The scientific evidence that the development of epithelial skin tumors as well as melanomas can be effectively prevented with consistent sun protection measures is opposed by various fears in the population regarding side effects and risks of sun protection products. In particular, there are reports of possible hormonal activity of chemical sunscreen filters, the question of the safety of physical filters in the nano-size range, and, last but not least, concerns about possible vitamin D deficiency in the growing skeleton under rigorous sunscreen measures. The purpose of this article is to highlight the current data situation with regard to the aforementioned questions and to make recommendations for daily practice.
That UV radiation leads to the induction of malignant skin tumors is well known and well documented. Both UVB (wavelength 280-320 nm) and UVA (320-400 nm) have carcinogenic properties. The latter is also central in skin aging processes.
Severe sunburns in childhood represent one of the most important modifiable risk factors for melanoma [1], which continues to have an increasing incidence and poor prognosis in advanced stages. While for epithelial skin tumors (basal cell carcinoma, spinocellular carcinoma) the data regarding a positive influence of regular use of sunscreens on tumor development is relatively clear, uncertainty prevailed for a long time with regard to melanoma. Recently, however, the first randomized controlled trial has been published, which documented a clear reduction in melanoma incidence with consistent use of sunscreens [2].
In this light, it is surprising that knowledge of these relationships is still very limited in the general population and especially among children and adolescents. A recent survey of schoolchildren in northwestern Switzerland found that only one-third of respondents had a good knowledge of sun protection and risks [3]. More than half of the participants also experienced at least one sunburn in the year prior to the survey, and despite older students’ better knowledge, they were much less likely to consistently protect themselves from UV radiation than younger respondents. Moreover, it seems that parents protect their children especially in high-risk situations (staying at the beach), while daily sun exposure (playing in the garden) is neglected [4]. However, the latter accounts for a large part of the cumulative UV dose. These facts make it clear that the topic of sun protection must have a permanent place in routine pediatric check-ups as well as in every dermatological consultation.
Sunscreen – effect and possible risks
Exposure prophylaxis is the top priority when it comes to sun protection, both in children and adults. In addition to seeking shade during the midday hours (11-15 hours), children should pay particular attention to covering as large a part of the body as possible with light clothing, whereby the UV protection of dark clothing is better compared to white clothing and the protection of wet clothing tends towards zero. More and more often, clothes with built-in sun protection are also available at major distributors. Likewise, sunglasses and hat are mandatory.
In addition, sunscreens, which are available in all conceivable galenics, play an important role. These are divided into organic filters, which cause absorption of UV radiation, and physical filters, which result in reflection and scattering of radiation [5].
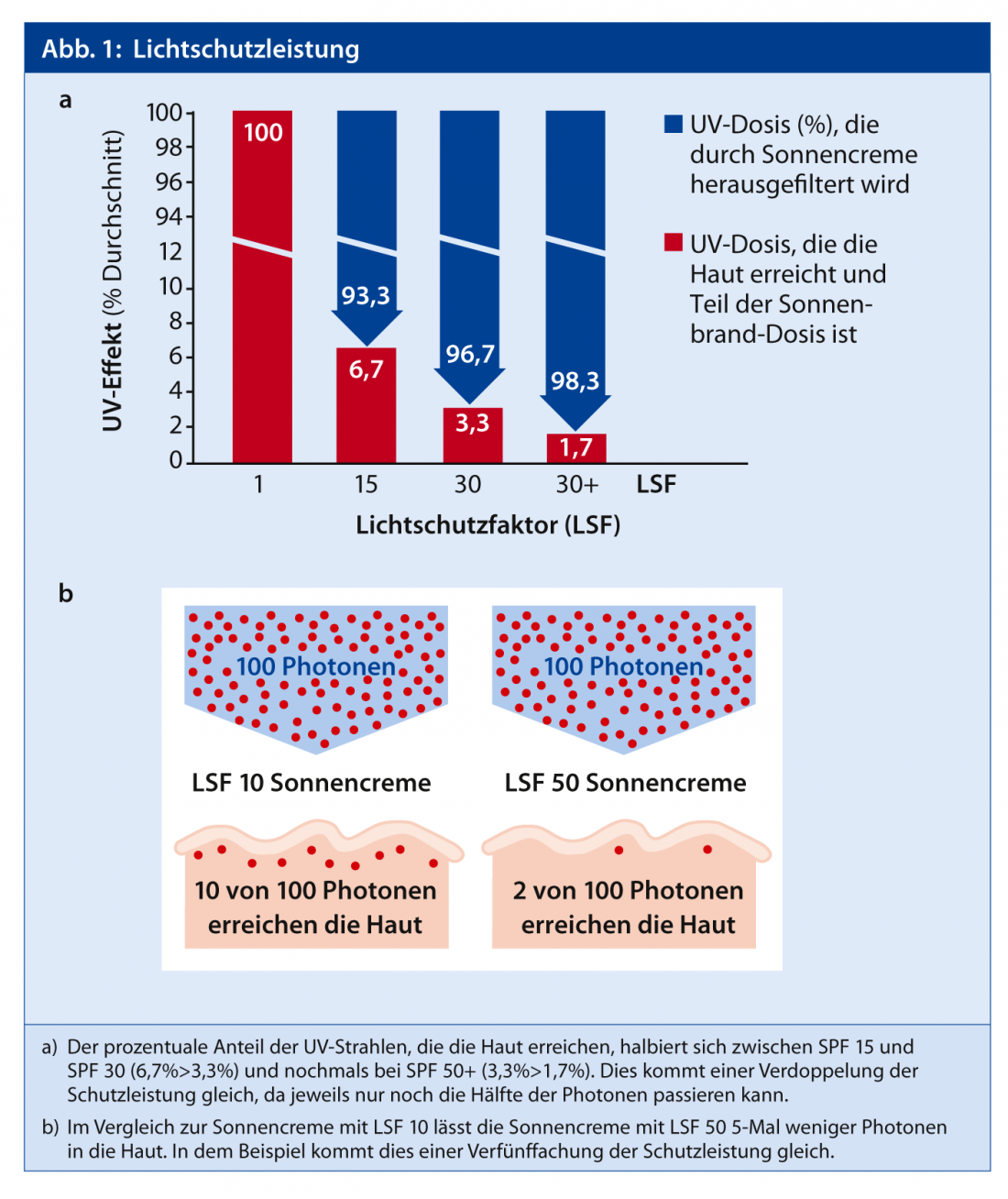
The required level of sun protection factor (SPF) is controversial. Officially, the American Academy of Pediatrics (AAP) recommends the use of a product with SPF 15 or more [6], while dermatological societies call for much higher protection factors. SPF is the quotient of erythema threshold time with sunscreen divided by erythema threshold time without sunscreen. Unfortunately, there are many incorrect opinions about what these numbers actually say. For example, it is often assumed that the protective performance does not double or quadruple from SPF 15 to SPF 30 or SPF 60, because the percentage of UV radiation filtered out (absorbed) only increases by 5%. This means: The protective performance improves only insignificantly with increasing sun protection factor. However, the protective performance does not refer to the radiation filtered out (absorbed), but to the radiation that actually reaches the epidermis/dermis. With SPF 15, approx. 6.7%, with SPF 30 approx. 3.3% and with SPF 60 approx. 1.7% of the UV radiation reaches the epidermis/dermis – this corresponds to a doubling or quadrupling of the light protection performance. (Fig. 1, as well as www.youtube.com/watch?v=8cc8qRr7oMQ).
These facts, together with the observation that the applied amount of sunscreen is in reality less than half of the recommended amount of 2 mg/cm2 used in the tests, suggest that the use of a product with at least SPF 30 is reasonable. For example, the recommended amount of sunscreen for an 8-year-old girl to treat the entire integument with a body surface area of 0.85 m2 is a good 16 g, which is about the size of a golf ball. In addition, products in which the UVA protection is at least one third of the SPF are preferable. The latter are marked with the UVA signet (Fig. 2) .

Repeated reports of relevant systemic absorption and hormonal activity of organic sunscreen filters made headlines in recent years.
The compounds benzophenone-3 (oxybenzone), octyl methoxycinnamate and 3-(4-methyl-benzylidene)camphor are particularly affected, with the majority of data coming from in vitro studies. A clinical study in 32 adults showed that all compounds were absorbed when applied over a large area, with the absorption rate being greatest for benzophenone-3 [7]. A relevant influence on sex hormone levels has not been demonstrated despite large-area and high-dose application, although the risk may be higher in very young children due to the less favorable body surface-to-weight ratio and more immature metabolic systems. For this reason, it is probably sensible to use products without the filters mentioned, especially benzophenone-3, during the first years of life, although it should be noted that this compound is also present in many other cosmetics, such as hair shampoos. The ingredients of most sunscreens and other cosmetics can be conveniently accessed at www.codecheck.info.
In addition, organic sunscreen filters can cause skin irritation and rarely photoallergic reactions.
These reasons have led to the recommendation by us, as well as by various other bodies, to use only physical sunscreen filters (titanium dioxide, zinc oxide) in the first year of life, although this is not based on hard data. Recently, the particle size of the physical filters has also been gradually reduced in order to reduce the undesirable “whitening” effect of the products. The particle size is now in the nanoscale, which in turn raised concerns about safety. However, various studies have failed to demonstrate permeation beyond the stratum corneum, so these compounds should probably be considered safe [8].
Sun protection and vitamin D
In recent years, there has been growing evidence that vitamin D has much more far-reaching effects in the human body than previously thought. Most of the active vitamin D is produced under the influence of UV-B in the skin. Several studies have shown that the consistent use of sunscreens leads to a relevant reduction in systemic vitamin D levels. However, the study conditions are unlikely to have corresponded to “real-world conditions” and sun protection measures do not lead to a relevant decrease in vitamin D levels in most individuals in everyday life [9]. This is in contrast to special situations such as patients with xeroderma pigmentosum or oculocutaneous albinism, where maximum sun protection and thus controls of vitamin D levels are certainly indicated.
Since UV radiation is an important carcinogen, recommendations by certain experts for daily short-term unprotected sun exposure should be firmly rejected and vitamin D supplementation should be preferred. In this context, the new recommendations of the Federal Office of Public Health (FOPH) to extend vitamin D substitution to the first three years of life are very welcome (www.bag.admin.ch/themen/ernaeh rung_bewegung/05207/13246/index.html).
Specific recommendations for sun protection in children
- Sun protection measures (stay in the shade where possible, clothing, sunscreen with at least SPF 30) should be taken whenever you are outdoors.
- Avoid direct sunlight until six months of age. If impossible, localized application of sunscreen.
- In the first years of life, purely physical filters are preferable.
- Sunscreen in sufficient quantity and apply sufficiently often, about every two to three hours, especially after bathing or playing in the sand (abrasion). For this reason, combination products with repellents (DEET) should be rejected.
- Vitamin D substitution according to FOPH recommendations. In situations of risk for hypovitaminosis D, appropriate level determinations are recommended.
Literature:
- Russak JE, Rigel DS: Risk factors for the development of primary cutaneous melanoma. Dermatologic clinics 2012; 30: 363-368.
- Green AC, Williams GM, Logan V, Strutton GM: Reduced melanoma after regular sunscreen use: randomized trial follow-up. J Clin Oncol 2011; 29: 257-263.
- Reinau D, Meier C, Gerber N, Hofbauer GF, Surber C: Sun protective behaviour of primary and secondary school students in North-Western Switzerland. Swiss Med Wkly 2012; 142: w13520.
- Li J, Uter W, Pfahlberg A, Gefeller O: A comparison of patterns of sun protection during beach holidays and everyday outdoor activities in a population sample of young German children. Br J Dermatol 2012; 166: 803-810.
- Quatrano NA, Dinulos JG: Current principles of sunscreen use in children. Current opinion in pediatrics 2013; 25: 122-119.
- Section on D, Balk SJ: Ultraviolet radiation: a hazard to children and adolescents. Pediatrics 2011; 127: 588-597.
- Janjua NR, Mogensen B, Andersson AM, et al: Systemic absorption of the sunscreens benzophenone-3, octyl-methoxycinnamate, and 3-(4-methyl-benzylidene) camphor after whole-body topical application and reproductive hormone levels in humans. J Invest Dermatol 2004; 123: 57-61.
- Newman MD, Stotland M, Ellis JI: The safety of nanosized particles in titanium dioxide- and zinc oxide-based sunscreens. J Am Acad Dermatol 2009; 61: 685-692.
- Norval M WH: Does chronic sunscreen use reduce vitamin D production to insufficient levels? Br J Dermatol 2009; 161: 732-736.
DERMATOLOGIE PRAXIS 2013; no. 2: 4-6











