According to the new EAN guidelines, paroxysmal disorder caused by neurovascular compression should be diagnosed by MRI. Neurovascular contact (NVC) should be used only with regard to possible surgery, not to confirm diagnosis. Carbamazepine and oxcarbazepine are recommended for first-line prophylactic treatment.
Trigeminal neuralgia (TN) is defined as a flashing, extremely sharp, electrifying and stabbing pain in the area supplied by one or more trigeminal branches. The attacks usually last a few seconds, but in rare cases can last up to two minutes. They are often triggered by speech, other mouth movements or touch in the area supplied by the trigeminal nerve, but can also occur spontaneously. A distinction is made between idiopathic and symptomatic trigeminal neuralgia. While patients with an idiopathic form are usually pain-free between attacks, those with a symptomatic form are not and there is often, but not regularly, a sensory deficit in the affected trigeminal branch.
The new EAN guideline answers the top ten questions patients and pain specialists face when managing TN. The new classification includes three categories: idiopathic TN (no NVC or NVC without morphologic changes in the trigeminal root), classic TN (resulting from neurovascular compression with morphologic changes in the trigeminal root), and secondary TN (resulting from severe neurologic disease such as multiple sclerosis). Patients with secondary TN generally appear to be younger and more likely to have trigeminal sensory deficits and bilateral pain.
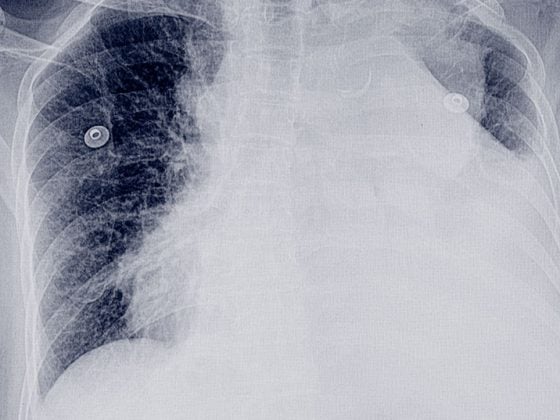
MRI supports clinical diagnosis
A correct diagnosis is essential and should be based on clinical features as described in the latest classification system. MRI is necessary to rule out secondary causes of TN such as tumors and multiple sclerosis. Specific imaging protocols have been developed to determine whether the trigeminal nerve root is compressed by one or more blood vessels. Evidence of neurovascular contact should not be used to confirm the diagnosis of TN but should be used to guide decisions about possible surgery.
Long-term treatment with antiepileptic drugs
First-line treatment of TN is pharmacologic. The use of opioids is not usually effective for acute pain episodes in patients with TN. Acute pain episodes may require hospital admission for rehydration and intravenous infusion and titration of antiepileptic drugs. Long-term treatment is based on antiepileptic drugs, with carbamazepine and oxcarbazepine being first-line drugs. It is important that patients be accompanied by pain specialists who can advise them on how to titrate the dosage of medications according to effect and side effects. Patients should be offered surgery if their pain is not adequately controlled medically or if medical treatment is poorly tolerated. Surgical options include microvascular decompression, in which the blood vessel is moved, and various procedures in which the trigeminal nerve is partially destroyed. Microvascular decompression is recommended as first-line surgery when the nerve is compressed by a blood vessel.
Source: 5th Congress of the European Academy of Neurology (EAN).
InFo NEUROLOGY & PSYCHIATRY 2019; 17(6): 31 (published 11/24/19, ahead of print).