The currently known and established hereditary thrombophilias are statistically associated with an increased clinical risk of thrombosis. This risk is variably expressed and depends on the individual genetic background of each patient. The presence of hereditary thrombophilia should never be considered the sole explanation for a thromboembolic event. It is important that this is explained in detail to the patients concerned during a consultation.
Venous thromboembolism (VTE) is associated with a relevant risk of morbidity and also mortality. Primary and secondary prevention are key to reducing these risks. In order to use drug prophylaxis correctly in terms of anticoagulation, it is necessary to have the best possible understanding of the factors that influence the development of VTE.
Hereditary or acquired conditions that lead to an increased tendency to thrombosis are referred to as thrombophilias. However, it is the case that VTE are complex disorders that occur as a result of the interaction of various hereditary or acquired risk factors.
To estimate the risk of recurrence after a history of VTE, all these risk factors must be taken into account. Unfortunately, the significance of currently known hereditary thrombophilias with regard to recurrence risk is limited. This is one reason why they do not play a relevant role in the management of VTE, even according to the current guidelines of the American College of Chest Physicians (ACCP) of 2012. Rather, what is more crucial in determining the duration of anticoagulation is whether an event occurred provoked or unprovoked (idiopathic).
A provoked event is said to occur when a trigger for the VTE can be demonstrated. However, these triggers are not entirely uniformly defined in the relevant studies. A distinction is usually made between strong triggers such as plaster immobilization, fracture of an extremity, surgery under general anesthesia, or active cancer and weaker triggers such as pregnancy, puerperium, estrogen-containing contraceptives, or immobilizing travel. Studies have repeatedly shown that unprovoked VTE carry a significantly higher risk of recurrence than provoked VTE (provided the provoking factor is reversible). Nevertheless, in individual cases it may be useful to have knowledge about existing hereditary or acquired thrombophilias in order to be able to advise and treat the patient optimally. In the following, we would like to point out the role of different thrombophilic factors as well as a reasonable use of laboratory diagnostics considering the current data.
Thrombophilic factors
Age: The risk of VTE increases with age. While the incidence of VTE is 1:1000 in those under 50 years of age, it increases almost exponentially in those over 60 years of age and is already 1:100 in those 75 years of age. Statistically, the presence of hereditary thrombophilia no longer significantly increases the risk of VTE in people over 60 years of age.
Family history: a positive family history is a risk factor for VTE, regardless of the presence of a known hereditary thrombophilia. However, this only applies if first-degree relatives (parents, siblings, children) are affected.
Hereditary thrombophilias: Hereditary thrombophilias are usually considered relevant in the literature only if they increase the relative risk of VTE by at least a factor of 2. With regard to a first VTE, according to the current state of knowledge, this applies to the deficiencies of the natural inhibitors protein C, protein S, and antithrombin as well as to the factor V Leiden mutation and the prothrombin gene mutation G20210A. Strictly speaking, the latter two are polymorphisms, as they are found in more than 1% of Caucasians. Prospective studies have shown that the hereditary thrombophilias mentioned above play only a minor role, if any, in influencing the risk of VTE recurrence. However, once multiple hereditary thrombophilias are present in the same individual (combined heterozygous or homozygous defects), the risk of recurrence is significantly affected.
In the case of other potentially thrombophilic conditions such as persistently elevated factor VIII and mild hyperhomocystinuria, but also various genetic polymorphisms (e.g., PAI-1 4G polymorphism, ACE deletion polymorphism), the data situation regarding the influence on recurrent thrombosis is unclear.
Acquired thrombophilia: Antiphospholipid syndrome is the most important laboratory-detectable acquired thrombophilia. Several cohort studies show a high risk of recurrence of venous and arterial thrombosis when antiphospholipid antibodies persist (anti-cardiolipin antibodies, anti-beta2-glycoprotein antibodies, lupus anticoagulant).
Thrombophilia screening in the laboratory
Based on current data, thrombophilia screening should primarily include a search for deficiency of the natural inhibitors protein S, protein C, and antithrombin, as well as the genetic polymorphisms factor V Leiden and prothrombin gene mutation G20210A. Ideally, antiphospholipid syndrome diagnostics are also performed. This panel is also so recommended by various national guidelines.
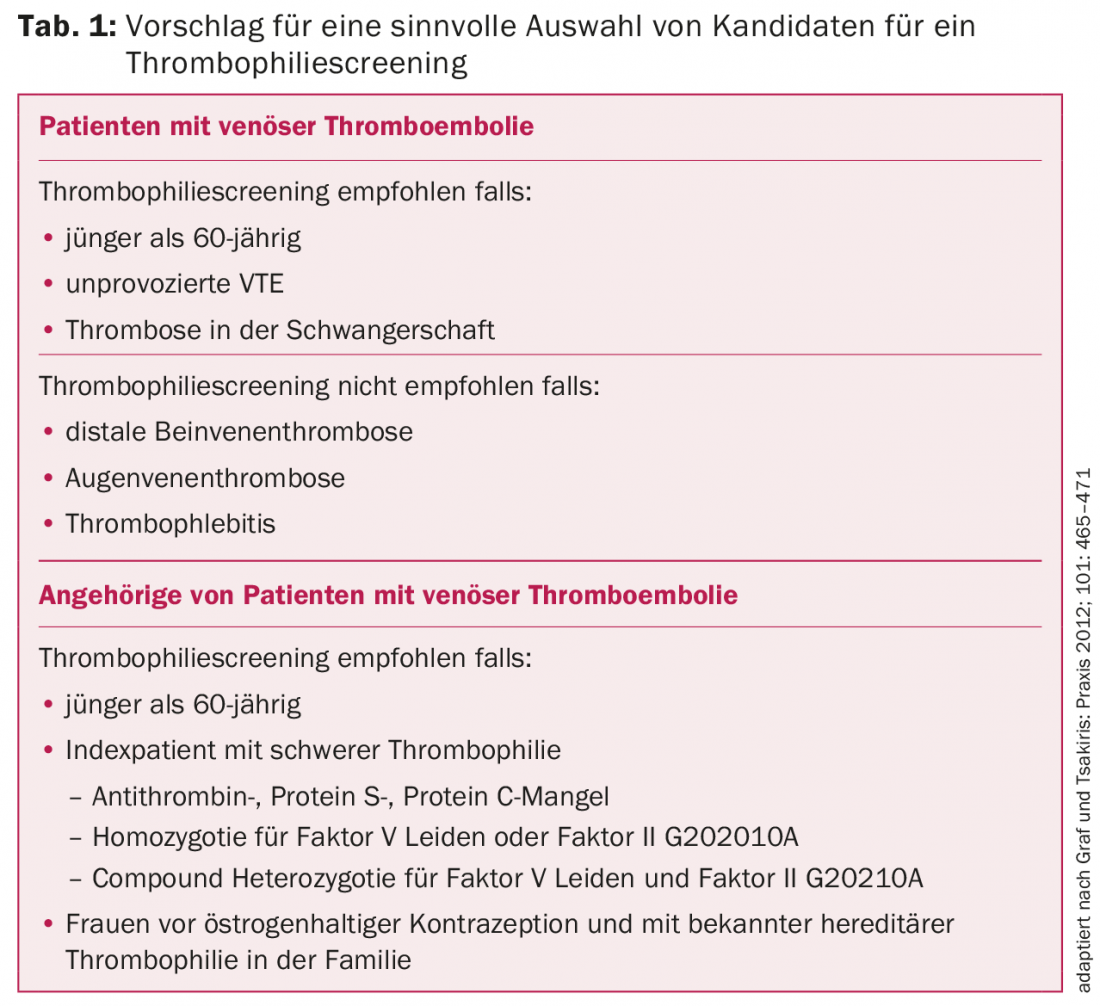
Thrombophilia screening should generally be considered for any first episode of proximal deep vein thrombosis or pulmonary embolism in patients younger than 60 years of age. However, if there is a clear trigger for the event, screening may not be necessary in men and postmenopausal women. Patients with recurrent unprovoked VTE are generally candidates for time-unlimited anticoagulation, and management would not change with positive thrombophilia screening. In such cases, thrombophilia screening is therefore advisable only if it could result in family clarification (Table 1).
The timing at which thrombophilia screening should ideally be performed is controversial. According to the ACCP guidelines, after three months of anticoagulation, a decision should be made regarding its longer-term duration. However, there is no mention of thrombophilia screening as a potential decision aid. Rather less than ideal is thrombophilia screening just at the time of the acute event. The natural inhibitors are then often lowered due to consumption, so that no conclusive statement can be made in this respect. Moreover, the type of initial treatment does not depend on the presence of thrombophilia either.
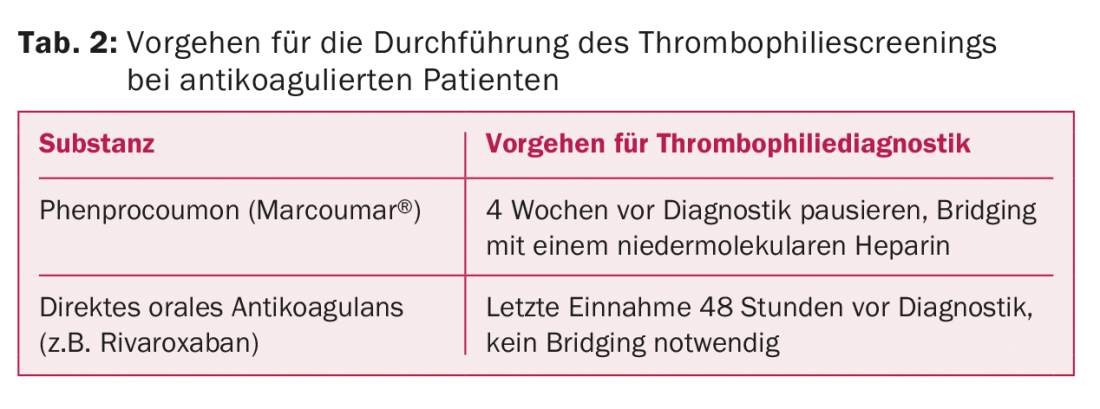
In patients who are candidates for longer-term anticoagulation, it is probably most appropriate to screen for thrombophilia approximately three months after VTE. Since patients must not be anticoagulated at the time of blood collection, anticoagulation must be discontinued for a short period of time. A possible practical approach is shown in Table 2.
Pathological, functionally measured parameters (e.g., a reduced activity of a natural inhibitor) should be confirmed in a second measurement during the course to exclude a disorder that is only transiently present.
Special situations
Distal deep vein thrombosis: Based on current data, it is unclear how anticoagulation should be performed for infrapopliteal thrombosis. The ACCP guidelines also mention monitoring by imaging alone as an option in selected cases. Certain data suggest that patients with distal leg vein thrombosis are less likely to be carriers of hereditary thrombophilia than patients with proximal leg vein thrombosis. Thrombophilia screening in patients with distal leg vein thrombosis should therefore be used with caution (Table 1).
Superficial venous thrombosis (thrombophlebitis): There are no reliable data regarding the prevalence of thrombophilia in superficial venous thrombosis, nor is the treatment of superficial venous thrombosis influenced by the presence of thrombophilia. Therefore, thrombophilia screening in superficial venous thrombosis cannot be recommended.
Cerebral venous thrombosis: The association of hereditary thrombophilia with cerebral venous thrombosis has been clearly demonstrated and thrombophilia screening may therefore be useful. However, as with other atypically localized venous thromboses, it is essential to actively exclude other causes such as myeloproliferative disease or paroxysmal nocturnal hemoglobinuria (PNH).
Retinal vein thrombosis: The known hereditary thrombophilias show only a very weak association, if any, with ophthalmic vein thrombosis. Primarily, therefore, established risk factors such as hypertension, hypercholesterolemia, and diabetes should be sought in retinal vein thrombosis. Thrombophilia screening is usually not indicated.
Intra-abdominal venous th rombosis: Since hereditary thrombophilias are established risk factors for intra-abdominal venous thrombosis, it is reasonable to screen patients under 60 years of age accordingly. However, it should be remembered that myeloproliferative disorders, PNH, liver cirrhosis, and abdominal surgery are also important risk factors for intra-abdominal venous thrombosis. Since the Janus kinase mutation JAK2V617F, which is typical for myeloproliferative neoplasms, can be detected in up to almost 20% of cases, the corresponding molecular genetic search is useful, even if no obvious blood count changes are present.
Family clarifications
In the case of proven hereditary thrombophilia in the index patient, asymptomatic relatives are often also specifically clarified for the thrombophilia proven in the patient in a second step in common practice. However, it has never been shown with certainty that thromboembolic events can actually be significantly prevented by consistent thromboembolic prophylaxis in carriers of thrombophilia. Family clarification should therefore be used only in selected situations, and it should generally be limited to first-degree relatives of the index patient who are younger than 60 years of age. It may be useful to screen young female relatives for possible pregnancy or contraception. Possible selection criteria for a family assessment are shown in Table 1.
Bibliography by the authors
CARDIOVASC 2015; 14(2): 24-26