At a training event held at EMPA, the Research and Service Institute for Materials Science and Technology Development of the ETH Domain, the question of how the situation of patients with chronic wounds can be improved in the future was discussed. This involved new types of gentle textiles and intelligent beds that register when a patient is bed sore.
(ag) 50 million people worldwide suffer from chronic wounds, e.g. due to malnutrition, diabetes or vascular diseases. First, Jürg Traber, MD, Director of the Bellevue Vein Clinic, Kreuzlingen, discussed the question of how a chronic wound is defined in the first place. Normally, a wound should heal after four to six weeks, after which any wound can become chronic. But are these periods set in stone? “Of course not, because no two wounds are alike. The size of the wound and the patient’s situation, e.g. bed confinement, must always be included in the assessment. Likewise, you have to ask yourself whether you are talking about a healing tendency or healing,” says Dr. Traber. Therefore, some researchers use the term chronic wound only after three months [1]. Even in guidelines, terminology must be viewed critically, including that of the Association of the Scientific Medical Societies (AWMF), where a chronic wound is defined by a lack of healing within eight weeks. First, the term “chronic wound” in this guideline refers only to venous, arterial and mixed ulcers and diabetic foot ulcers; second, too little attention is paid to the wound area.
Time parameters for successful wound healing can be found in week four: If the wound area of venous leg ulcers (VLU) has decreased by >40% by then, complete healing is likely after 24 weeks [2]. In “diabetic foot ulcers” (DFU), the same is true for a reduction of >50% and the probability of healing after 12 weeks [3].
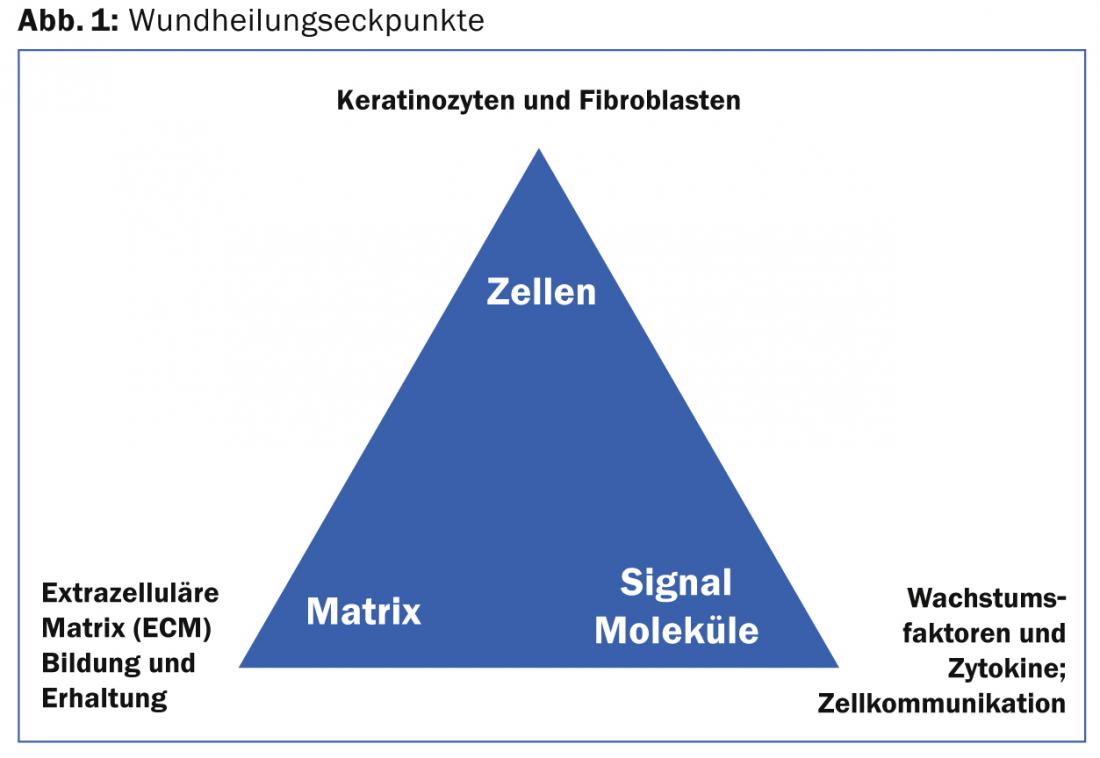
“A prerequisite for proper wound healing is an intact extracellular matrix,” Dr. Traber explained. The degradation of the extracellular matrix is carried out by so-called matrix metalloproteases (MMP). This process is inhibited by TIMPs (“tissue inhibitors of metalloproteinases”). If these are missing, an imbalance of the MMPs occurs and the interaction of successful wound healing is disturbed. The wound healing corner points are summarized in Figure 1.
Wound dressings
Modern wound dressings aim to absorb in wet wounds. This is done according to Maria Signer, dipl. Wound expert SAfW/Hplus, using alginate, hydrofiber, hydropolymer foam, (super)absorber or negative pressure therapy. For dry wounds, the therapeutic goal was to rehydrate using hydrogel, films, hydrocolloids, and hydrogel in combination with fatty gauze. And moist wounds should be preserved using alginate, hydrogel, hydrocolloids, films and hydropolymer foam. An innovative treatment approach is tissue engineering, an umbrella term for the artificial production of biological tissue by culturing cells (e.g. EpiDex®) to replace or regenerate diseased or missing tissue in a patient. Wound healing is stimulated by the release of active substances (growth factors).
How can a pressure sore be prevented?
New bed sheets: According to Dr. med. Anke Scheel, Swiss Paraplegic Center, Nottwil, pressure ulcer prevention through new bed sheets is still a long way from becoming a reality, but the goal has recently been approached significantly. “Paraplegics have a 30 to 50 percent risk of developing pressure ulcers, usually in the sacral region. Blood flow and recapilarization are altered in paraplegics,” Dr. Scheel said. Since shear forces and friction are thought to be partly responsible for the development of superficial and deep pressure sores, research is currently being conducted into new bed sheets whose structure has free spaces and thus fewer contact points with the skin. This causes less friction. In addition, they can absorb perspiration via evaporation and suspension and reduce capillary adhesion. “In a prospective, randomized intervention study at the Swiss Paraplegic Center Nottwil, they compared the new bed sheet to conventional hospital textiles in terms of skin hydration, redness, elasticity and blood flow,” Dr. Scheel explained. Patients lay with bare skin for five nights each on each textile. The result of the study was that redness was on average 2% lower and moisture was 5% lower. Blood flow was 6% higher, elasticity remained the same. While these results did not reach significance, there was a statistically significant increase in subjective well-being (p=0.044). Sweating (p=0.024) and wrinkling (p=0.014) also reduced, which suggests that extending the indication to other skin conditions or using the fabric in undergarments or as an incontinence pad would be reasonable.
Smart beds: Normally, the sleeping person moves involuntarily when pressure is applied, because of the disturbing ischemic pain. This process is disrupted in people with mobility impairments or cognitive deficits. An innovation from EMPA/ETH now gives their beds “intelligence” (Mobility Monitor): A sensor plate, which can be placed under each mattress, detects when and how often a patient shifts (physiological sleep profile). If there is a threat of the patient resting for too long (defined in advance), this is communicated to the nurses by the system, who can then reposition the patient in a targeted manner. According to Dr. Michael Sauter, the inventor of the technology, this prevents unnecessary stock transfers.
Data from an application observation show that the monitor saved 41% of planned transfers. The whole process becomes more efficient, you save time and personnel, the lack of which is one of the biggest challenges in today’s care. “With the help of this information, decisions can be made fact-based and unexpected risks can be identified in time. You can do the right thing at the right time, avoid complications and discharge or transfer patients earlier. Of course, the system does not replace people, but it serves as an important support,” says Dr. Sauter.

New approach to wound treatment
Prof. Dr. med. vet. Brigitte von Rechenberg from the Center for Applied Biotechnology and Molecular Medicine (CABMM) at the University of Zurich concluded by discussing QuickSana®. This is a phytotherapeutic agent that has been used in animals in Switzerland for years. It consists of hops and wormwood, trace elements and minerals. “Hops have an antibacterial and anti-inflammatory effect. In the first phase, the medication is used to rinse (cleanse) the wound, and in the second phase, a protective film is created by means of cream to seal the wound,” says Prof. von Rechenberg. In addition to in vitro tests with cell cultures, the drug was investigated in rats. With success as it turned out: Compared to Betadine® and chlorhexidine and, of course, with the control group, QuickSana caused® reduced wound contraction and accelerated epithelialization on day 7, and thicker epithelium and better cosmesis on day 28. According to Prof. von Rechenberg, the drug in this form thus offers a new approach to wound treatment (but one that has long been known in terms of the active ingredients), but so far only for animals.
Source: On the pulse: chronic wound management today and tomorrow. Technology Briefing of Empa, April 28, 2014, St. Gallen
- Dissemond J: When is a wound chronic? Dermatologist 2006; 57: 55.
- Gelfand JM, Hoffstad O, Margolis DJ: Surrogate endpoints for the treatment of venous leg ulcers. J Invest Dermatol 2002 Dec; 119(6): 1420-1425.
- Sheehan P, et al: Percent change in wound area of diabetic foot ulcers over a 4-week period is a robust predictor of complete healing in a 12-week prospective trial. Diabetes Care 2003 Jun; 26(6): 1879-1882.
DERMATOLOGIE PRAXIS 2014; 24(3): 41-43











