Despite the introduction of disease-modulating pharmacological therapies, rehabilitative interventions continue to play an important role in the long-term management of MS. People with MS should be encouraged to engage in regular physical activity early in the course of the disease and instructed in an adapted exercise program. As the degree of disability increases, specific rehabilitative interventions and multidisciplinary rehabilitation phases are necessary.
Multiple sclerosis (MS) is a highly variable disease characterized by a wide spectrum of pathologies, multifocal lesions and functional deficits with complex disabilities. Disease-modulating drugs (beta-interferons, glatiramer acetate, natalizumab, fingolimod) can reduce inflammation and relapse frequency, improve clinical and subclinical course, and reduce tissue damage in relapsing-remitting MS [1–4]. However, in a recent, somewhat methodologically controversial study, the long-term effect of these disease-modulating therapies on clinical disease and disability progression was questioned [5]. Moreover, these treatments are ineffective in secondary progressive MS [6] without relapse superimposition and in primary progressive MS [7]. Since primary progressive MS is present in about 15% [6] and a large proportion of primary relapsing-remitting MS progresses to secondary progressive MS after 15-20 years [8], even today a large proportion of MS patients will develop complex functional disorders and disabilities in the long-term course, which can hardly be improved by drug therapies.
Symptomatic drug therapies are unfortunately only available for a limited range of symptoms (spasticity, bladder dysfunction, pain), while other common functional disorders (paralysis, ataxia, visual disturbances) have no effective pharmacological treatment options. In addition, the use of drug treatments is often limited by the occurrence of side effects. This means that MS sufferers face a long lifespan (median survival after diagnosis around 40 years) with increasing limitations in personal and social activities and quality of life [9, 10].
Thus, for these reasons, there continues to be an urgent need today for rehabilitative interventions and comprehensive multidisciplinary long-term management aimed at reducing the impact of the disease process on personal and social activities and enabling individuals to maximize their independence and quality of life in the context of MS [11].
What rehabilitative measures when?
Preservation of function and activity as an important goal in long-term treatment underscores the importance of evaluating rehabilitative interventions as early as possible in MS patients.
While at low levels of disability (EDSS. <3) Instruction and coaching to maintain and optimize physical performance (e.g., recommending physical activities and conducting independent individual training. [12]) are usually sufficient, MS patients with moderate disabilities (EDSS 3-5.5) should undergo specific assisted interventions to improve walking and daily living functions – this in combination with adapted strength-endurance training. For patients with higher disabilities (EDSS 6-7.5), regular specific therapy modalities combined with intensified multidisciplinary inpatient rehabilitation phases are recommended to maintain independence and mobility. In severely disabled, largely bedridden patients (EDSS 8-9.5), the main goal is to maintain mobility and mobilizability as well as to reduce the need for care and prevent complications (contractures, pressure sores, pain, respiratory problems): In addition to regular assisted therapies, caregiver counseling and instruction are particularly crucial in this phase. People with MS should be re-evaluated at regular intervals from the outset regarding the need to initiate or adapt rehabilitative measures.
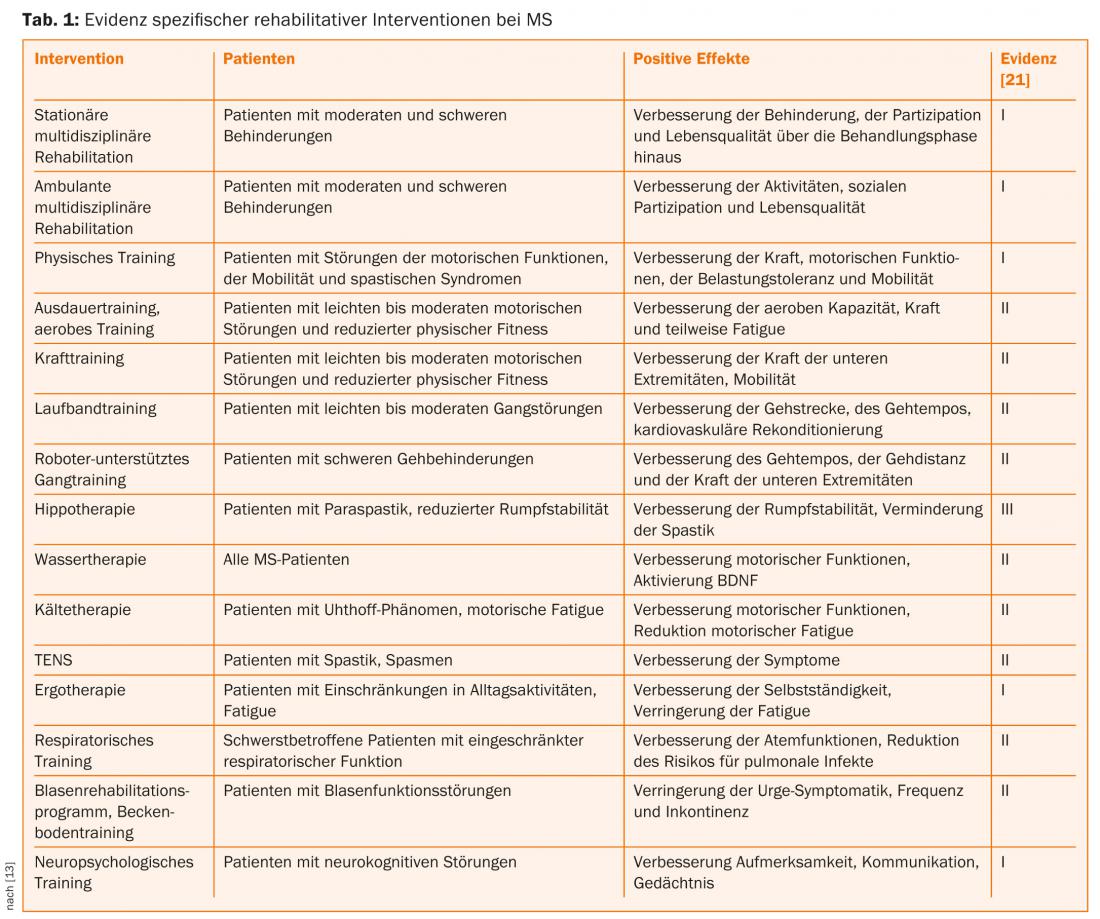
The decision to implement outpatient or inpatient rehabilitation measures depends on the degree and complexity of the disabilities as well as the individual objectives. In general, a multidisciplinary inpatient rehabilitation setting should be selected for MS patients with complex functional deficits and disabilities. An advantage of the inpatient treatment concept, besides the multidisciplinary organization and the high therapy intensity, is the focusing of the limited resources of MS patients on the therapies with regular rest periods, thus avoiding exhaustion by additional daily tasks [13]. On the other hand, outpatient or home-based therapies have the advantage that patients can carry out their training program in their familiar environment and this can take place in close cooperation with their caregivers [14]. However, the organization of outpatient multidisciplinary rehabilitation programs is often difficult in our country for logistical reasons due to the lack of availability of such specialized outpatient therapy centers. The place and evidence of specific rehabilitative interventions are summarized in Table 1.
On what mechanisms of action are rehabilitative measures based?
Functional studies indicate that continuous cortical reorganization occurs in MS patients, which allows affected individuals to compensate at least partially for multifocal lesions in an adaptive manner [15, 16]. Thus, one possible mechanism of action of rehabilitative interventions would be to promote such central adaptive processes. Another mechanism of action discussed on the basis of experimental data is a reduction in inflammatory activity through physical exercise [17, 18], although no definite effect on disease progression has yet been demonstrated in long-term studies. In addition to therapy-specific effects (specific activation, strength building, reconditioning), nonspecific effects (improved compensation, information, and instruction) also seem to play an important role [19].
Multidisciplinary long-term management
Due to the complexity and high variability of the disease, comprehensive long-term management should necessarily include the possibility of rehabilitative measures from the outset, in addition to pharmacological treatments. The focus of these interventions should not be solely on the timely adequate use of specific interventions, but should also include individual information and counseling of the affected persons and their relatives. In this context, all pharmacological and non-pharmacological measures should be combined in a goal-oriented long-term concept, which necessarily requires a coordinated multidisciplinary network. Due to the changes in the course of the disease, which are often difficult to predict, regular re-evaluation is necessary in order to adapt the interventions according to resources and needs by making appropriate adjustments to the treatment concept in the long-term course [11, 20].
Serafin Beer, MD
Literature:
- Sloka JS, Stefanelli M: Mult Scler 2005; 11: 425-432.
- Wingerchuk DM: Semin Neurol 2008; 28: 56-68.
- Bates D: Neurology 2011; 76: S14-S25.
- Freedman MS: Neurology 2011; 76: S26-S34.
- Shirani A, et al: JAMA 2012; 308: 247-256.
- Miller DH, Leary SM: Lancet Neurol 2007; 6: 903-912.
- La Mantia L, et al: Journal of neurology, neurosurgery, and psychiatry 2013; 84: 420-426.
- Hurwitz BJ: Neurology 2011; 76: S7-S13.
- Paltamaa J, et al: J Rehabil Med 2006; 38: 339-345.
- Pfleger CC, et al: Mult Scler 2010; 16: 121-126.
- Kesselring J, Beer S: Lancet Neurol 2005; 4: 643-652.
- McAuley E, et al: Mult Scler 2007; 13: 652-659.
- Beer S, Khan F, Kesselring J: Journal of neurology 2012; 259: 1994-2008.
- Khan F, et al: Mult Scler 2009; 15: 869-875.
- Rocca MA, et al: Ann Neurol 2002; 51: 330-339.
- Thickbroom GW, et al: J of Neurol 2008; 255: 1001-1005.
- Heesen C, et al: Expert Rev Neurother 2006; 6: 347-355.
- Bansi J, et al: Mult Scler 2013; 19: 613-621.
- Freeman JA, et al: Neurology 1999; 52: 50-56.
- Khan F, et al: Multidisciplinary rehabilitation for adults with multiple sclerosis. Cochrane Database Syst Rev 2011:CD006036.
- National Health and Medical Research Council (NHMRC). NHMRC Levels of Evidence and Grades for Recommendations for Developers of Guidelines NHMRC.
InFo Neurology & Psychiatry 2013; 11(6): 21-23.