Retroperitoneal liposarcomas are often discovered as an incidental finding. The most common subtypes of sarcomas in the retroperitoneum are dedifferentiated liposarcomas, well-differentiated liposarcomas and leiomyosarcomas. Complete surgical resection is the standard treatment for retroperitoneal soft tissue sarcomas. Contrast-enhanced cross-sectional imaging is required before such an intervention in order to assess the extent of the tumor, vascular supply and vascularization of the sarcoma.
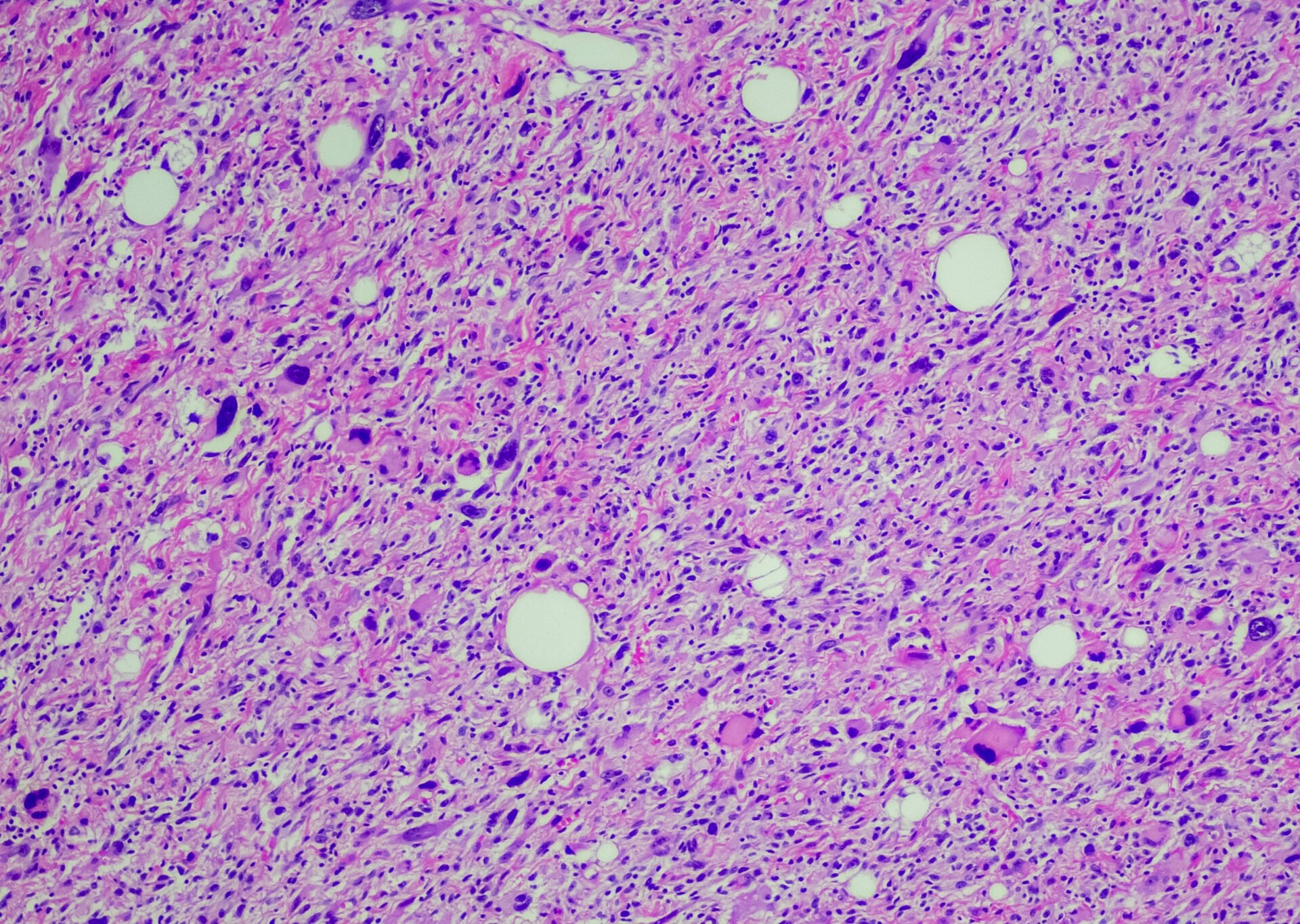
Highly differentiated liposarcoma, the most common type of liposarcoma, is a slow-growing, painless tumor that is usually located in the retroperitoneum, back or extremities. It consists of proliferating mature adipocytes [1–3,6]. The incidence is around 1:200,000 per year. It accounts for 20% of all malignant tumors of the soft tissues but only 1% of all malignancies. Like retroperitoneal fibrosis, this malignancy affects men more frequently than women, but the age of onset is slightly higher at 50-60 years. Infestation of children and adolescents is rare. It was first described in 1857 by Rudolf Virchow. Metastasis is usually found in the lungs and liver, less frequently in the peritoneum, diaphragm or pericardium. Lymphogenic filiae are less common [4].
Differential diagnoses include benign lipoma, other types of sarcoma, inflammatory myofibroblastoid tumor and Castleman’s disease. Metastatic testicular tumors, extragonadal germ cell tumors, lymphomas, paragangliomas and pheochromocytomas should also be ruled out.
Central necrosis, hemorrhages and calcifications are often found in the tumor.
The symptoms are non-specific, with pain and an unpleasant feeling of pressure in the affected area. In addition, general symptoms may occur, in about 20% of cases a B symptomatology. Fatigue and impaired physical and mental performance as well as impaired consciousness, dizziness or visual disturbances can also occur.
In addition, there is a slight fever in which the body temperature can rise to 38 degrees Celsius. Initially, weight gain may occur [7], but in the long term patients often lose weight and subsequently suffer from deficiency symptoms, for example feelings of weakness and skin irritation. Externally, a soft tissue tumor can manifest itself through paleness and a generally sickly appearance. The symptoms usually develop over the course of months and are often only recognized when the liposarcoma has already grown considerably.
If the tumor is located in one of the extremities, complete removal is often a cure. Sarcomas in the retroperitoneum and groin are more difficult to treat and are more likely to recur locally and develop into a dedifferentiated liposarcoma. If the tumor cannot be surgically removed or the removal was not complete, systemic therapies and radiation can be added, although their effectiveness is rather limited. Clinical trials are underway to investigate new forms of therapy for patients with advanced, inoperable disease (CDK4 and MDM2 inhibitor trials). Myxoid liposarcoma is low-grade malignant and exhibits high radiosensitivity. The prognosis is relatively favorable with a 5-year survival rate of around 70%. Pleomorphic liposarcoma is highly malignant and has a very poor prognosis with a 5-year survival rate of around 20%.
In retroperitoneal liposarcoma, the probability of being free of recurrence for 5 years is only 54%, while the 5-year survival rate is 80-90%. Various studies have concluded that patients taller than 30 cm and weighing 20 kg or more have a significantly higher risk of recurrence [6].
X-ray examinations are of little value in the diagnosis of retroperitoneal liposarcoma.
Sonography often shows a very variable echogenicity in retroperitoneal masses, which rarely allows a clear tumor diagnosis. Completely anechoic processes with dorsal sound amplification indicate cysts. The vascularization can be visualized by Doppler sonography [5].
Computed tomography and magnetic resonance imaging are the imaging techniques of choice for visualizing retroperitoneal sarcomas. By quantifying the tissue density in CT and especially the fat-suppressing sequences in MRI, the differential diagnoses can be narrowed down. The overall extent of the tumor can also be precisely determined, the relationship to the neighboring organs can be shown and functional limitations of the urinary system can be assessed.
Case study
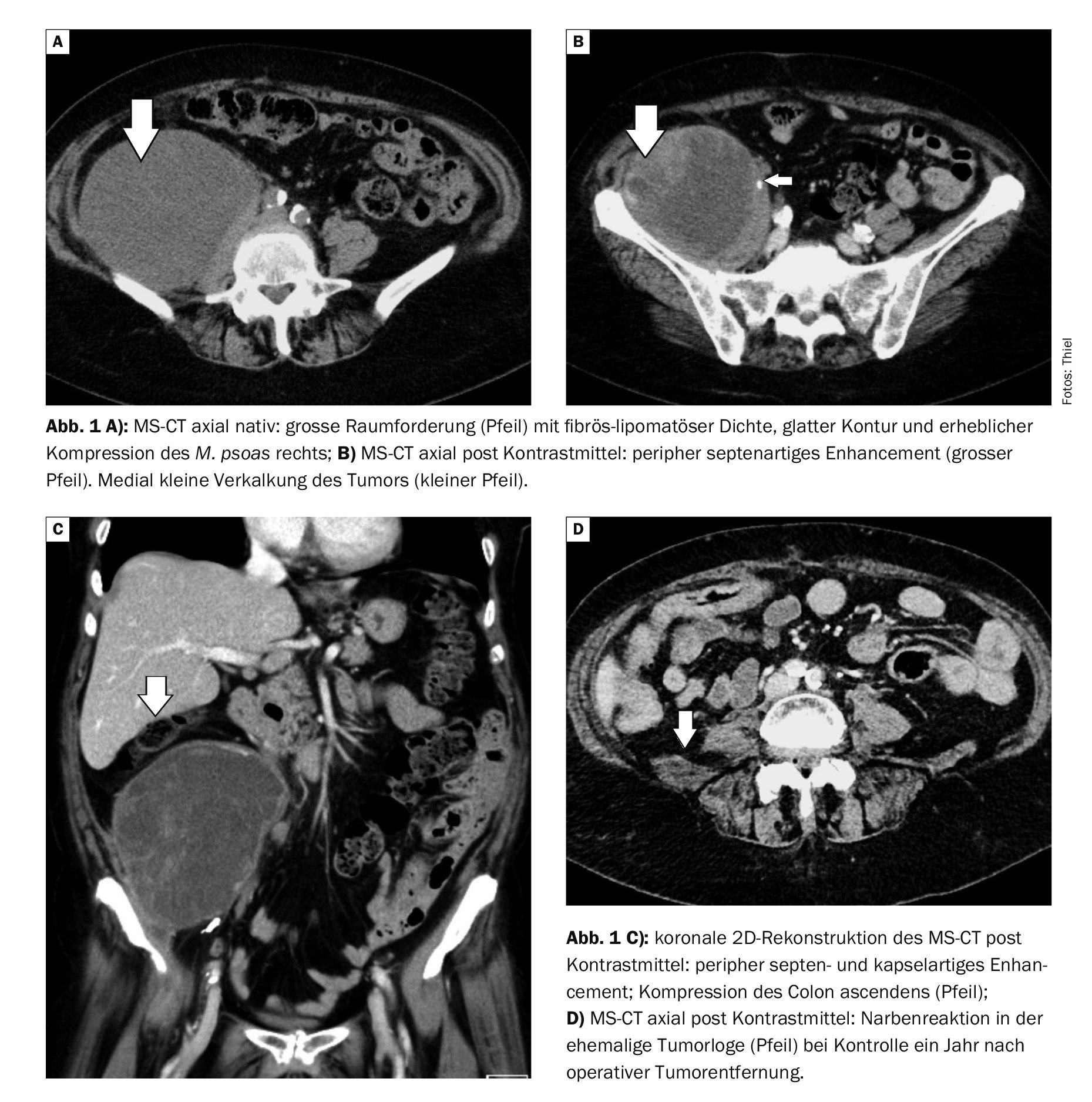
In case example 1 (Fig. 1A to 1D), a 57-year-old female patient complained of increasing pain in the lower abdomen. The symptoms were accompanied by undulating subfebrile temperatures and gradual weight loss. Sonographically, a mass was seen that could not be further verified. Computed tomography showed a tissue proliferation measuring approx. 14 × 11 × 10 cm in the right middle to lower abdomen with an inhomogeneous structure and marked peripheral, partly septal contrast enhancement. The retroperitoneal fatty tissue showed streaky thickening.
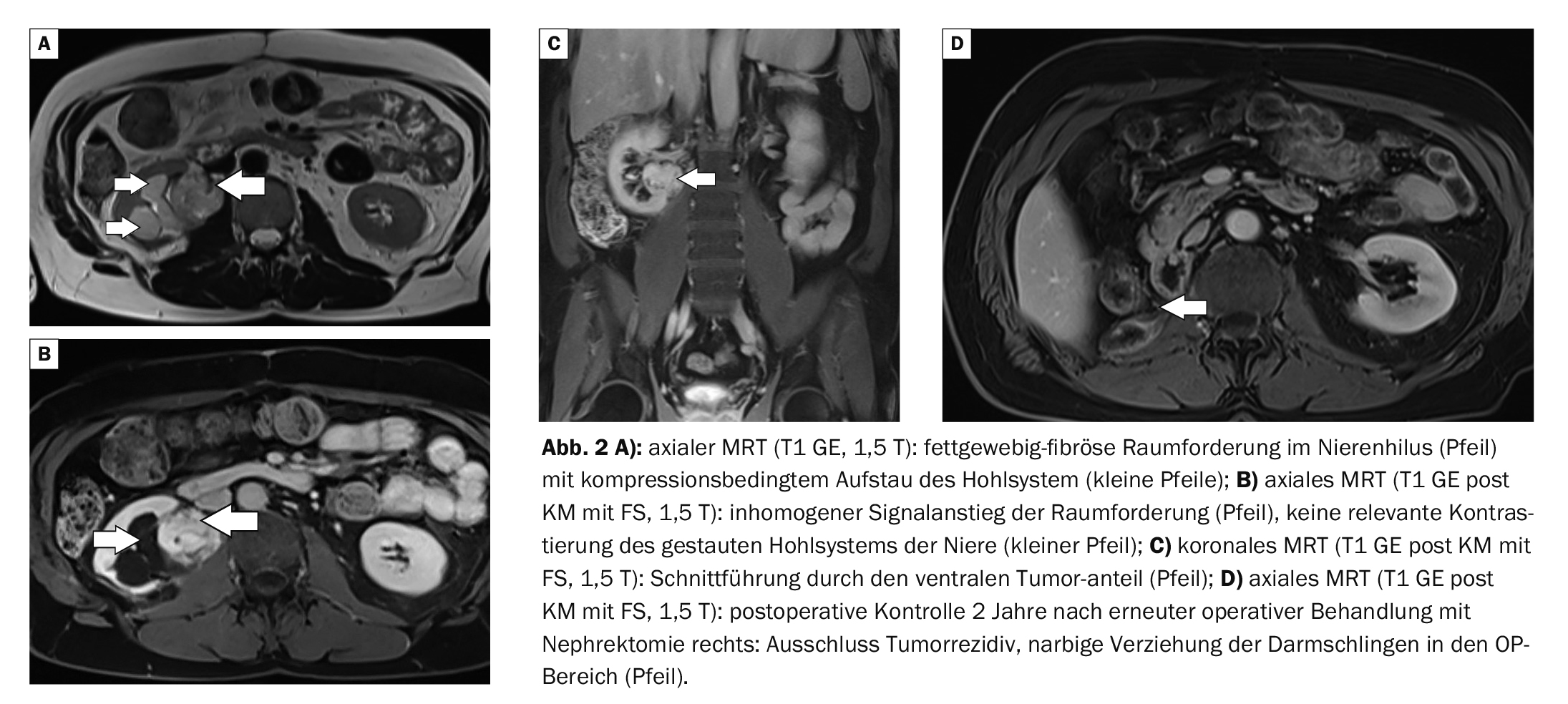
Case 2 demonstrates (Fig. 2A to 2D) the diagnosis of a recurrence of a retroperitoneal liposarcoma that was primarily operated on in September 2017. After a year, a urinary stasis kidney developed on the right. The abdominal MRI revealed a tumor recurrence infiltrating the psoas muscle and compressing the renal pelvis with consecutive urinary retention. A further check-up two years after the second operation with right nephrectomy ruled out a recurrence.
Take-Home-Messages
- At around 20%, liposarcomas account for a relatively large proportion of all
malignant soft tissue tumors. - Men are preferentially affected.
- Metastasis occurs mainly hematogenously in the lungs and liver.
- The symptoms are non-specific and can be wide-ranging.
- Imaging diagnostics are primarily performed using CT and MRI.
- Surgical removal of the tumor is the primary treatment option.
Literature:
- “Liposarcoma”, https://medlexi.de/Liposarkom,(last accessed 22.01.2024)
- “Liposarcoma”, https://flexikon.doccheck.com/de,(last accessed 22.01.2024)
- “Liposarcoma”, www.orpha.net/consor/cgi-bin,(last accessed 22.01.2024)
- Manski D: Urologielehrbuch.de, www.urologielehrbuch.de,(last accessed 22.01.2024)
- “Retroperitoneal sarcoma”, www.urologielehrbuch.de,(last accessed 22.01.2024)
- Marjiyeh-Awwad R, Mansour S, Khuri S: Giant Retroperitoneal Liposarcoma: Correlation Between Size and Risk for Recurrence. World J Oncol 2022; 13(5): 244-248.
- Marjiyeh-Awwad R, et al: Retroperitoneal Liposarcoma: The Giant Type. J Med Cases. 2022; 13(10): 517-520.
FAMILY PHYSICIAN PRACTICE 2024; 19(2): 31-33