The dominant topic at the AHA Congress was the SPRINT trial and its implications for future hypertension treatment. Is it prognostically meaningful to target lower systolic blood pressure values in hypertensive patients with increased cardiovascular risk in the future? Other interesting studies were devoted to smoking cessation in hospitalized ACS patients, cardiotoxicity in breast cancer therapy, and telemonitoring in heart failure.
The big news first: In the early-stopped SPRINT trial, whose results were eagerly awaited, lowering systolic blood pressure below the 120 mmHg mark compared with the standard target of <140 mmHg resulted in a 27 percent reduction in all-cause mortality and a 43 percent reduction in cardiovascular mortality. The surprisingly clear results not only attracted a lot of attention at the congress itself, but also triggered a great deal of controversy internationally on various scientific discussion platforms.
Key data: The study enrolled 9361 US patients aged ≥50 years with hypertension and at least one other cardiovascular risk factor (but without diabetes, prior stroke, polycystic or advanced kidney disease). Systolic blood pressure had to be 130-180 mmHg at baseline, treated or untreated. The choice of blood pressure therapy during the study was left to the treating physicians, with those patients with the target value of <120 mmHg eventually receiving an average of three antihypertensive drugs and those in the standard arm (<140 mmHg) receiving two. During follow-up, mean blood pressure values were 121.5 mmHg vs. 134.6 mmHg. On average, participants were just under 68 years old, so this was an older study population.
In addition to mortality reductions, which were among the secondary endpoints, the lower target value also led to an impressive result in the primary composite endpoint (myocardial infarction, other acute coronary syndromes, stroke, acute decompensated heart failure, cardiovascular death): risk decreased by 25% after 3.26 years compared with the group with the guideline-compliant target value (HR 0.75; 95% CI 0.64-0.89; p<0,001). The greatest protective cardiovascular effect was seen in heart failure, whereas neither stroke nor myocardial infarction nor acute coronary syndrome, considered separately, occurred significantly less frequently.
Severe complications were found equally frequently overall (38.3% vs. 37.1%). Hypotension, syncope and acute kidney injury resp. However, renal failure occurred significantly more frequently in those receiving intensive therapy. In the subgroup that already had renal disease at baseline, the proportion of patients with worsening renal function was the same in the two arms. In contrast, in patients without renal disease, a 30% (or greater) drop in GFR to values below 60 ml/min occurred more frequently with intensive blood pressure lowering. There will be more detailed analyses of this in the future.
Concurrent with the presentation at the congress, the study was published in the New England Journal of Medicine [1].
What next?
Clearly more exciting than the bare figures of the study are considerations of how the results fit into the evidence base to date. Are the side effects tolerable or do the advantages outweigh the disadvantages? The authors emphasize that bradycardia and falls leading to injury did not occur more frequently and orthostatic hypotension even less frequently in the intensively treated group. The increase in other adverse events was moderate at%–2%, and patients older than 75 years (28% of the total population) tolerated intensive therapy at least as well as younger participants. Overall, the rate of serious adverse events associated with the intervention was low (although significantly higher in the intensive arm: 4.7% vs. 2.5%). Of course, the observed complications should nevertheless not be taken lightly, since, for example, renal diseases in particular are associated with increased morbidity and mortality. Moreover, long-term effects cannot yet be estimated.
The treatment effect of more intensive therapy was evident in all prespecified subgroups (eg, sex, renal function, and preexisting cardiovascular disease). Men, individuals ≥75 years of age, and patients without preexisting cardiovascular disease or chronic kidney disease particularly benefited from the more aggressive targets in the primary endpoint. In addition, the lower the baseline blood pressure, the greater the benefit. Thus, SPRINT did not confirm the much-discussed therapeutic principle that individuals with hypertension and increased cardiovascular risk from comorbidities such as coronary artery disease or chronic kidney disease benefit most from lower target values. But what about diabetes comorbidity?
Diabetics with high blood pressure
The choice to exclude patients with diabetes from SPRINT was considered critically given the relevance of this comorbidity. How should hypertensive diabetic patients be managed in the future? Many experts place the results in the context of the ACCORD study published some time ago [2]. ACCORD compared the same target blood pressure values as SPRINT in a high-risk collective with diabetes mellitus. The risk reduction of 12% in the similarly defined primary end point as in SPRINT (but without heart failure) was not significant here. Nor were there any relevant advantages with regard to mortality. While SPRINT surprisingly failed to demonstrate a significant risk reduction for stroke, ACCORD was the only parameter with a significant benefit from more intensive therapy.
How can the differences be explained? It is possible that ACCORD was simply underpowered; after all, the event rate was significantly lower than anticipated; moreover, the confidence intervals were wide and included risk reductions in the size range of SPRINT (27%). Last but not least, there were differences regarding diuretic use (hydrochlorothiazide frequently in ACCORD, chlortalidone primarily in SPRINT). Because diabetes therapy was also different in ACCORD, there were also differences in glycemic control: it was more intense in some patients than in others. It is known that intensive glycemic control can increase event rates. Ultimately, the question of the appropriate target value for diabetics remains unanswered: 140, 135, 130, or 120 mmHg after all? The overall adverse event rate was low in ACCORD. A new, adequately powered study could provide the answer.
Good reasons for a follow-up study are also provided by the long-term follow-up of ACCORD called ACCORDION. The results were presented at the congress. During follow-up, the lower blood pressure value was no longer targeted, resulting in the disappearance of the significant difference with respect to stroke. Accordingly, this was actually an expression of the more aggressive blood pressure targets. In addition, it was demonstrated that intensive glycemic control had significantly interacted with the results.
Generalizability unclear overall
Systolic blood pressure was only moderately elevated in SPRINT at baseline (139.7 mmHg). Does the lower target value now also apply to patients with more severe hypertension? And what about younger patients and those with previous stroke? Are we dealing with a target that is universally applicable in all patients or only in a subset? First follow-up publications suggest that the SPRINT results are relevant for large parts of the hypertension population [3]. But the concrete implementation in practice is questionable in view of the fact that not even in the study setting a mean target value of <120 mmHg was achieved. Furthermore, it can be assumed that many patients do not want an extension of their therapy regime (no additional tablet) – not least because of the increasing costs and control consultations. In SPRINT, drugs were provided free of charge, which led to increased use of even expensive first-line therapies.
Varenicline successful in hospitalized smokers.
Smokers hospitalized for ACS rarely remain abstinent after discharge. This leads to an increase in morbidity and mortality. Apparently, twelve weeks of varenicline therapy (2× 1 mg/d) initiated already in the hospital may help to increase abstinence rates, at least during the observation period. This is suggested by the results of a randomized, placebo-controlled trial involving 302 subjects, mostly men, with an average age of 55 years. At the time of the ACS, they had smoked for an average of 36 years and were currently smoking 21 cigarettes per day. According to the Fagerström test, they were considered moderately to severely dependent.
A significant benefit of the therapy was already evident from week four. After 24 weeks, the primary endpoint, point prevalence for abstinence in the last seven days according to self-report and measurement of exhaled carbon monoxide, was 47.3% vs. 32.5% (p=0.012; NNT 6.8). Of seven ACS patients, one managed to become a non-smoker thanks to varenicline. The continuous abstinence rate, i.e., verified smoking cessation since baseline, was 35.8% vs. 25.8% at 24 weeks (NNT 10). This difference was no longer significant, after a significant advantage had been shown in weeks four and twelve. For this, 67.4% vs. 55.6% achieved a reduction of 50% or more in their daily cigarette consumption with varenicline (p<0.05). Within 30 days after stopping the medication, no side effects occurred more frequently in the intervention group than with placebo. Major cardiovascular events such as myocardial infarction, unstable angina, or cardiovascular death occurred in 4% vs. 4.6%. During treatment, patients sometimes complained of nausea or insomnia, but compared to placebo, only the side effect “strange dreams” occurred significantly more often under varenicline.
The data are promising. To date, nicotine replacement products are commonly prescribed during hospitalization despite a lack of evidence. While varenicline was known to be effective in “healthy” smokers and those with stable CHD, its effect in ACS had not been extensively tested. Further studies are needed on the safety aspects, as the study was not powered for this.
It is possible that the combination with nicotine replacement products may further increase the benefit of varenicline – in terms of an immediate effect against “craving” with nicotine replacement and a long-term one with varenicline. In any case, experts see the start of therapy in the hospital as a suitable time window, since the patient usually does not smoke here (at least for a short time).
PRADA – cardiac prevention during breast cancer therapy
Currently used adjuvant therapy regimens in early breast cancer prolong survival but may lead to cardiac dysfunction and consecutive clinical heart failure. PRADA is a randomized controlled trial that tested the cardioprotective effect of the beta-blocker metoprolol (target dose 100 mg/d) and/or the angiotensin receptor blocker candesartan (32 mg/d) vs placebo. 120 average 50-year-old women undergoing adjuvant therapy with anthracyclines with/without trastuzumab and radiation participated. Apart from breast cancer, the patients had no other serious diseases, in particular no cardiovascular diseases. Left ventricular ejection fraction (LVEF) was ≥50%.
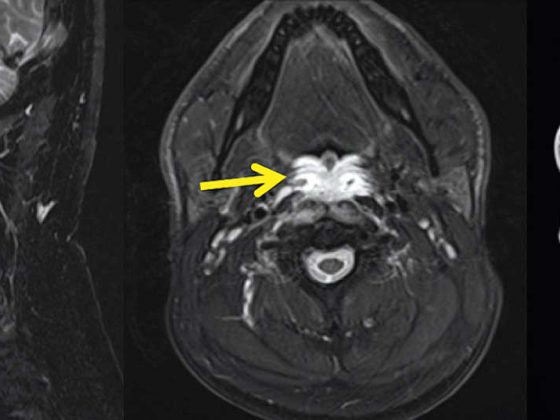
The primary endpoint, LVEF (imaging by cardiac MRI), showed a decrease of 2.6% in the placebo group vs. 0.8% in the candesartan group after cancer therapy (p=0.026). No protective effects were found with metoprolol. Although the sample was small, PRADA is the largest study on this topic. The implications for practice are unclear given the significant but overall modest differences in LVEF. In addition, a possible limitation could be that this was a low-risk population. Long-term follow-up and further studies are useful in any case.
Telemonitoring disappoints
With patient education while still in the hospital, telephone coaching and home monitoring, the rate of heart failure rehospitalizations can be reduced. This is the hypothesis of the randomized controlled BEAT-HF, one of the largest studies in this field. Telephone coaching took place weekly for the first month and monthly thereafter. Specifically trained nurses were used. Telemonitoring consisted of weight, blood pressure, heart rate, and symptom parameters. The data were transmitted electronically on a daily basis and reviewed by the technical staff. Patients were called when limits were exceeded. In case of significant symptoms, patients were referred to the appropriate physicians.
The population consisted of 1437 hospitalized heart failure patients with a median age of 73 years (61% with NYHA III or IV). There were no differences between the standard and telemonitoring groups at either 30 or 180 days. This was true for rehospitalizations and, at least after 180 days, also for mortality. After 30 days, mortality was significantly reduced, but this was not due to the intervention but to deaths while still in hospital.
On the one hand, the result is not surprising if one thinks back to earlier large studies such as Tele-HF or TIM-HF, which also showed no benefit in terms of rehospitalization or mortality. On the other hand, it had been hoped to improve adherence and thus outcome through new technologies, specific encouragement/education of the patient while still in hospital, and regular telephone contacts with trained nurses. In addition, there are monitoring studies that were positive. So what went wrong in BEAT-HF?
Lack of integration of the intervention into the primary care practice providing care and the rapid progress of technology (in the meantime, there are already numerous advanced approaches with implantable devices, wristwatches, etc.) may have given the study a leg up. Adherence appears to be critical: a post-hoc analysis showed significant benefits in both mortality and rehospitalization in patients who were monitored more than 50% of the days and made more than half of the coaching calls.
However one ultimately interprets the data: A definitive conclusion on this subject is not possible at present.
Source: American H eart Association (AHA) 2015 Scientific Sessions, November 7-11, 2015, Orlando.
Literature:
- The SPRINT Research Group: A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med 2015; 373: 2103-2116.
- The ACCORD Study Group: Effects of Intensive Blood-Pressure Control in Type 2 Diabetes Mellitus. N Engl J Med 2010; 362: 1575-1585.
- Bress AP, et al: Generalizability of results from the Systolic Blood Pressure Intervention Trial (SPRINT) to the US adult population. J Am Coll Cardiol 2015 Oct 31. pii: S0735-1097(15)07103-X.
CARDIOVASC 2016; 15(1): 33-34