An environmental medicine study on the effects of birch pollen on allergic vs. non-allergic individuals reached interesting results. Among other findings, there is evidence that IgG1 and IgG4 levels are predictors of pollen-induced symptoms in both cohorts.
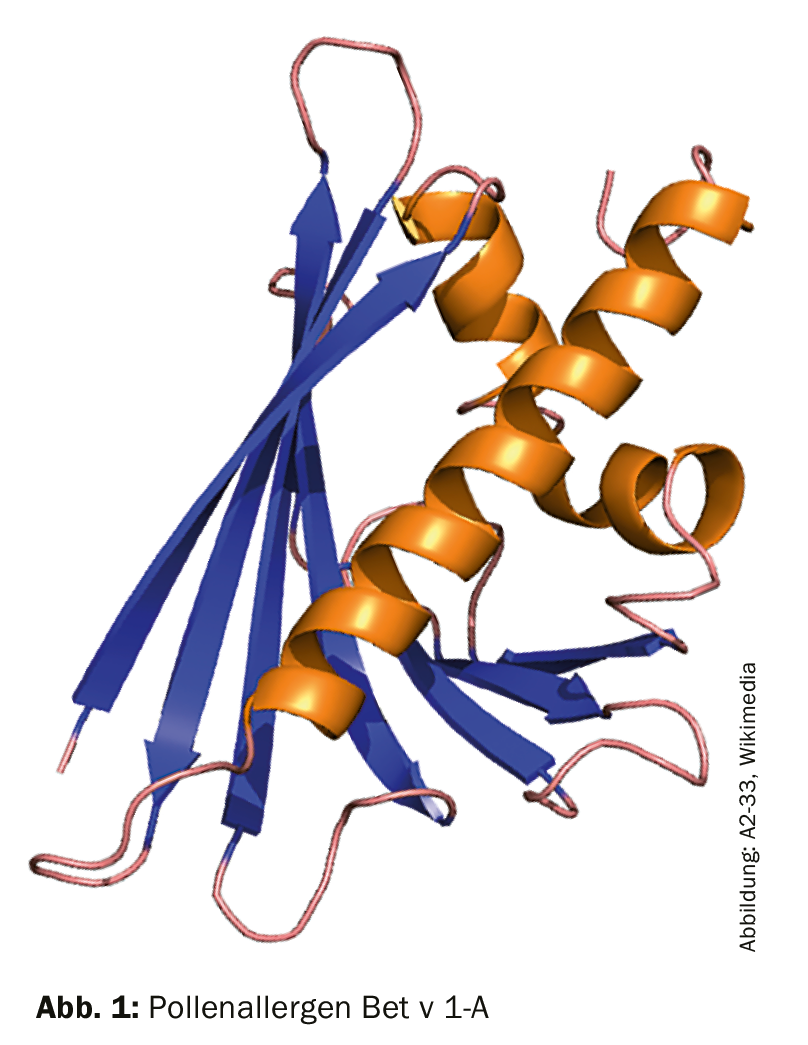
Allergens in pollen from birch trees often trigger allergic reactions in spring (e.g. hay fever, eye inflammation). The peak of birch pollen is in the months of April and May. One of the main allergens is the protein Bet-v-1 (Fig. 1), which is also a marker for sensitization to related tree species such as alder, beech, chestnut, hazel, hornbeam, and oak. Allergy to birch pollen is common in allergic individuals and up to 80% of those affected develop hypersensitivity reactions to Bet-v-1 like proteins in plant foods [1,2]. According to the results of this study, birch pollen can also cause symptoms in non-allergy sufferers. The data indicate that nasal IgG1 and IgG4 levels are predictors of pollen-induced symptoms.
A book with seven seals?
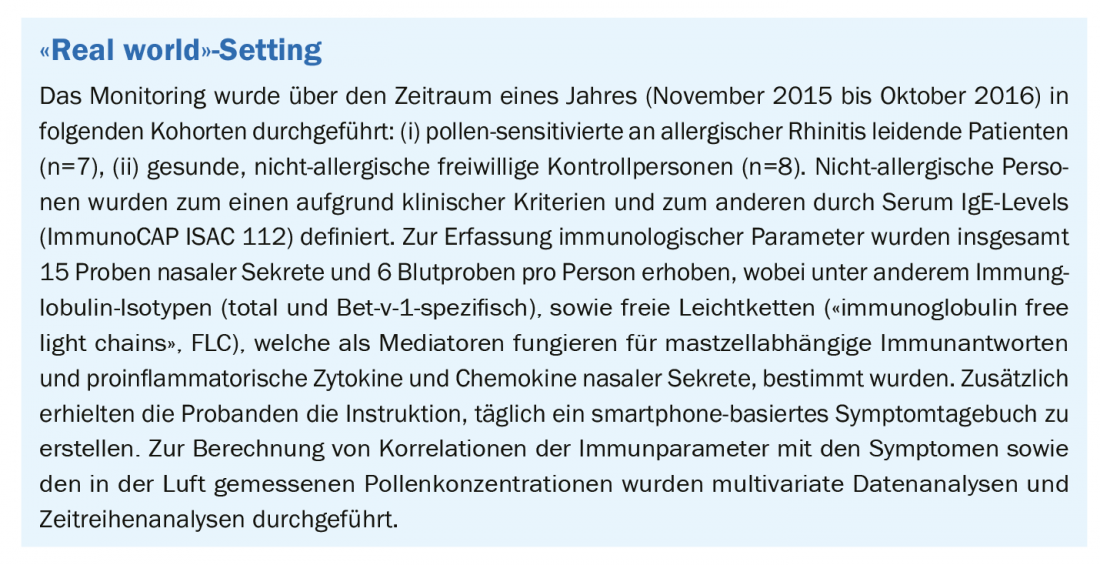
At the current time, not much is known about Bet-v-1-specific immunoglobulin responses to birch pollen, particularly with respect to nasal symptoms. Likewise, little is known about how exactly pollen exposure under natural conditions affects the health of non-allergic individuals. Therefore, the aim of the present study was to assess the effects of birch pollen exposure on respiratory symptoms and on the humoral immune response in allergic and non-allergic subjects: (a) Comparison of local humoral immune responses of patients with allergic rhinitis vs. healthy controls during and outside the pollen season, (b) Evaluation of the kinetic processes of the immune response under natural pollen exposure over the course of one year, (c) Association of immune response profiles with the occurrence of nasal symptoms.
Surprising results
Most surprisingly, not only the allergic but also the non-allergic subjects showed nasal symptoms during the birch pollen season, and these correlated with the pollen concentrations in the air. Unlike hazel pollen and alder pollen exposures, which result in delayed effects, birch pollen has an immediate effect on symptoms in both allergic and non-allergic individuals.
A comparison of values during vs. outside the pollen season shows that total IgA levels, as well as Bet-v-1-specific and FLC levels of nasal secretions are significantly higher during the pollen season only in the non-allergic subjects. A group comparison shows that non-allergy sufferers have significantly higher Bet-v-1 specific IgA, IgG1, and FLC (free light chain) levels during the season than the cohort of allergy sufferers (positively correlated with birch pollen concentration). With regard to IgG4 levels, it was found that after the end of the main pollen season, they were sigfnificantly higher in the allergic patients compared to the control group. The immune profiles of the nasal secretions of both cohorts differed with respect to the following cytokines: IL-33, eotaxin-2, IL-1β.
A principal component analysis based on a correlation matrix of normalized nasal immunomodulators also revealed that the loadings were highest for nasal IgG1 and IgG4.
Source: 46th ADF Annual Meeting, Munich (D), March 13-16, 2019.
Literature:
- ImmunoCAP Explorer: www.immunocapexplorer.com/de/molekulare-allergologie/birkenpollen-allergie, last accessed March 17, 2019.
- Groh N, et al: Immunoglobulin E and G4 epitopes of the major allergen of birch pollen Bet v 1 share residues critical for antibody binding. Clin Transl Allergy 2013; 3(Suppl3): O15. published online 2013 Jul 25. doi:10.1186/2045-7022-3-S3-O15.
- Gökkaya M, et al.: Changes in immunoglobulin levels under real-life pollen exposure: Role of nasal IgA and IgG antibodies. Poster presentation 46th ADF Annual Meeting, Munich, March 13-16, 2019.
DERMATOLOGIE PRAXIS 2019; 29(2): 33