The first case study concerns a young woman with papulopustular acne for whom teledermatology treatment proved to be effective. After around a year of treatment, the patient is now largely acne-free. The second case study of a woman with diabetic nephropathy shows that patients on dialysis can also develop severe forms of acne. The acne nodulocystica in this patient could be treated efficiently and safely with a “low-dose” isotretinoin therapy.
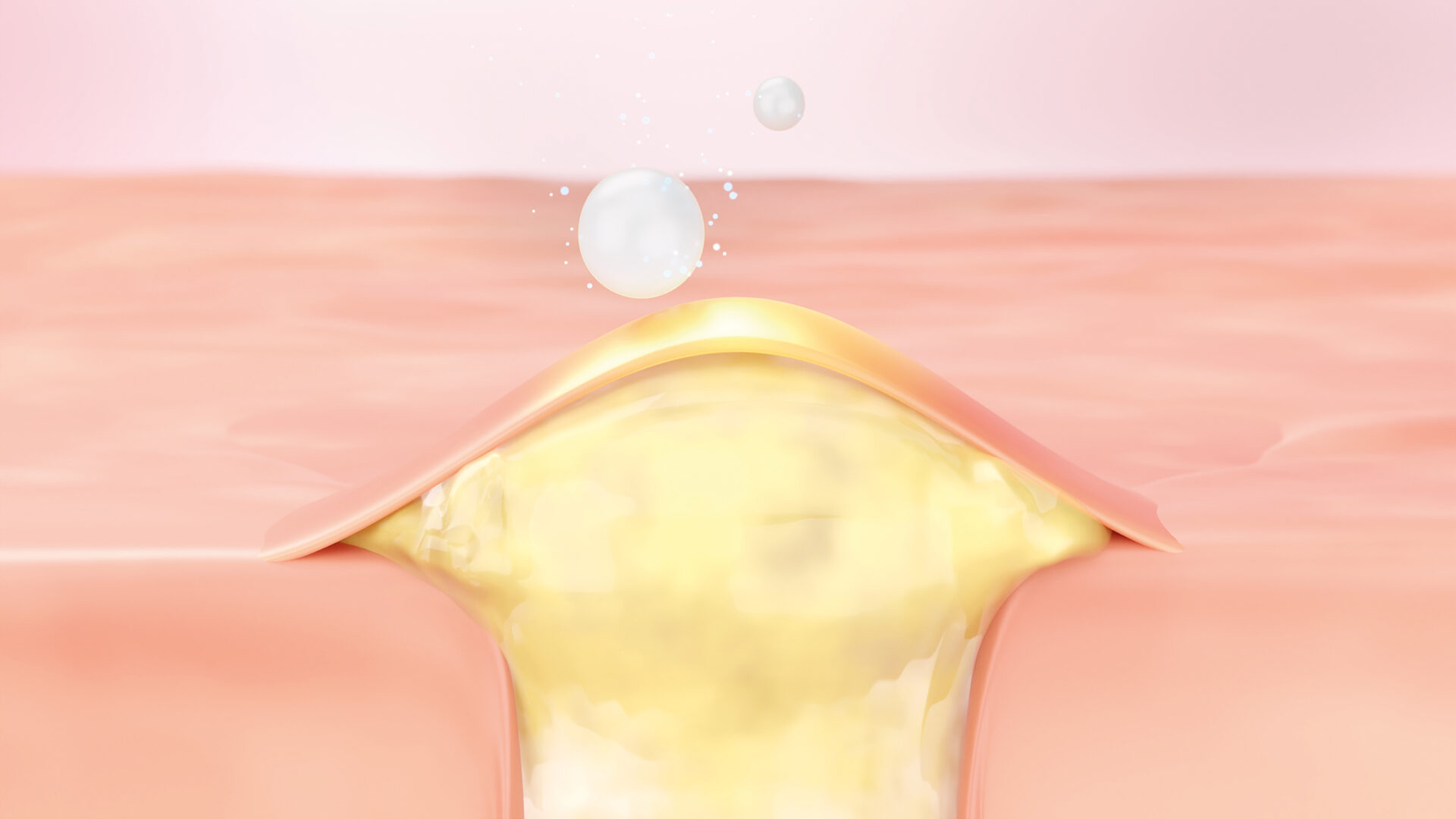
Acne is an inflammatory disease of the sebaceous follicles that primarily affects the face, chest and back [1]. The etiopathogenesis is multifactorial. It is now assumed that, in addition to genetic determinants, the following factors in particular are significantly involved: increased, partly androgen-dependent sebaceous gland stimulation and lipid synthesis as well as follicular hyperkeratosis, which leads to the formation of the primary lesion of the comedo [2]. The associated dysbiosis in the microbiome with Cutibacterium acnes, with varying degrees of inflammatory reaction, causes the development of papules, pustules and abscesses, such as in acne papulopustulosa and acne nodulocystica. As a therapeutic approach, a combination treatment with topical or systemic preparations directed against these processes is usually used and escalated depending on the severity [2].
Case 1: Acne papulopustulosa in a 29-year-old woman
Acne papulopustulosa is the most common subtype of acne vulgaris. It is a moderately severe, inflammatory form of acne characterized by comedones and inflammatory erythematous papules and pustules and has a significant impact on the quality of life of those affected. Acne papulopustulosa often affects the face and back.
At this year’s meeting of the German Dermatological Society (DDG), the case history of a 29-year-old female patient who presented to a teledermatology outpatient clinic in September 2021 with moderate to severe facial acne was presented [3].
Clinical findings and diagnosis: After analyzing the images taken by the patient herself, the findings revealed inflammatory erythematous papules and pustules as well as atrophic scars. After subsequent analysis of all the data collected, a diagnosis of acne papulopustulosa was made.
Course of therapy: Topical treatment was initially carried out with an individual formulation of benzoyl peroxide (BPO) 2.5% and clindamycin 1% for daily evening application. After three months, there was a slight reduction in inflammation and the therapy was switched to an individual formulation of tretinoin 0.0125%, clindamycin 1% and niacinamide 4% in carbomer gel. The tretinoin concentration was gradually increased during therapy and is currently 0.05%. The antibiotic clindamycin was removed from the individual prescription after six months of treatment and reintroduced after a three-month break. The patient is currently in her 13th month of treatment.
A significant reduction in papules and pustules as well as post-inflammatory hyperpigmentation was observed after just six months. Currently, only a few small blemishes are still visible and the patient is largely acne-free. Telemedical treatment proved to be a suitable form of therapy. Thanks to the close and regular monitoring of the course and side effects, the therapy could be optimally adapted and optimized to the dynamic development of the acne skin.
Case 2: Acne nodulocystica disseminata in a 47-year-old woman on dialysis
It is known that patients on dialysis can develop severe forms of acne. The pathogenesis is still largely unexplained, but toxic effects of hyperuricemia in chronic kidney failure (CNV) are being discussed. Similarly, hyperprolactinemia often associated with CNV can lead to lower estrogen and progesterone levels in women. This causes a relative androgen excess and stimulation of sebum production. Nodulocystic forms of acne usually respond poorly to conventional forms of therapy.
This patient case, which was also presented at the DDG conference, concerns a 47-year-old female patient on dialysis who presented at the University Clinic for Dermatology, Paracelsus Medical Private University in Nuremberg with disseminated nodular skin changes that had been present for six months [4].
Clinical findings and diagnosis: The patient with kidney disease reported that the skin lesions had started on the right flank with increasing spread to the rest of the integument and multiple abscesses. Apart from moderate itching, the patient was symptom-free. Due to terminal renal insufficiency with diabetic nephropathy, the patient has been on dialysis for a year. Clinically, plaques with a diameter of up to five centimeters and livid-erythematous, indurated, partly pustular nodules with comedones were found on the integument with emphasis on the lower extremity. In addition, hypopigmented atrophic-scarred areas were found in the surrounding area. The actual predilection sites of acne vulgaris were not, or only sparsely, affected. In summary of the clinical picture and all findings, acne nodulocystica disseminata was diagnosed in dialysis-dependent renal insufficiency.
Course of therapy: Systemic “low-dose” therapy with isotretinoin 20 mg (once daily) was initiated. This treatment proved to be efficient and safe. The follow-up showed a regression in the skin findings after just six weeks.
Literature:
- “Acne”, www.chemie.uni-hamburg.de/institute/bc/arbeitsgruppen/kerscher/patienten/akne.html,(last accessed 08/17/2023)
- “Acne vulgaris: New developments”, https://aerzte
zeitung.at/wp-content/uploads/2021/04/OAZ-Spezial-Dermatologie-2020.pdf, (last accessed 17.08.2023) - Manushkina L, Jureleviciute K: Telemedicine case report: Successful treatment of acne papulopustulosa. Poster, P056. DDG Conference, 26-29.04.2023.
- Sommer K, Krieter M, Mordstein V, Schultz E: Acne nodulocystica disseminata in end-stage renal disease and hemodialysis. Poster, P235, DDG Conference, 26-29.04.2023.
DERMATOLOGY PRACTICE 2023; 33(5): 27