In most cases, it is not enough to simply recommend more exercise or activity for COPD patients. An indication-specific training control based on objective and subjective disease and performance parameters during exercise can be decisive for the course of the disease already in the early stages and becomes more important with the severity of the disease. Inevitably, targeted exercise management and exercise-related patient education within an interdisciplinary program become mainstays of rehabilitation in COPD.
In practice, the severity of obstruction in COPD is not a clear predictor of low exercise capacity, quality of life, or patient mobility . The function and performance of the skeletal musculature and how much the patient knows about his disease and how he deals with it are also decisive factors. The necessity as well as the chances of physical activity in COPD are undisputed and evidently proven [1]. However, a well-structured and adapted training introduction that avoids frustration is crucial for sustainable success and patient acceptance of the autonomous implementation of targeted training sessions. For it is also these negative experiences that have led the patient, via insecurity and fear, into the cycle of inactivity and deconditioning.
Physiological background
The performance of patients with obstructive airway disease may be limited by the obstruction itself and the increased work of breathing associated with it. In addition, performance is limited by dynamic overinflation of the lungs with increased ventilation. In addition, the respiratory muscles are often fatigued by chronic overload and respiratory gas exchange is impaired [2]. With regard to the peripheral musculature, the changes can be observed particularly well in the quadriceps femoris muscle. In advanced stages, atrophy is seen in the type I fibers, and as the disease progresses, there is a compensatory increase in type IIb fibers, resulting in a lower aerobic capacity of the muscles [3–5]. Furthermore, it is discussed that fatigued respiratory muscles reflexively support sympathetic vasoconstriction and inhibit blood flow to the working muscles of the extremities [4]. The result in each case is rapid fatigue and reduced performance.
A decisive factor, also for motivation and compliance of the patient, appears to be the fact that the changes in the peripheral musculature and thus also the symptoms of reduced performance can be described as partially reversible. This is because the changes in the musculature are not a direct consequence of the disease, but secondary to dyspnea-related inactivity. This gives the patient a realistic prospect of noticeably improved performance.
Training control depending on multiple factors
In the early stages or with only minor to moderate physical limitations, regular independent endurance training in the continuous method may be sufficient to maintain performance. As the disease progresses, systematically controlled training becomes increasingly important and can certainly be described as a challenge. Diagnostic disease parameters such as lung function values, pulse oximetry and results of exercise ergometry, as well as compliance, motivation, exercise tolerance and training experience of the patient must be taken into account in the selection of training method, extent and intensity.
In advanced stages of COPD, significantly reduced local energy stores (ATP, glucose, creatine phosphate) also limit performance and, in conjunction with a constantly elevated muscle lactate level, lead to rapid fatigue [4]. If a constant load cannot be maintained over a longer period of time during training, interval training is a suitable alternative to the continuous method. Various authors found comparable performance improvements with interval training in different stages of COPD, which was also associated with significantly higher feasibility and compliance compared with the continuous method [6, 7]. A decisive advantage compared to the continuous method is not only a prolonged training time, but also the increased stimulus on the peripheral skeletal muscles.
Global Insufficiency Training
In the case of chronic respiratory global insufficiency, adapted and controlled exercise management is particularly important, since increased ventilation is already present at rest, often leading to lactic acidosis in both the respiratory support muscles and peripherally. This is amplified with the slightest exertion, so that, strictly speaking, the patient is already in a state of overtraining without physical activity around the clock. However, this is not a general contraindication for physical training. However, to set the stage for training, noninvasive ventilation (e.g., BiPAP) can also be used in training [8]. If the breathing mask is tolerated by the patient during exertion, effective training of the peripheral muscles can be achieved by unloading the respiratory muscles [9].
The training control criteria presented in Table 1 are based on data from various authors as well as on practical experience.

Strength training – only a supplement?
The clinical changes in skeletal muscle described above alone provide a physiological rationale for targeted strength training of local muscle groups. The literature still lacks concrete statements on intensity and scope in the implementation of strength training [10], but the positive effects on muscle mass, strength and quality of life are considered certain. The authors agree that individual strength training adapted to the patient’s everyday profile supports and sustainably stabilizes the effects of training therapy measures [10, 11]. Figure 1 shows the training start on the bicycle ergometer. Here, objective as well as subjective factors can be well controlled and monitored during training. In addition to instruction, the therapist is also responsible for counseling and motivation.

Fig. 1: Training start on the bicycle ergometer
Place of O2 substitution in training.
The administration of oxygen under stress may well be considered necessary or mandatory, especially in the advanced stages of COPD [12]. This is especially true for patients who are already being treated with long-term oxygen therapy or who suffer from concomitant or secondary cardiac diseases (cor pulmonale, heart failure) [13].
Intensive training with already fatigued respiratory support muscles can be expected to result in a massive decrease in performance of the working skeletal muscles, presumably also due to an emerging competitive situation between working peripheral muscles and respiratory support muscles for cardiac output [4].
The additional administration of oxygen during training with the aid of nasal oxygen goggles is handled very differently in practice. Various authors found a positive effect of oxygen administration during training in recent studies [12]. Reduced lung overinflation, lower lactic acid production, and measurably reduced respiratory rate with increased expiratory time can result in higher exercise intensity and thus maximize exercise progress. Thus, facilitating the work of breathing may allow for more effective training of the peripheral muscles. The fact is that nasally administered oxygen should be considered a medication and thus used in the minimum necessary dosage. Since many Swiss rehabilitation clinics are located at altitude, oxygen administration under stress takes on additional importance.
Education and motivation
Exercise therapy interventions, especially in severe COPD, require great compliance on the part of the patient. The high intensity of the training combined with a lack of training experience and tolerance can lead to mental overload of the patient. It is therefore of great importance to inform the patient in advance not only about the necessary intensity and the positive consequences of the training, but above all to awaken his motivation and self-efficacy [14]. Often, it is through the patient’s understanding and confidence in the exercise therapy intervention (and in the therapist him/herself) that training at the required intensity is possible.
Through targeted eduction, fear and uncertainty during exertion can be reduced, and dyspnea and exhaustion during exercise are accepted as the body’s normal response to exertion. Especially patients without training experience find it difficult at the beginning of the intervention to be able to assess a load and to recognize the limits of their own physical capacity. This makes the experience of the supervising therapist and the intensity control through preceding performance tests all the more important.
Numerous studies in both inpatient and outpatient settings have examined the effectiveness of patient education in COPD. Patients who received training had up to 85% fewer physician visits the following year [15, 16]. Similarly, hospitalization rates were significantly reduced compared with patients who did not receive training [17, 18]. Other authors report a higher quality of life in trained patients even after one year [15, 19]. In addition, a sustained lower BODE index as well as a lower antibiotic requirement in trained patients can also be expected [18]. From a health economic perspective, targeted patient education can significantly reduce disease costs and morbidity [15, 19].
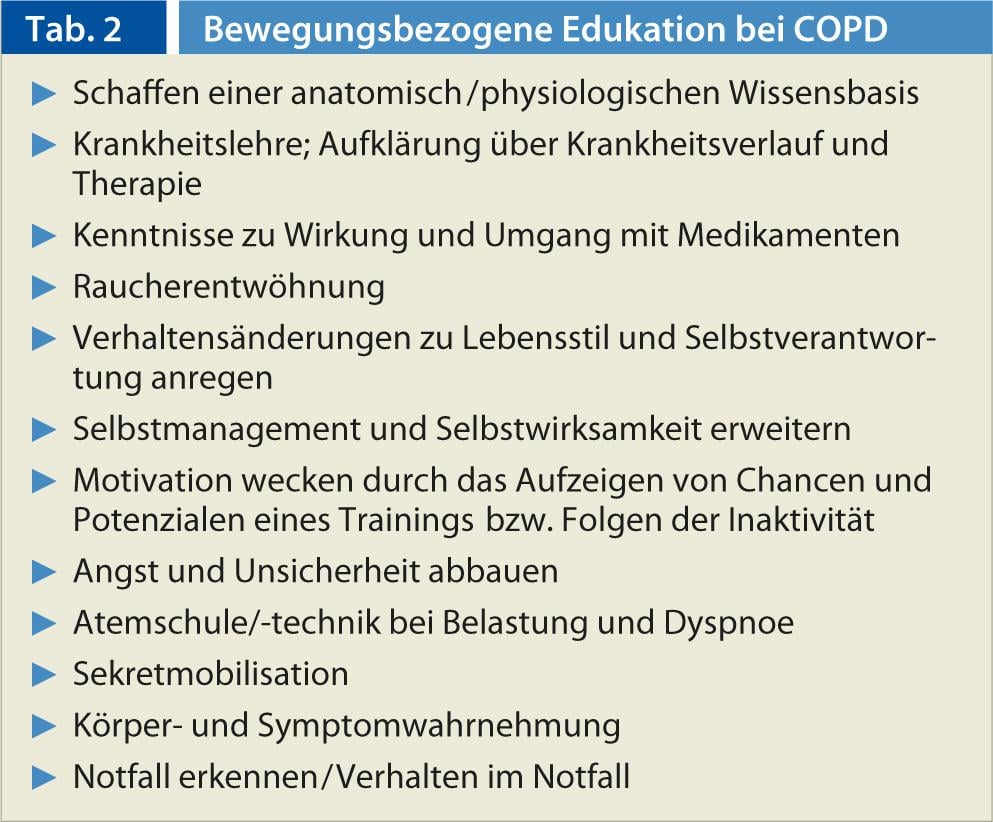
Table 2 summarizes the key contents of targeted patient education.
Implementation in an interdisciplinary setting
Even though targeted physical training is referred to here as a pillar of rehabilitation, this is only effective in the long term if it is taught in an interdisciplinary setting. Various respiratory therapy interventions, which lack any evidence as an isolated treatment measure [20], have important tasks in the interdisciplinary context, since they can not only increase the well-being of the patient, but also create the basis for adequate behavior under stress to increase the stress tolerance of the patient. In addition, it is often only when the patient is optimally adjusted to medication that training can be carried out (see article by Dr. med. Thomas Rothe). The absolutely necessary smoking cessation as well as lifelong instructions for self-management by experts from various disciplines (medication, nursing measures, inhalation, infection prophylaxis, psychological support) are also at the center of an interdisciplinary rehabilitation (see article by Nadja Wyrsch).
The challenge now is to communicate all the measures to the patient without overwhelming him.
transfer to everyday life
It cannot be assumed that a patient will internalize the training control content described above in detail and later continue it in an independent training session. From experience, a long-term increase in activity in everyday life after completion of inpatient rehabilitation is also not to be expected if the patient does not return to everyday life with clear ideas and a concrete plan for continuing the training. For this reason, outpatient programs for stabilization and continuation of training have a high priority. In addition, the social environment should be involved in the process and motivated to actively support the patient.
CONCLUSION FOR PRACTICE
- Intensively educate and motivate patients and explain the consequences of inactivity
- Establish exercise and targeted training already in the early stages of COPD
- Enforce smoking cessation as an absolute necessity
- Take fears and uncertainty seriously and clarify them
- Refer to accredited exercise programs if noticeable increase in inactivity and uncertainty (Swiss Society of Pneumology, www.pneumo.ch)
- Involve social environment and family
- Support early intervention through inpatient stays
Silvio Catuogno
Sandra Brülisauer
Literature:
- Meyer, A, et al: German Journal of Sports Medicine 2007; 58(10): 351-356.
- Worth H, et al: Pulmonology 2000; 54(2): 61-67.
- Hughes RL, et al: Respiration 1983; 44(5): 321-328.
- Dempsey JA, et al: German Journal of Sports Medicine 2000; 51(10): 318-326.
- Schultz K, et al. (Ed.): Exercise therapy in COPD. Dustri-Verlag, Dr. Karl Feistle, Munich 2012.
- Beauchamp, et al: Thorax 2010; 65: 157-165.
- Puhan MA, et al: Thorax 2005; 60: 367-375.
- Gerdes A: BiPAP® – Biphasic Positive Airway Pressure, 2005, www.intensivcareunit.de/bipap.html.
- Reuveny R, et al: Isr Med Assoc J 2005; 7(3): 15.
- Frey M: Strength training in COPD – what is secured?, in: Schultz K, et al. (eds.): Training therapy in COPD. Dustri-Verlag, Dr. Karl Feistle, Munich 2012.
- Mador MJ, et al: Chest 2004; 125: 2036-2045.
- Emtner M, et al: Am J respir Crit Care Med 2003; 168: 1034-1042.
- Williams PT: Arch Int Med 1998; 158: 237-245.
- Jonas S, Phillips EM.: ACSM`s Exercise is medicin. A clinician`s guide to exercise prescription. American College of Sports Medicine (ed.). Wolters Kluwer/Lippincot Williams & Wilkins, Philadelphia, 2009.
- Wittmann M, et al: Pneumology 2007; 61: 636-643.
- Gallefoss F, Bakke PS: Respiratory Medicine 2000; 95: 279-287.
- Effing T, et al: The Cochrane Collaboration 2009.
- Bösch D, et al: Pulmonology 2007; 61(10): 629-635.
- Gallefoss F: Patient Education and Counseling 2004; 52(3): 259-266.
- Holland AE, et al: Cochrane Database Syst Rev. 2012 Oct 17;10:CD008250. doi: 10.1002/14651858.CD008250.pub2.
- Göhl O: Methodology of endurance training in COPD, in: Schultz K, et al. (Ed.): Exercise therapy in COPD. Dustri-Verlag, Dr. Karl Feistle, Munich 2012.











