Mammography and sonography are two important procedures for the differential diagnosis of a mammary nodule detected by palpation. Digital tomosynthesis can further reduce the number of false results.
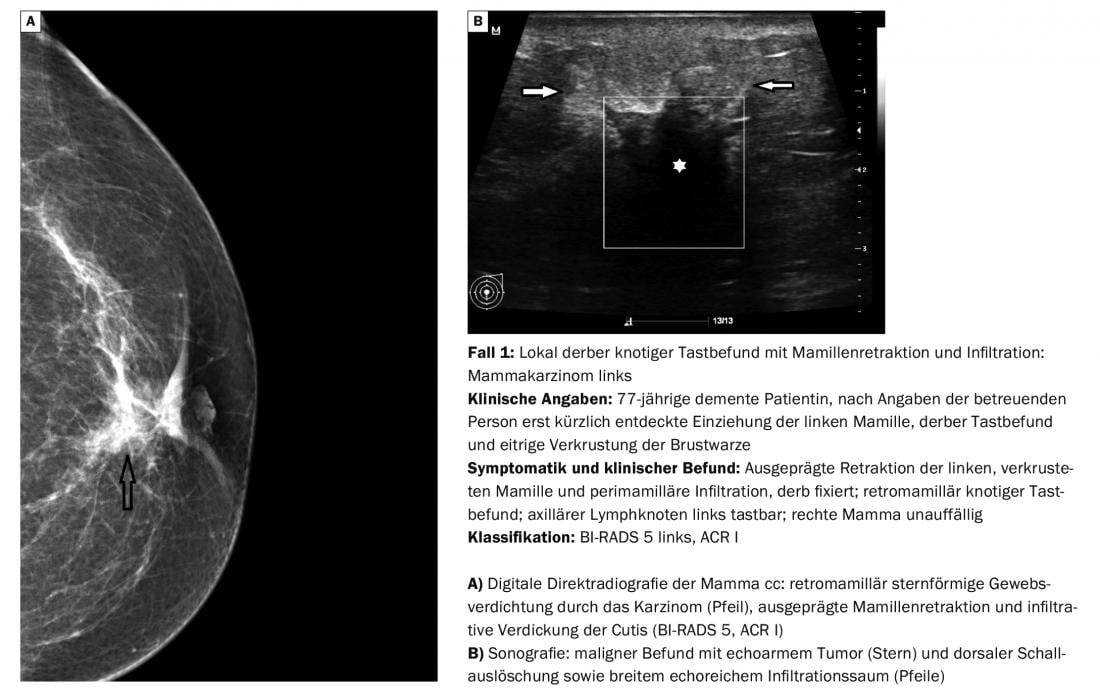
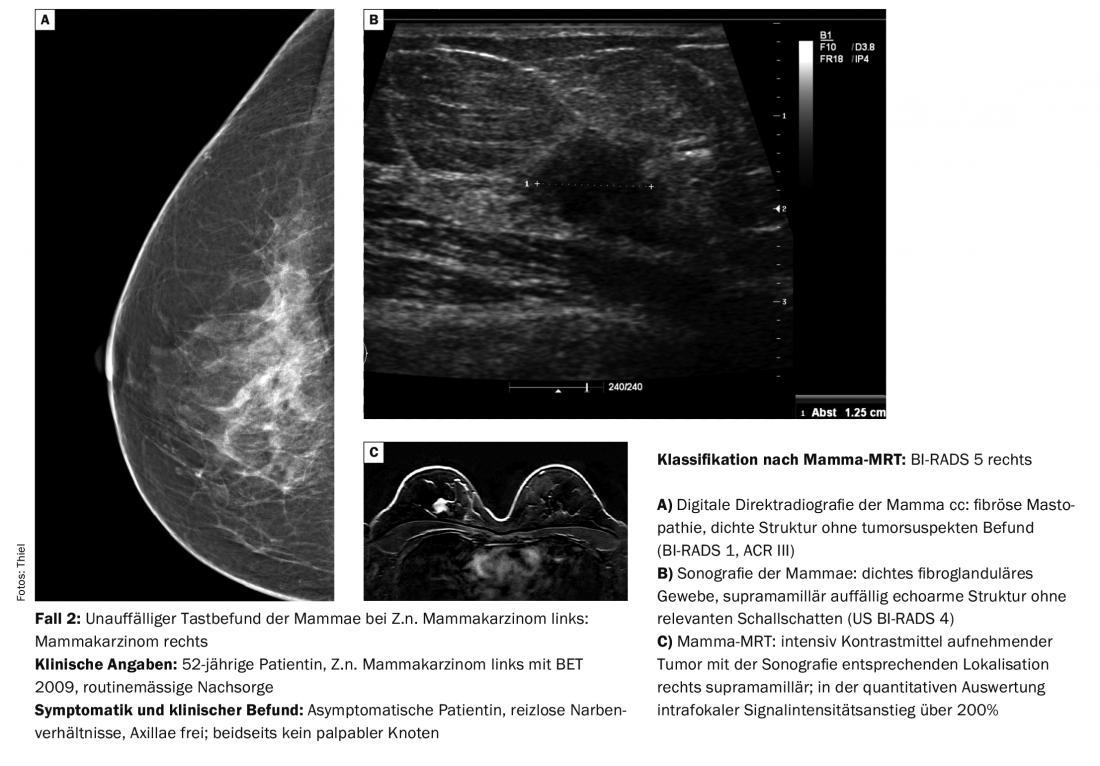
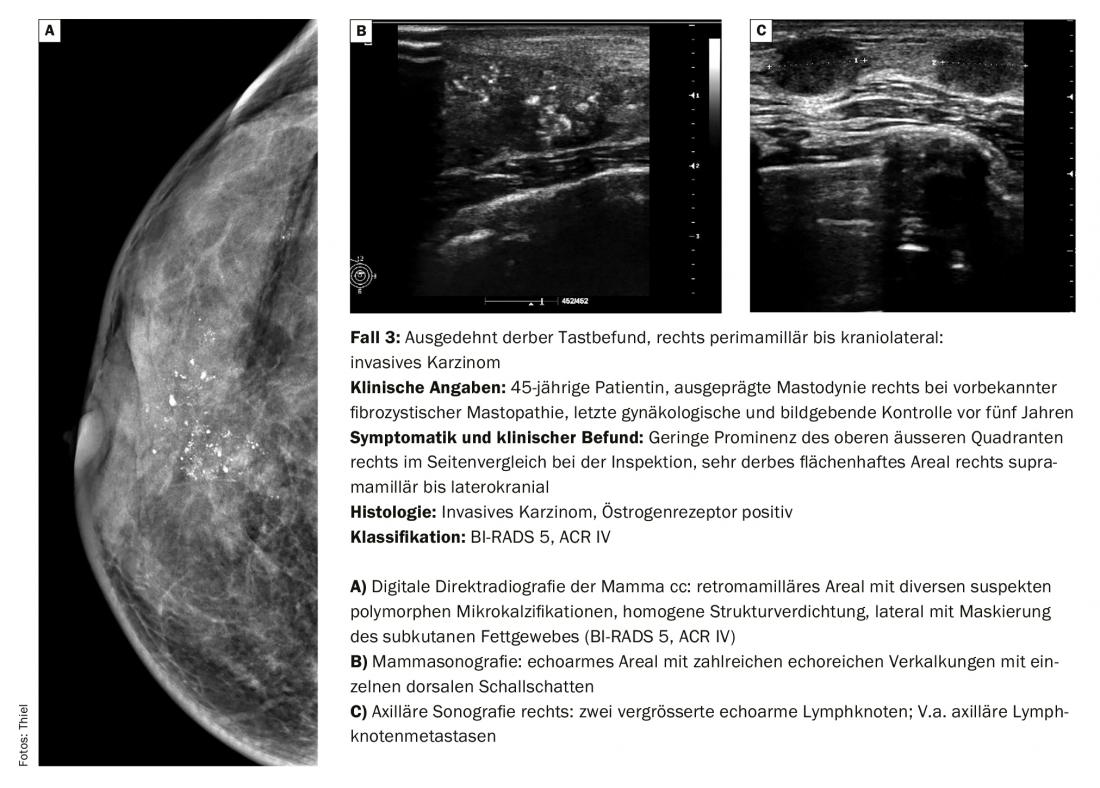
The differential diagnosis of palpated mammary nodules corresponds to benign changes such as fibroadenomas, cysts, fibrocystic mastopathies, and other less common changes in about 90%. However, carcinoma can be expected in about 10% of cases [1]. In these cases, the palpation findings are usually dermally nodular. Small findings may still be mobile, while larger tumors may be less mobile. However, not all malignancies are clinically conspicuous (case 2) or, in the case of dense mammary structure and suspicious palpation, can be clearly identified by mammography (case 3).
The American College of Radiology (ACR) standard for the Breast Imaging Reporting and Data System (BIRADS) and ACR classification is also applicable to malignancies.
Diagnostic imaging techniques
In addition to mammographic and sonographic imaging, digital tomosynthesis is on its way to being increasingly used. It can eliminate the undesirable masking of relevant findings by structural overlays and reduce the number of false positive and false negative results of image interpretation [2]. In principle, it can be stated that digital mammography now represents the diagnostic standard across the board and offers considerable advantages in postprocessing (zooming, inverting, measurements) in addition to monitor viewing of the images [3]. Breast MRI is used much more frequently in malignant changes and is a reliable tool in the differentiation of scar tissue and recurrent tumors – even in cases of discrepancy between clinic and mammogram on the one hand and sonography on the other (Case 2). The specific indications for the use of the method have already been described. However, breast MRI is also a technically very demanding diagnostic procedure and prone to errors; thus, motion artifacts and fat saturation errors must be avoided or taken into account during the evaluation [4].
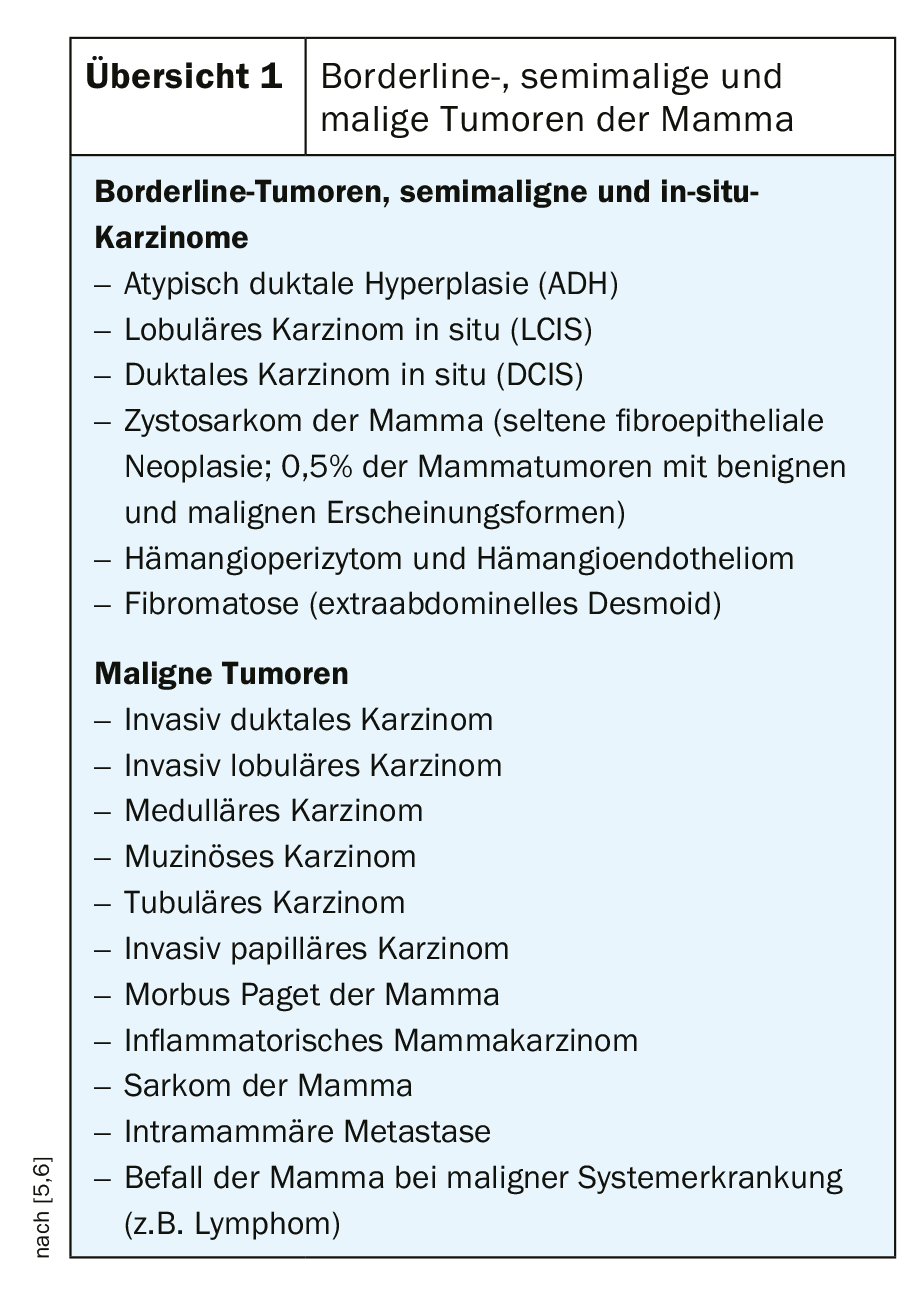
The different histologic types (overview) of borderline, semimalignant, and malignant tumors cannot always be differentiated by image morphology. The decisive factor is that they are recognized and the course is set for any further diagnostic or therapeutic procedures that may be required.
Important aspects of aftercare
Regular postoperative check-ups are important for early detection and treatment of local recurrences, local lymph node metastases or contralateral findings. Collegial collaboration between primary care physicians and gynecologists is critical to providing women with a seamless network of follow-up care, in which radiologists also play an important role. In the case of breast-conserving therapy, mammography and sonography with inclusion of the axillae are used in the imaging procedures; MRI occupies a separate position and is not part of standard follow-up. After ablation, careful examination of the chest wall scar is the domain of sonography after appropriate clinical examination. The insertion of silicone implants for cosmetic treatment after surgery of malignant breast findings regularly leads to a limitation of the assessability of the retroimplant region in mammography. Sonography and mammary MRI are then required in further detail. Diagnostic problems are caused by inflammatory breast carcinoma, which cannot be reliably differentiated from non-puerperal mastitis with all imaging techniques. Percutaneous punch or open biopsy are directional.
Take-Home Messages
- Numerous malignant changes can occur in the mamma.
- In most cases, diagnoses can be made after taking a history, clinical and imaging examination with mammography and sonography.
- As a very sensitive and specific procedure, breast MRI is used as a complementary method for special questions, especially to differentiate scar and recurrent tumor tissue and to exclude multifocal and contralateral tumors in dense mammae.
- Standardized classification of findings is performed according to BI-RADS and ACR.
Literature:
- Battista MJ, et al: Lumps in the breast. Diagnostics and differential diagnoses. Lege artis 2015; 5(1): 44-49.
- Schulz-Wendtland, Hermann KP, Bautz W: Digital mammography. Radiology up2date 2004; 4: 327-348.
- Schulz-Wendtland, Hermann KP, Uder M: Digital tomosynthesis of the breast. Radiology 2010; up2date 3: 195-202.
- Kurtz C: Update in breast MRI technique. Examination standards and quality assurance. Radiology up2date 2013; 2: 129-139.
- Fischer U, ed: X-ray mammography. Understanding, applying and optimizing. Stuttgart/New York: Georg Thieme Verlag, 2003: 132-209.
- Heywang-Köbrunner SH, Schreer I: Imaging breast diagnostics. Stuttgart/New York: Georg Thieme Verlag 1996: 217-286.
FAMILY PRACTICE 2019; 14(7): 33-35