Multiple sclerosis is a relatively common inflammatory disease of the brain and the entire central nervous system in which demyelination, the cause of which is still unclear, occurs [1]. Diagnosis is based on diagnostic criteria with occurrence of repeated neurological deficits, detection of oligoclonal bands in CSF, and often typical radiological findings; only magnetic resonance imaging (MRI) is used as an imaging modality. MRI reveals typical inflammatory plaques in the white matter, often located paracallosally and periventricularly. Because the
diagnosis is not always clear, radiological classifications are very helpful (e.g. McDonald criteria). They are based on accurate classification in terms of number, localization, contrast uptake, and temporal changes in foci.
Multiple sclerosis (MS) is the most common chronic inflammatory disease of the central nervous system in Central Europe. It usually occurs early in life, so aggressive treatment is necessary. It predominantly affects young women (2:1 ratio) who have a long life expectancy and may face increasing disability without treatment. It is a so-called demyelinating disease of the central nervous system in which the white matter is destroyed by inflammatory changes. Since the disease can affect the entire nervous system and the clinical symptoms are multifaceted, the disease cannot be diagnosed quite clearly even in many cases at the beginning. This article discusses the basics of radiological diagnosis, as well as techniques and criteria that can help to facilitate the diagnosis.
A central problem with the disease is that the triggering factor (antigen) has not been precisely identified to date. There seems to be clear evidence of an external triggering factor on the one hand, but it is likely that genetic predisposition also plays a role. The course of the disease is inconsistent and the primary imaging findings are not always clear. According to some experts, MS is also not necessarily a uniform disease pattern. This also means that treatment is still essentially only symptomatic. However, treatment of the disease has made great strides in recent years, especially with the development of drugs for immunomodulation and immunosuppression.
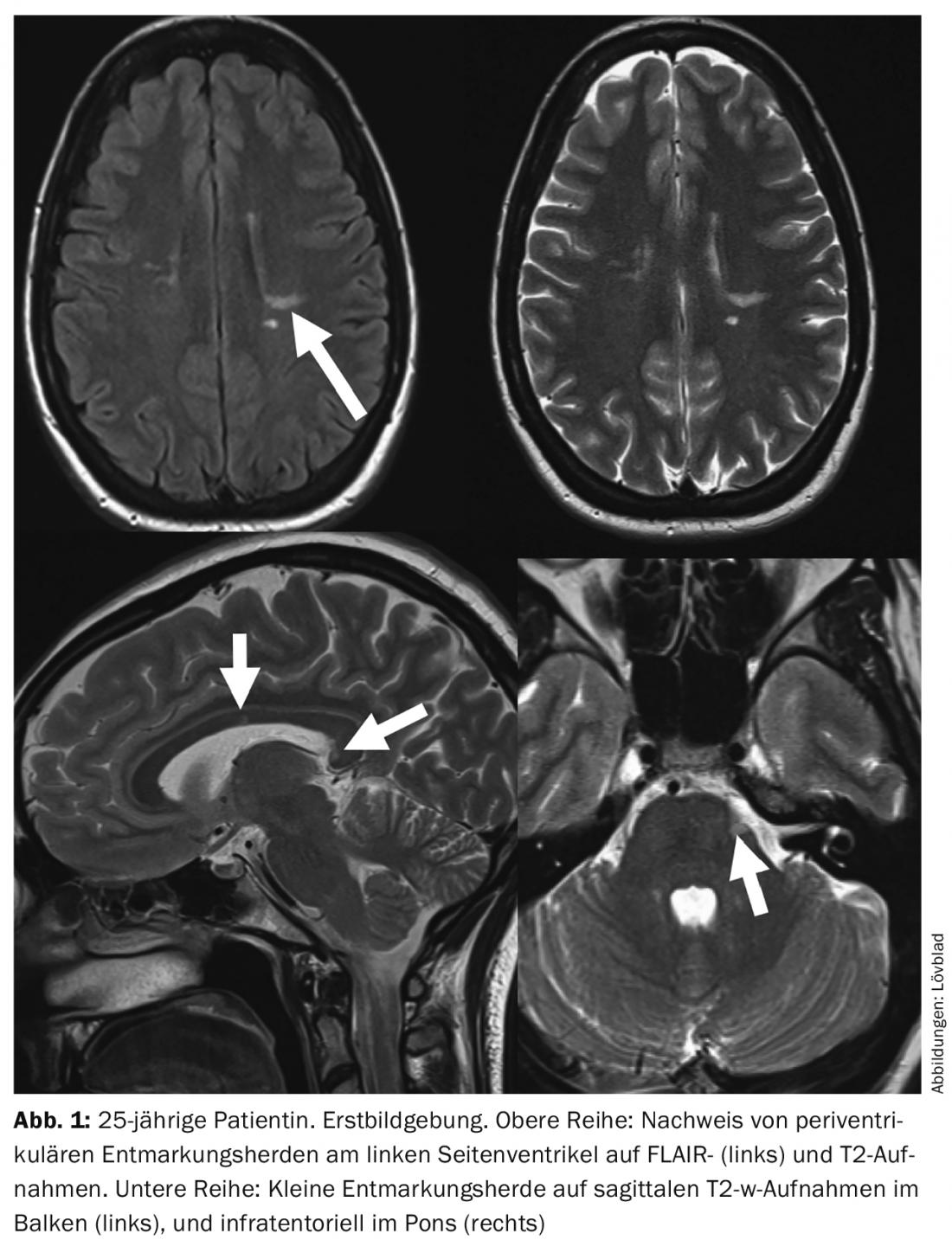
Imaging of the CNS plays a central role today. The diagnosis of MS is usually based on imaging findings. However, it is important to remember that the clinical findings always guide the diagnostic procedure [2]. An important concept is the so-called “clinically isolated syndrome”. This is the first occurrence of isolated neurological symptomatology due to inflammatory demyelination. These patients most often, but not always, have or will develop definitive MRI findings over time. Another concept is “radiologically isolated syndrome,” in which imaging findings show changes typical of MS but the patient is asymptomatic in this regard (Fig. 1).
Choice of imaging technique
Computed tomography was used at the beginning of axial imaging of the brain. Plaques could sometimes be seen here as hypodensities, especially larger “Dawson’s fingers” (the ovoid lesions perpendicular to the ventricles look like transversely cut fingers).
Computer tomography has since been replaced by magnetic resonance imaging. MRI has the advantage that it does not generate ionizing radiation, this means that the examination can be repeated several times. Most importantly, MRI allows multiplanar imaging of the nervous system with better resolution for inflammatory changes in the brain. Nevertheless, there is still the case today that, due to a neurological deficit, a patient with an onset of MS will have a CT scan if an intracerebral hemorrhage is suspected, for example. In these cases, especially if the expected finding cannot be delineated, demyelinating plaques should be considered. Otherwise, MRI is the modality of choice both for primary diagnosis and subsequent follow-up examinations, as well as for the conduct of therapeutic studies (“drug trials”), which remain necessary to establish optimal treatment. It is important that the examination be as complete as possible so that the diagnosis can be made with certainty and potentially successful treatment can be started as soon as possible and side effects of therapies can be detected (e.g., progressive multifocal leukoencephalopathy [PML]).
MRI findings
The demyelinating plaques are visualized on MRI as hypointensities on T1 sequences and as hyperintensities on T2-weighted sequences. Old “burned-out” MS lesions are referred to as “black holes” because they appear very dark to black on T1-weighted sequences. The total volume of these black holes is called lesion load and correlates with clinical status and outcome. One sequence that has found its full application potential in MS imaging is the FLAIR sequence. This is a T2-weighted sequence in which free fluid (Liqour) no longer gives a signal: This allows lesions that are close to the ventricular system to be seen more clearly. These sequences are usually performed in the axial plane. One plane that is extremely important in MS imaging is the sagittal plane: this allows good topical visualization of lesions in the bar. With the development of better isotropic 3D sequences, it is now possible to record T1-weighted, T2-weighted, or FLAIR sequences as a volume set that can be reconstructed afterwards in any plane. This also allows the image plane to be reconstructed identically during progression examinations. The 3D images are also the norm in therapeutic studies to calculate the volumes of the lesions.
Never forget that MS can potentially affect all parts of the nervous system. Therefore, it is often necessary to image the remaining sections such as the myelon or the orbitals, even if this leads to a significant increase in examination time.
Classification criteria
When evaluating MR examination, it is important to use well-established criteria based on the accurate description of the number, location, and contrast behavior of lesions [3]. Also, it is often important to repeat the examination to show the local and temporal fluctuation of the lesions. The most commonly used criteria for diagnosing MS are those of McDonald. If foci are present in at least two of four locations (periventricular, juxtacortical, infratentorial, or spinal), the criteria for local dissemination are met. Temporal dissemination is fulfilled when one or more clinically asymptomatic foci take up contrast or when new foci appear in a follow-up scan.
Contrast administration still plays a central role in diagnosis: it allows visualization of disease activity as well as monitoring of active plaques during treatment and, as mentioned above, is part of the McDonald criteria. However, one should be aware of the potential side effects. Contrast allergies associated with MR contrast administration are extremely rare. There is some risk of nephrogenic fibrosing dermatopathy (NSF) in patients with inflammatory diseases, but this is also extremely low. An additional controversial issue is the possible accumulation of gadolinium in the brain, especially in patients who have been studied more than once; this is the case in MS patients, but the data on this still need to be reviewed.
New techniques
Several newer (“advanced”) MRI techniques show promising results, but they have not yet fully gained clinical acceptance. Because the disease affects the white matter, diffusion tensor imaging (DTI) would be of interest in addition to basal diffusion imaging. A method like DTI allows a better evaluation of the so-called “normal appearing white matter”; and therefore has a lot of potential especially for scientific purposes and for the establishment of new therapeutic strategies. The same is true for different perfusion methods, but these are also not yet used clinically. These modalities will certainly play a major role in future research and contribute to a better understanding of the underlying pathophysiology of the disease.
Summary
Multiple sclerosis is a demyelinating disease of the CNS in which radiological criteria play a major role in addition to clinical criteria. MRI is the method of choice and consists of a combination of T2 and flair sequences along with T1-weighted images with contrast. Three-dimensional sequences are playing an increasing role, as they allow reconstruction in every level of the brain and better comparability over time. The goal is to represent a disease that affects the entire CNS, with a temporal and local evolution. It is important to use established diagnostic criteria such as the McDonald criteria and to mention them accurately in the radiologic report.
Literature:
- Lövblad KO, et al: MR imaging in multiple sclerosis: review and recommendations for current practice. AJNR Am J Neuroradiol 2010 Jun; 31(6): 983-989.
- Haller S, et al: Magnetic resonance imaging in multiple sclerosis. Top Magn Reson Imaging 2009 Dec; 20(6): 313-323.
- Polman CH, et al: Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 2011 Feb; 69(2): 292-302.
InFo NEUROLOGY & PSYCHIATRY 2016; 14(1): 4-6.











