The new S3 guideline “Diagnosis, therapy and follow-up of penile carcinoma” aims to improve the quality of care for affected patients. The focus is on organ preservation.
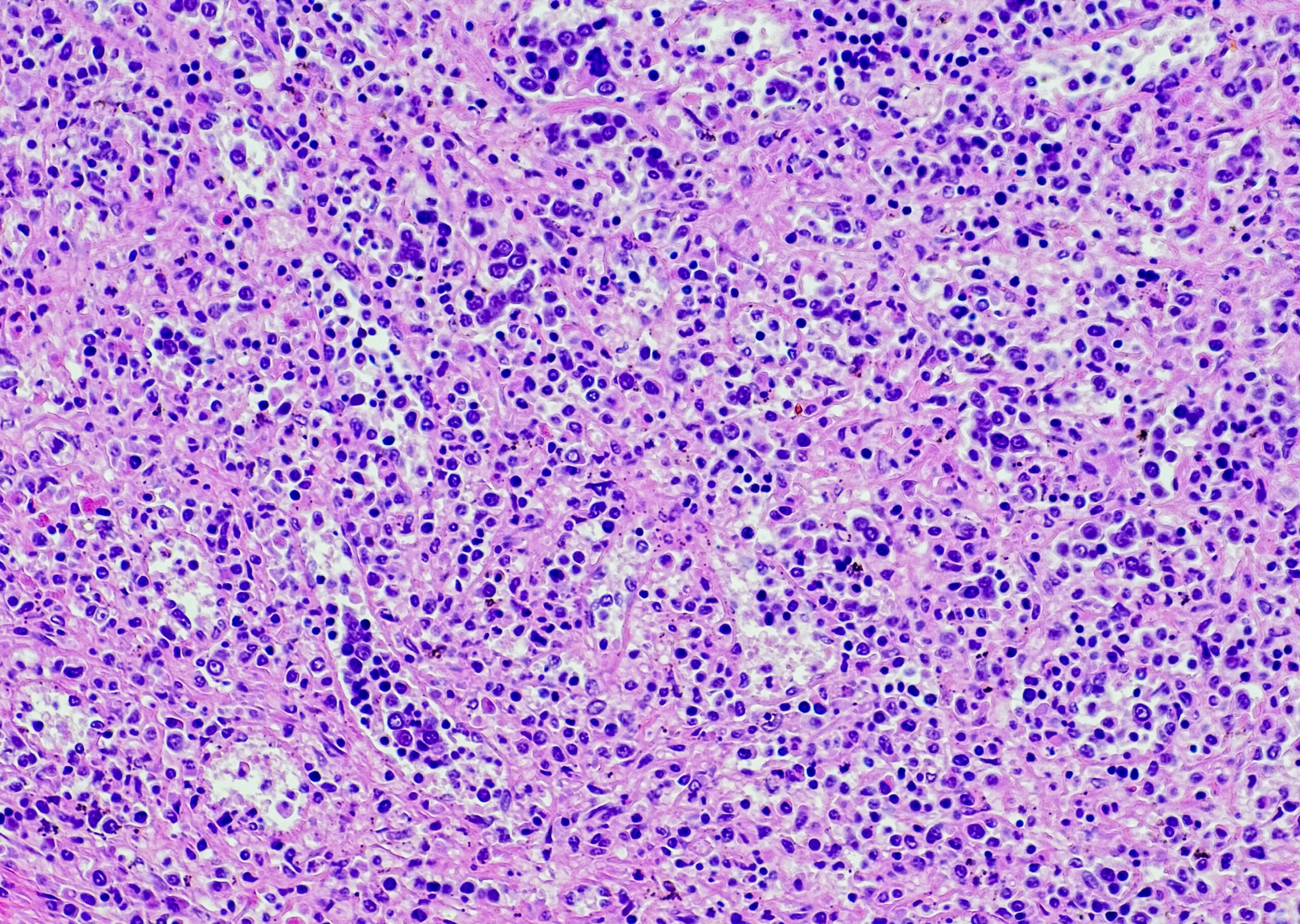
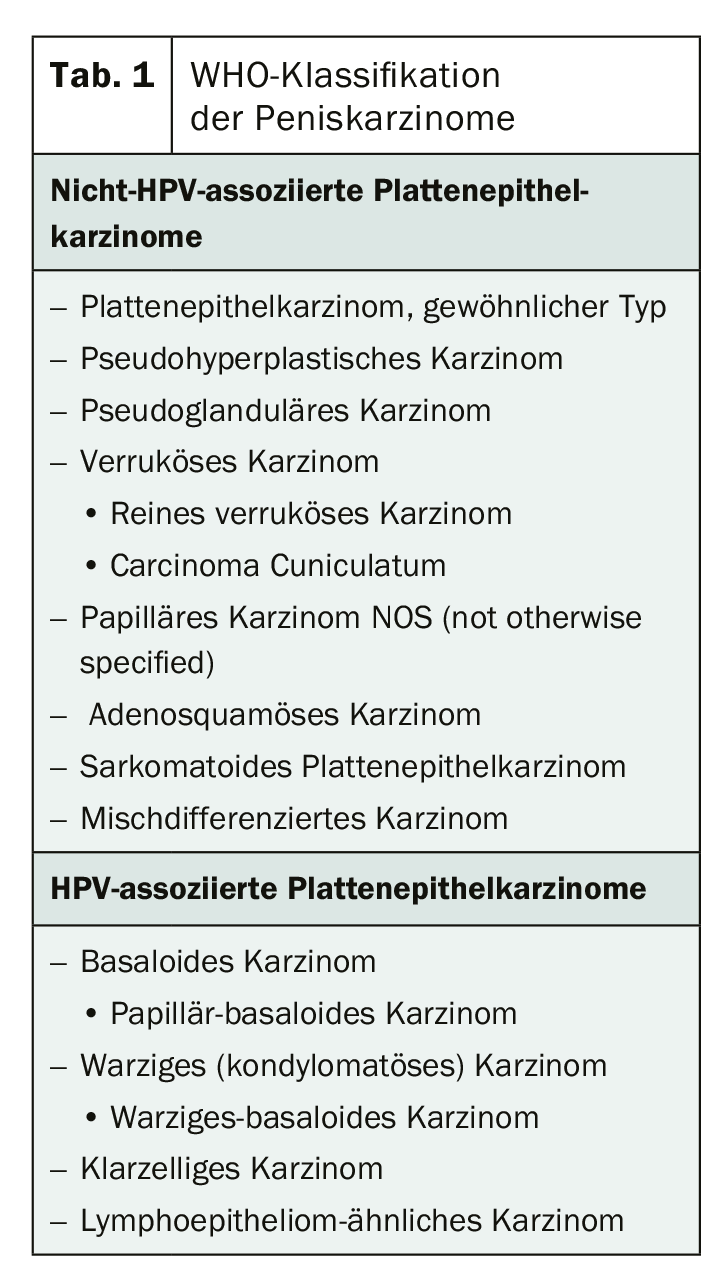
According to the WHO classification, squamous cell carcinoma of the penis is divided into histological subtypes – the non-HPV-associated and the HPV-associated squamous cell carcinomas (Table 1). The common squamous cell carcinoma predominates with 41%, followed by the basaloid penile carcinoma (7%) and the warty subtype with 5%. The macroscopic growth forms largely determine the prognosis. The superficial spreading type, for example, has a rather good prognosis in contrast to the deeply invasive penile carcinoma.
HPV status as a marker for therapy management
Currently, there are no molecular biological markers that can be recommended for routine diagnosis of penile carcinoma. Nevertheless, the pathological findings should include a statement as to whether the disease is HPV-associated or not. This could provide additional decision support for the tumor board, as patients with differential HPV status respond differently to chemotherapeutic agents or checkpoint inhibitors. However, primary oncogenesis factors can currently be distinguished. The development of therapeutic HPV vaccines may provide an additional therapeutic option in the future. These generate cell-mediated, HLA-restricted matched T-cell immunity that destroys HPV-infected cells via cytotoxic lymphocytes.
Primary goal: organ preservation
Treatment should focus primarily on organ preservation, depending on the stage and degree of differentiation. This is because it has been proven that mutilating procedures on the external genium result in significant psychological and psycho-oncological problems. Especially in younger patients, this can lead to significant social and occupational limitations. The key to organ preservation is a tumor-free incision margin. In the meantime, however, it can be assumed that a safety distance of approx. 1 mm is sufficient to achieve this.
Radiotherapy for small tumors
A real alternative to surgery is radiation therapy – especially for small tumors. The guideline recommends local radiotherapy for T1 and T2 tumors. Especially with regard to organ preservation, brachytherapy is an adequate option for tumors ≤4 cm. However, this should only be done in experienced centers and analogous to the published guidelines. However, patients should be educated about the low local control compared with surgical therapy. The use as adjuvant therapy, on the other hand, has not yet been sufficiently investigated in studies, so that no general recommendation can be made. And even in palliative use, no definitive statements can be made. The S3 guideline for patients with noncurable cancer recommends that the indication for local radiation therapy in malignant wounds to reduce the risk of bleeding, exudation, or to reduce disfiguring or difficult-to-care-for tumor manifestations and to reduce edema should be considered.
Source: 71st Congress of the German Society of Urology (DGU)
InFo ONCOLOGY & HEMATOLOGY 2019; 7(5): 31 (published 10/16/19, ahead of print).