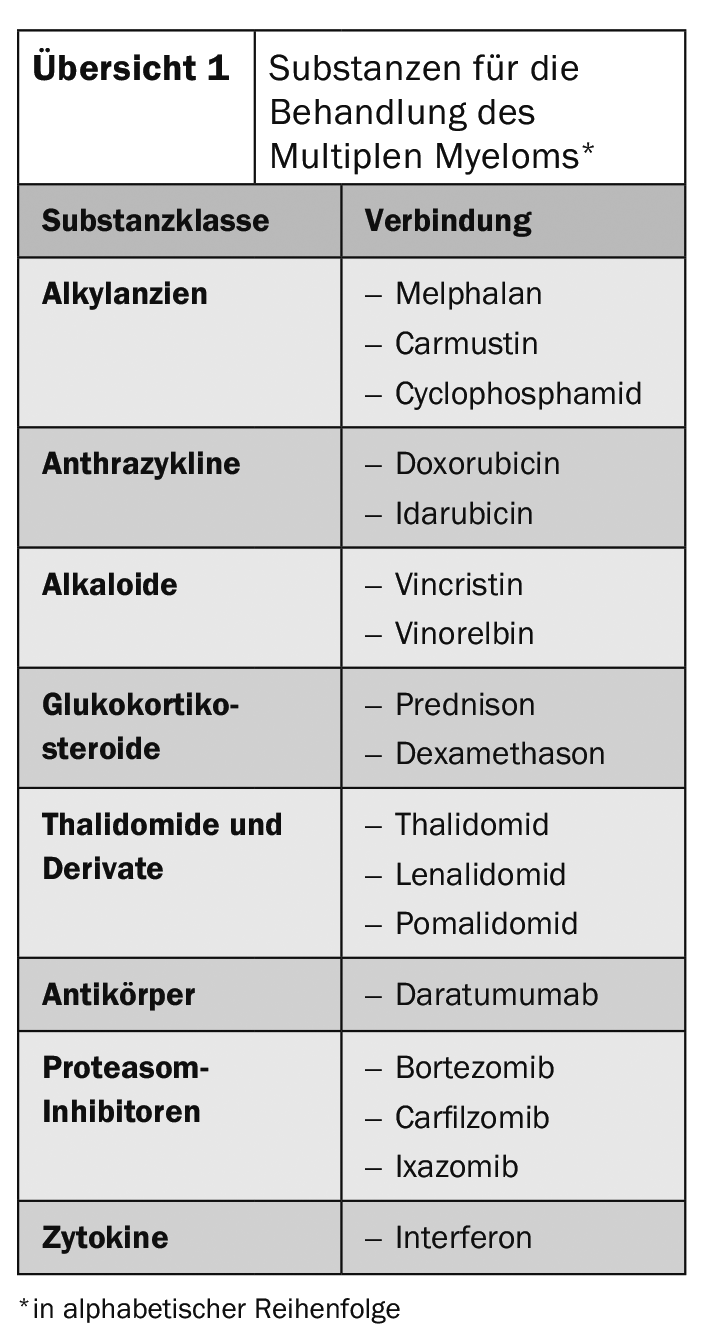
The various therapeutic approaches are based on conventional chemotherapy, high-dose chemotherapy with autologous blood stem cell transplantation, and newer substances such as bortezomib, lenalidomide, thalidomide, or antibodies (overview 1) . In order to achieve the greatest possible effect against the tumor cells during chemotherapy and at the same time reduce side effects, combinations of cytostatic drugs with different effects are frequently used. However, high-dose chemotherapy with autologous stem cell transplantation is the treatment of choice for patients up to about 70 years of age. Success also depends on the choice of treatment before and after chemotherapy. A combination of the two most important substance classes, proteasome inhibitors and immunomodulators, seems promising for this purpose.
Established and effective
Thalidomide, bortezomib, lenalidomide have already been shown to be effective in multiple therapeutic regimens, although thalidomide is now rarely used. As a proteasome inhibitor, bortezomib has a high response rate in primary and relapse therapy. Among other things, it blocks the activation of certain signaling pathways as well as DNA repair mechanisms in the myeloma cell so that the cells’ resistance to cytostatic drugs can be overcome. As a triple combination, bortezomib is often used with dexamethasone and cyclophosphamide. Lenalidomide belongs to the group of immunomodulators. It impairs the release of pro-inflammatory substances and increases the production of anti-inflammatory substances.
For the treatment of elderly patients >70 years or sufferers with many comorbidities, the only option for a long time was a combination therapy of melphalan and prednisone. A significant improvement in efficacy was achieved by adding bortezomib. This combination resulted in a significant improvement in the prognosis of affected patients compared with MP. Recent results suggest that an extension of this treatment regimen to include an antibody could lead to further improvement in therapeutic outcomes.
Further reading:
- https://multiples-myelom.ch/de/multiples-myelom/therapien/ (last accessed on 05.08.2020)
- https://lymphome.de/multiples-myelom/therapie/ (last accessed on 05.08.2020)
- www.myelom-deutschland.de/das-multiple-myelom/therapie-des-multiplen-myeloms (last accessed on 05.08.2020)
- www.krebsgesellschaft.de/onko-internetportal/basis-informationen-krebs/krebsarten/multiples-myelom-plasmozytom-morbus-kahler/therapie.html (last accessed on 05.08.2020)
InFo ONCOLOGY & HEMATOLOGY 2020; 8(4): 16.