Lipid-lowering agents have been used for years for both primary and secondary prevention of cardiovascular disease. Statins, which can significantly lower both total and LDL cholesterol, play a central role. Current European guidelines now advocate even stricter LDL-C lowering.
An elevated cholesterol level is considered to be the main risk factor for the development of arteriosclerosis. However, this also increases the risk of cardiovascular events [1]. Studies have demonstrated that the incidence of cardiovascular events decreases with the reduction of LDL cholesterol levels [2]. Since atherosclerosis is an inflammatory process, it is obvious to use anti-inflammatory and antioxidant drugs for vascular prevention. Therefore, when lifestyle changes involving a change in diet and increased exercise are not enough, statins are usually used. Their lipid-lowering effect occurs via inhibition of HMG-CoA reductase, the key enzyme in cholesterol biosynthesis. This inhibition results in decreased formation of LDL cholesterol with concomitant increased expression of hepatic LDL receptors [3]. Dyslipidemia is characterized by an elevated plasma cholesterol and/or triglyceride (TG) concentration or a low HDL level in the blood. In primary dyslipidemia, there is a genetic predisposition. Secondary dyslipidemia can be triggered by:
- Physical inactivity lifestyle
- Excessive intake of saturated fatty acids, cholesterol and trans fats
- Diabetes mellitus
- Alcohol abuse
- Chronic kidney disease
- Hypothyroidism
- Primary biliary cirrhosis
- Drugs (especially beta-blockers, thiazide diuretics, retinoids, cyclosporine, tacrolimus, estrogen, glucocotricoids)
Lipid determination and risk stratification
In addition to the survey of cardiovascular risk factors, a measurement of serum lipids is performed. The current European guideline recommends the determination of HDL-C, LDL-C, TC, TG, non-HDL, ApoB, and Lp(a) [4]. Risk calculation scores (PROCAM, SCORE, ARRIBA) can be used for individual risk stratification, which forms the basis for the therapy regime. In addition to the laboratory parameters, information on gender, age, smoking habits and systolic blood pressure are also included in the assessment. The LDL-C target value is based on the patient’s determined risk (Table 1).

Numerous study results have led to new evidence-based findings in recent years. For example, it has been shown that the lower the LDL-C level achieved, the lower the risk of future cardiovascular events – without very low LDL-C levels representing an increased risk. Therefore, the guideline advocates consistent and efficient lipid modification with the goal of very low LDL-C levels.
Prevention as the main indication
The main indication for the treatment of dyslipidemia is the prevention of atherosclerotic cardiovascular disease. Therapy is also indicated in patients with coronary artery disease. Lowering LDL cholesterol in CHD patients is associated with a slowing of atherosclerosis and reduction of cardiovascular events and lethality.
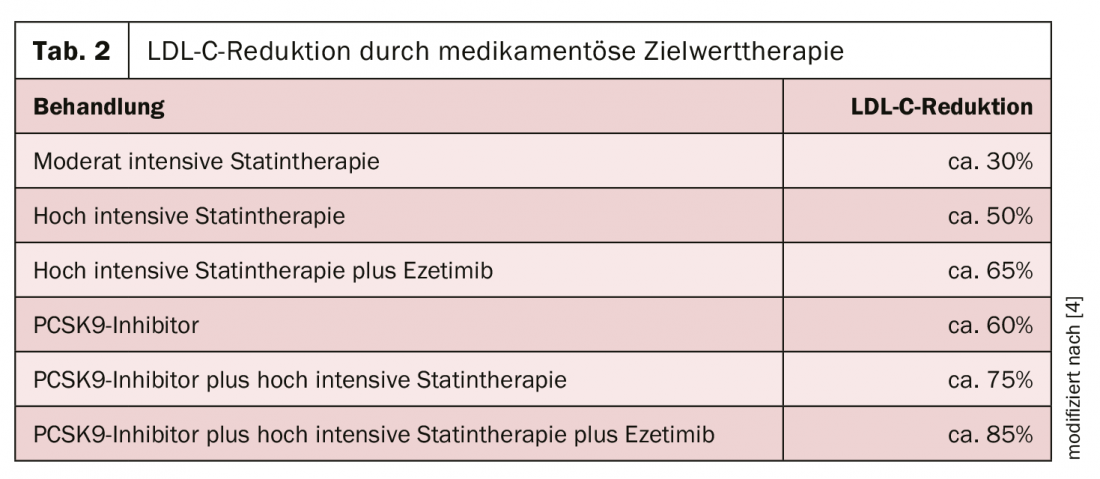
Nonpharmacologic interventions include dietary adjustment, weight reduction, regular physical exercise, and tobacco and alcohol cessation. Pharmacologically, statins (e.g., atorvastatin, lovastatin, pravastatin), cholesterol resorption inhibitors (ezetimibe), bile sorbents (cholestyramine, cholestipol), and PCSK9 inhibitors (e.g., evolocumab, alirocumab) are available. To achieve the individual risk level, high-potency statins should be used primarily up to the highest tolerated dose. If the target values are not reached by the use of a statin, a combination of statin and ezetimibe is recommended. If this treatment regimen is still not sufficient in the case of high or very high risk, the further addition of a PCSK9 inhibitor is conceivable (Table 2) [4].
Although statins are usually very well tolerated, they can have adverse effects, such as muscle symptoms, negative effects on the liver and kidneys, a slightly increased risk of diabetes mellitus, and for osteoporosis. It should also be kept in mind that most preparations are metabolized via the CYP3A4 and CYP2C9 isoenzymes of the cytochrome P450 system. Therefore, interactions may occur with grapefruit juice or agents such as fibrates, ciclosporin, or HIV/hepatitis C protease inhibitors, among others.
Literature:
- Ference BA, Ginsburg HN, Graham I, et al: Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. evidencefromgenetic, epidemiologic, andclinicalstudies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J 2017; 38: 2459-2472.
- Boekholdt SM, HovinghGK, Mora S, et al: Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: a meta-analysis of statin trials. J Am Coll Cardiol 2014; 64: 485-494.
- www.amboss.com/de/wissen/Lipidsenker (last accessed on 24.02.2020)
- Mach F, Baigent C, Catapano AL, et al: 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020; 41(1): 111-188.
CARDIOVASC 2020; 19(1): 20-21