Pathological changes of the skin and skin appendages are very common in the context of internal diseases. Dermatoses may precede such a disease as primary symptoms on the one hand, or they may develop during its course. Thus, from a thorough dermatologic examination, cutaneous clues to internal diseases often emerge. This article is intended to give an excerpt about more common as well as less common skin manifestations in internal diseases in adults.
Since the discovery of HIV in 1981, approximately 2.7 million people per year are newly infected with the HI virus. HIV infection and subsequent immunosuppression are associated with various skin manifestations. Oral candidiasis is one of the most common mucocutaneous manifestations in HIV-infected patients. In the setting of acute HIV infection, there is often an onset of flu-like symptoms with lymph node swelling, vomiting, diarrhea, arthralgias, and not infrequently morbiliform or maculopapular exanthema. The clinical picture is very similar to infectious mononucleosis. The presence of exanthema is predictive of a very high viral load.
Oral hairy leukoplakia (Fig. 1) is characterized by whitish, streaky, nonwipeable changes that do not cause subjective discomfort and are often localized to the margins of the tongue but also buccally. It was described in 1984 and long thought to be pathognomonic of HIV infection. Oral hairy leukoplakia also occurs in other immunosuppressive conditions and should be evaluated accordingly. The trigger is the Epstein-Barr virus. Complete clinical remission occurs with well-controlled antiretroviral therapy. Periungual erythema (Fig. 2) was first described in 1985 as a marker of HIV and hepatitis C infection.
Severe or chronic herpes simplex virus disease and/or generalized, multisegmental herpes zoster infection occur only in the setting of underlying immunosuppression, such as HIV infection, among others.
In about 90% of HIV-infected persons, there is a latent HPV infection, which not infrequently manifests itself clinically as condylomata acuminata in the genital area.
HIV-associated malignancies include oral and anal squamous cell carcinoma (induced by HPV), basal cell carcinoma, and Kaposi’s sarcoma and non-Hodgkin’s lymphoma, especially Burkitt’s lymphoma. In recent years, HIV-typical malignancies such as Kaposi’s sarcoma have declined, whereas the incidence of non-HIV-associated skin malignancies has increased, which can be explained by a higher life expectancy under HAART and the associated higher relevance of the usual risk factors.
The most frequent non-infectious HIV-associated dermatosis is seborrheic dermatitis and a highly pruritic papular exanthema, also called “pruritic papular eruption” (PPE), in about 10% of patients. PPE is characterized by chronic pruritus with often symmetrically arranged papules and pustules on the extensor sides of the arms, backs of the hands, and trunk and face with exclusion of the palms and soles. Therapy-induced problems such as lipodystrophy or drug exanthema have become common.
Endocrinological diseases
It is estimated that approximately 30-70% of all diabetics develop pathological skin changes. Diabetic dermatopathy (Fig. 3) is the most common cutaneous manifestation of diabetes mellitus. It is characterized by sharply demarcated, erythematous macules, scattered papules that merge into atrophic, slightly scaly hyperpigmented macules.

It is known that the incidence of skin infections in diabetes mellitus has a correlation with the concentration of blood glucose. Other predisposing factors include impaired microcirculation and neuropathy. Candida infections are frequently observed in the genital area, submammary and other intertriginous areas.
Onychomycosis or tinea pedum should be treated, after consideration of comorbidities and/or polypharmacy, if possible, as it is a portal of entry for erysipelas.
A common bacterial infection is erythrasma (Fig. 4), which is caused by Corynebacterium minutissimum.
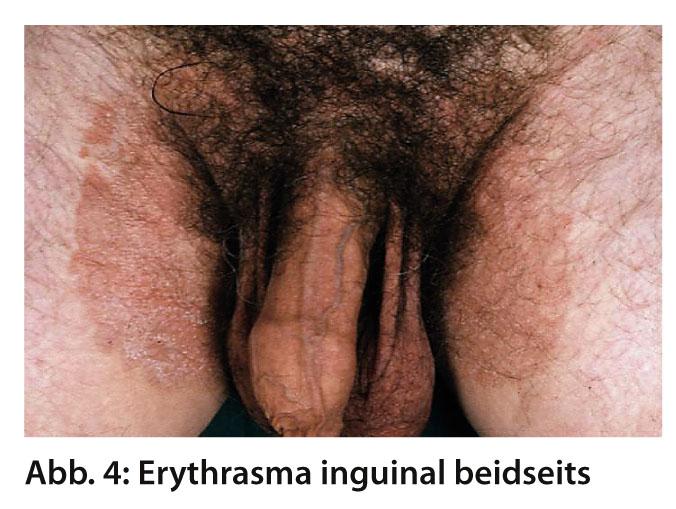
In the Wood light, it glows coral red. In diabetics, impetigo, folliculitis, boils, carbuncles, ecthyma or necrotizing fasciitis caused by Staphylococcus aureus or β-hemolytic streptococci are also more common.
Approximately 1% of diabetics develop necrobiosis lipoidica during their course (Fig. 5).

This typically occurs on the shins, solitary or multiple. Diagnostically helpful are the central atrophy and the slightly infiltrated erythematous rim. Complicating ulcerations with poor healing tendency may occur in one third of patients.
Not infrequently, pruritus vulvae exists as an early symptom of diabetes mellitus.
Acanthosis nigricans (Fig. 6) presents clinically as a grayish-brown, papillomatous-hyperkeratotic, asymptomatic extensive proliferation of the skin, typically on the intertriginous areas, especially axillary, neck, and genital.
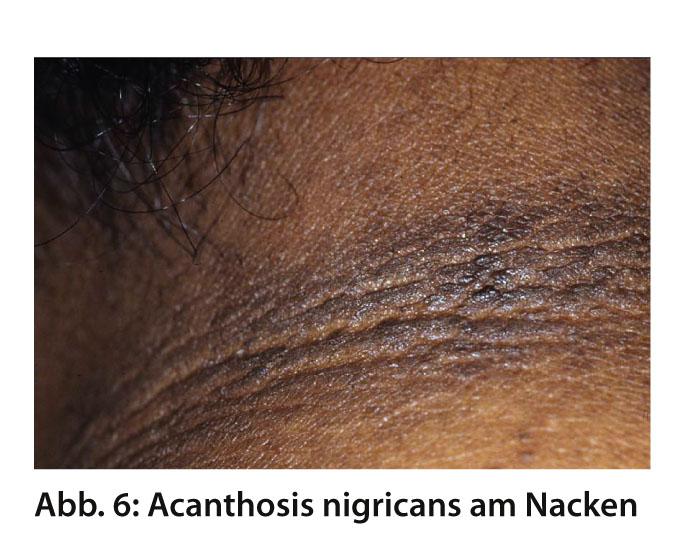
Roughly, a distinction is made between a paraneoplastic form, acanthosis nigricans maligna, which is associated with adenocarcinomas and manifests itself predominantly palmar, plantar, on the tongue and oral mucosa, and acanthosis nigricans benigna, which occurs, among other things, in endocrinological disorders, such as insulin resistance, and manifests itself on the intertriginous areas. Because of this, malignancy exclusion is obligatory in all forms of acanthosis nigricans. Southern ethnic groups show this pseudoacanthosis nigricans in a cluster.
Bullosis diabeticorum (Fig. 7) is a rare spontaneous blistering of a few millimeters to several centimeters on the lower legs and/or feet that occurs in diabetic patients. This occurs predominantly in long-standing diabetes mellitus.

Diabetic foot syndrome is well known but often overlooked in clinical practice. Malum perforans has several precipitating factors, but the most important are peripheral sensorimotor neuropathy and microangiopathy. The typical deformation of the feet with pronounced hyperkeratosis and rhagades occurs. The maximum variant is the Charcot foot. The most important preventive measure is to educate patients about good foot/skin care, appropriately soft footwear, and avoiding sharp objects or walking barefoot, as well as daily self-inspection of the soles of the feet.
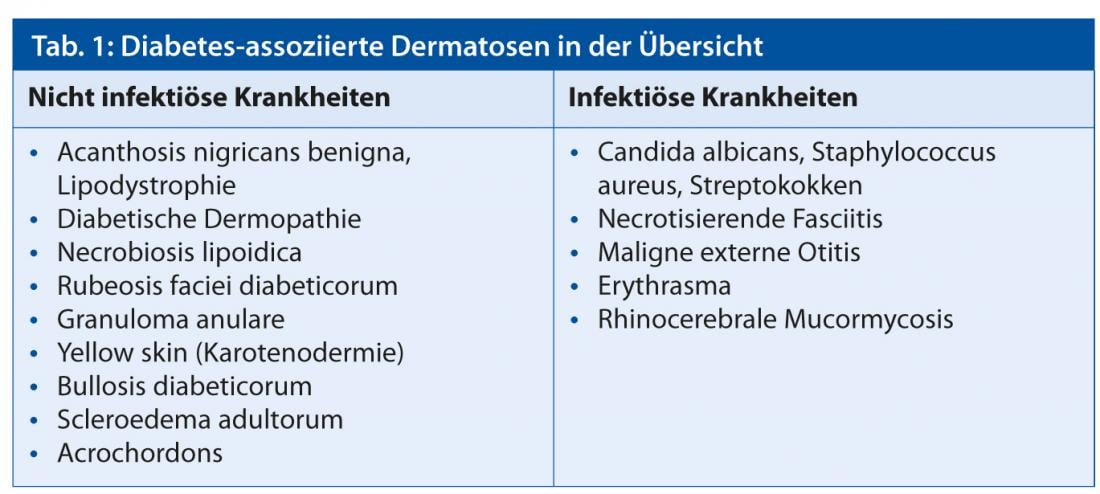
Scleroedema adultorum, which occurs predominantly in 2.5% of overweight diabetics, is characterized by marked thickening of the skin on the back and neck. An overview of diabetes-associated dermatoses is shown in Table 1.
In Cushing’s disease or prolonged steroid therapy, generalized atrophy of the skin, striae distensae, purpura, hypertrichosis, rubeosis faciei, acanthosis nigricans, and redistribution of adipose tissue with truncal adiposity and atrophy of the limb muscles are typically found.
Polycystic ovary syndrome (PCO) is one of the most common endocrinological disorders in childbearing women, with an incidence of 5-10%, and is characterized by elevated androgen and insulin levels. Thus, in the context of hyperandrogenism, one mainly finds hirsutism, acne vulgaris, and androgenetic alopecia. Acanthosis nigricans may manifest due to hyperinsulinemia.
Liver disease
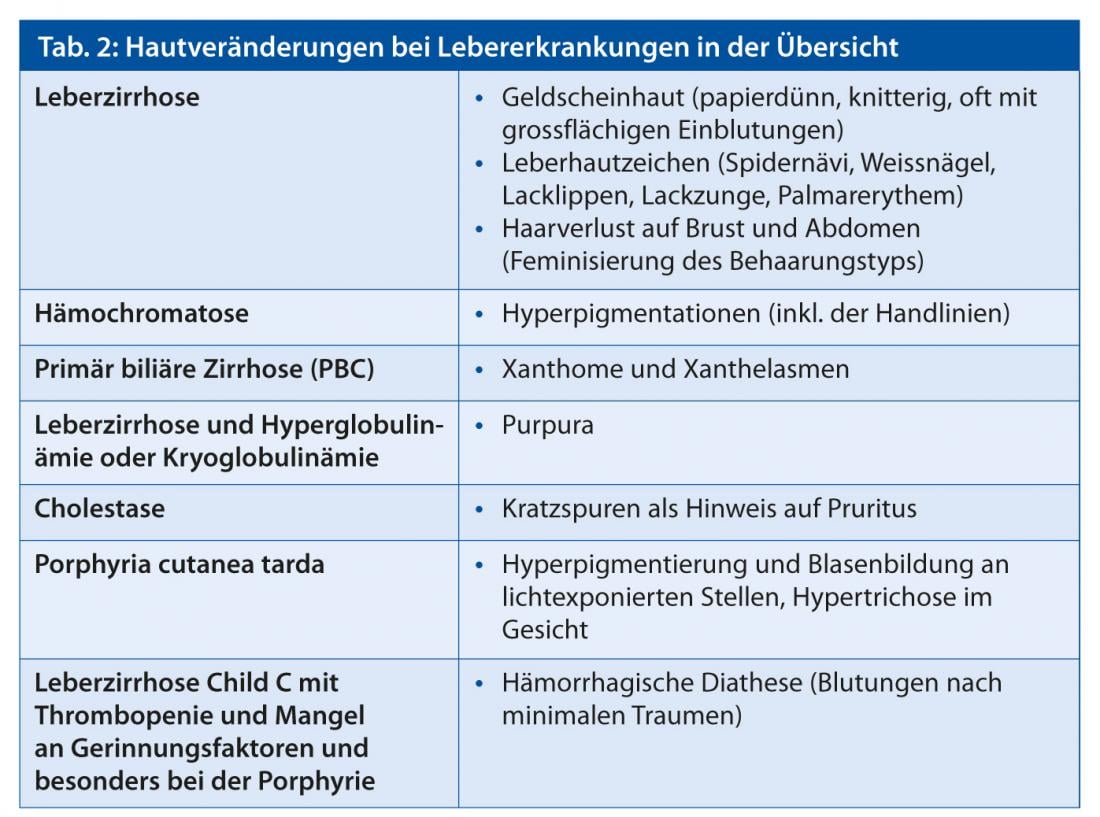
Acute or chronic liver damage often results in secondary skin manifestations. On the one hand, this may be due to a disturbed or altered metabolic function or to an immunological co-reaction.
The following skin diseases can be caused or triggered by acute or chronic hepatitis B/C:
- Vasculitis
- Erythema elevatum diutinum
- Systemic lupus erythematosus
- Lichen planus
- Pyoderma gangrenosum
- Urticariavasculitis
An overview of skin changes in liver disease is given inTable 2.
Chronic inflammatory bowel disease
Crohn’s disease is a chronic granulomatous disease that can affect the entire intestinal tract. Up to 70% of all patients develop perianal lesions, such as fistulas or abscesses. Perianal fissures, mariscs, and eczematous or ulcerative lesions are also more common. Perianal lesions may precede the disease as symptoms for years. Diagnostic colonoscopy is recommended for recurrent perianal fistulas. About half of the patients develop erythema, edema, and pustular lesions on the labia, penis, or scrotum. Polymorphous skin lesions in the context of infiltrated erythema, as grouped papulopustules or ulcerative infiltrates are found more frequently on the trunk and lower extremities. Diagnosis of cutaneous Crohn’s disease, i.e., without continuity with the gastrointestinal tract, is often difficult, especially in the absence of gastrointestinal symptoms. The course may be chronic or spontaneously healing. Enorally, often only very nonspecific lesions such as stomatitis or aphthous ulcers are found. The incidence for oral Crohn’s disease ranges from 0 to 9%.
Reactive dermatoses associated with Crohn’s disease include erythema nodosum, pyoderma gangrenosum, and Sweet syndrome. Erythema nodosum (Fig. 8) is the most common dermatosis occurring with Crohn’s disease and ulcerative colitis.

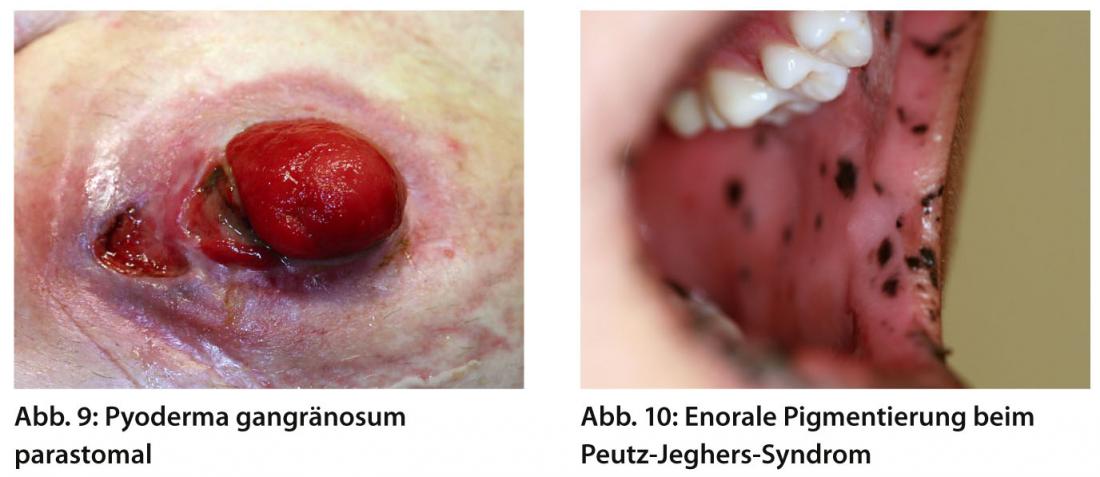
There are cutaneous-subcutaneous painful erythematous nodules, which typically occur on the extensor sides of the lower legs. Pyoderma gangrenosum occurs in 1-2% of patients with Crohn’s disease, and is slightly more common in ulcerative colitis. Clinically, there is often initial blistering or pustules with subsequent abscessing and painful ulceration. The localization is mainly on the lower extremities, but it can occur ubiquitously, clustered parastomally (Fig. 9).
Sweet’s syndrome clinically presents with reddish-livid, succulent, pressure-dolenous, infiltrating papules and confluent plaques associated with an antecedent decrease in general condition, accompanied by fever and histologically neutrophilic dermatitis of the affected skin areas.
Gastrointestinal tumor syndromes
The colorectal syndromes, which include hereditary colon carcinoma without polyposis (HNPCC), familial adenomatous polyposis (FAP), juvenile polyposis syndrome, and Peutz-Jeghers syndrome, have disease-specific skin changes that dermatologists should be aware of. In addition, early diagnosis of these diseases is also of great importance in view of the need for monitoring and prevention. HNPCC, also known as Lynch syndrome, is the most common hereditary form of colorectal cancer and affects approximately 5% of colorectal cancer cases. In a variant of this, Muir-Torre syndrome (MTS), the cutaneous changes occur in early adulthood, usually a decade before the onset of the internal malignancy. Sebaceous gland adenomas and epitheliomas are found mainly on the face and scalp and appear as yellowish papules and nodules. The sebaceous gland carcinomas usually originate from the Meibomian glands or Zeiss’ glands and due to this are mainly found on the eyelids as yellowish papules with a tendency to ulceration and locally aggressive growth. In about 20% of patients, sun-exposed areas also show a frequent occurrence of keratoacanthomas. If the diagnosis is confirmed, family screening is recommended, as well as regular colonoscopies (every 2-3 years) and an annual dermatological check-up.
Gardner syndrome represents a variant of FAP, with the development of multiple gastrointestinal adenomatous polyps, with consequently accelerated adenoma-carcinoma sequence. Indications are multiple epidermal cysts, especially on the face and extremities, and also on the trunk. Desmoid tumors, i.e. benign fibrous mesenchymal tumors that arise from well-differentiated fibroblasts and can be locally very aggressive, are found in approximately 10-14% of patients. Approximately half of desmoid tumors arise intraabdominally; extraabdominal locations include the chest, shoulder girdle, and inguinal.
In Peutz-Jeghers syndrome, 95% of patients present with typical lentiginosis of the lip, perioral, nose, buccal mucosa, hands, feet, and perianal areas, which manifests during childhood (Fig. 10) . Differential diagnosis should include Addison’s disease or Mc Cune-Albright syndrome. In Addison’s disease, there is a generalized brownish pigmentation with emphasis on the light-exposed areas as well as the axillae, nipples, and genital area. In Mc Cune-Albright syndrome, which is defined by the triad of fibrous dysplasia, pubertas praecox, and café-au-lait spots, characteristic café-au-lait spots with map-like hyperpigmentation of skin and mucous membranes have existed since birth.
Maja Wüest, MD
Prof. Dr. med. Peter Itin
Literature:
- Schmidt-Westhausen AM, et al: Mouth, pharynx, teeth and HIV. MED-INFO 2006; 59.
- Shashi, et al: Skin and Mucocutaneous Manifestations: Useful Clinical Predictors of HIV/AIDS. J Clin Diagn Res 2012 Dec; 6(10): 1695-1698.
- Eisman S, et al: Pruritic papular eruption in HIV. Dermatologic Clinics 2006 Oct; 24(4): 449-457.
- Fistarol SK, et al: Cowden disease or multiple hamartoma syndrome cutaneous clue to internal malignancy. Eur J Dermatol 2002; 12: 411-421.
- Henschel, et al: Crohn’s disease-associated dermatoses. Dtsch Arztbl 2002; 99(50): 3401-3410.
- Lauren, et al: Dermatologic manifestation of diabetes. Journal of Diabetes 2012; 4: 68-76.
- Meurer M, et al: Skin changes in diabetes mellitus. Dermatologist 2004 Apr; 55: 428-435.
- Intekhab A, et al: Diabetes mellitus. Clinics in Dermatology 2006; 24: 237-246.
- Prague, et al: Cushing’ syndrome. BMJ 2013 Mar 27; 346: f945.
- Lee, et al: Dermatologic manifestation of polycystic ovary syndrome. Am J Clin Dermatol 2007; 8(4): 201-219.
- Kejal R, et al: Cutaneous manifestations of gastrointestinal disease: part I. J Am Acad Dermatol 2013 Feb; 68(2): 189.e1-21.
- Breck Thrash, et al: Cutaneous manifestations of gastrointestinal disease: Part II. J Am Acad Dermatol 2013 Feb; 68(2): 211.e1-33.
- Anders D, et al: Muir-Torre syndrome. Dermatologist 2012; 63: 226-229.
DERMATOLOGIE PRAXIS 2013; No. 5: 10-13.











